Abstract
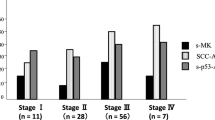
Introduction: Recent investigations indicate that in 50% of patients with gastric cancer, β-hCG-posiitive cells can be found in the tumour by immunohistochemical investigations. The objective of this study was to investigate how often β-hCG-immunoreactive gastric carcinomas were accompanied by an elevation in serum β-hCG, that could have been used as a course control variable. Methods: In 54 patients with gastric carcinoma a monoclonal antibody directed against β-hCG was used for immunohistochemical marking in the APAAP system. The evaluation was graded positive or negative. In parallel, serum β-hCG was determined preoperatively using an enzyme immunoassay (MEIA). Tumour stage, grading and tumour locallization were determinants in the evaluation. Results: We found that 41% (22 of 54) of the carcinomas induced a :positive immunohistochemical response to β-hCG, regardless of their location in the stomach. In relation to tumour stage, a positive β-hCG immunoreactivity was apparent in 27% (6/22) of tumours without lymph node or distant metastases (TI -4N0M0), in 54% (7/13) of tumours with lymph node and without distant metastases (T1−4N≥1 M0) and in 47% (9/35) of tumours with distant metastases. Poorly differentiated tumours (G3–4) were positive in 42% (15/36) and well-differentiated tumors (G1–2) in 39% (7/18) of cases. In only 1 patient was the β-hCG, level in serum elevated, however. Conclusions: β-hCG-Positive gastric carcinomas are found more frequently in advanced tumour stages and poorly differentiated carcinomas. These carcinomas, however, seem not to excrete β-hCG in sufficient amounts to produce measurable serum values. Therefore, β-hCG cannot be used a prognostic factor or for course control. The relevance of β-hCG expression of tumour cells to the patients' prognosis remains obscure.
Zusammenfassung
Einleitung: Nach neueren Untersuchungen ist davon auszugehen, daß bei des Hälfte von Patienten mit einem Magenkarzinom β-hCG-positive Zellen im Tumor immunhistochemisch gefunden werden können. Ziel war daher, systematisch zu untersuchen, inwieweit β-hCG-immunreaktive Magenkarzinome von einem Anstieg des Serum-β-hCG begleitet werden and dieses damit als Verlaufsparameter zur Verfügung steht. Methode: Bei 54 Patienten mit einem Magenkarzinom wurde zur immunhistochemischen Darstellung ein gegen β-hCG gerichteter monoklonaler Antikörper (Fa. Sigma, 1:100) im APAAP-System verwendet. Die Auswertung wurde nach positiver and negatives Reaktion graduiert. Parallel wurde im Serum des Patienten β-hCG präoperativ mit einem Enzymimmunoassay (MEIA, Fa. Abbot) bestimmt. Tumor-stadium, Grading and Tumor-lokalisation werden in die Auswertung mit einbezogen. Ergebnisse: Es wird bestätigt, daß 41% (22 von 54) des Karzinome, unabhängig von ihrer Lokalisation im Magen, eine positive immunhistochemische Reaktion gegen β-hCG auslösen. Es zeigte sich in Abhängigkeit vom Tumorstadium eine positive β-hCG-Immunreaktivität in 27% (6 von 22) des Tumoren ohne Lymphknoten- and Fernmetastasierung (T1–4 N0 M0), in 54% (7 von 13) des Tumoren mit Lymphknotenaber ohne Fernmetastasen (T1–4 N≥1 M0) und in 47% (9 von 35) des Tumoren mit Fernmetastasierung. Schlecht differenzierte Tumoren (G3–4) waren zu 42% (15 von 36) und gut differenzierte Tumoren (G1–2) nur zu 39% (7 von 18) positiv. Aber lediglich bei einer Patientin war der β-hCG-Spiegel im Serum erhöht. Zusammenfassung: Immunhistochemisch β-hCG-positive Magenkarzinome werden vermehrt bei fortgeschrittenem Tumorstadium und Schlecht differenzierten Karzinomen gefunden. Diese Kar zinome scheinen aber nicht in ausreichender Menge β-hCG ins Serum abzugeben, was zu serologisch meßbar erhöh-ten Werten führt. β-hCG im Serum kann daher nicht als Prognosefaktor bzw. zur Verlaufskontrolle herangezogen werden. Abzuwarten bleibt, inwieweit die β-hCG-Expression von Tumorzellen u. U. Einfluß auf die Propose der Patienten besitzt.
Similar content being viewed by others
Literatur
Akar AH, Gervasi G, Blacker C, Wehmann RE, Blithe DL, Nisula BC (1990) Human chorionic gonadotrophin-like and β-core-like materials in postmenopausal urin. J Endocrinol 125:477–484
Bellet D, Arrang JM, Contesso G, Caillaud JM, Bohoun C (1980) Localization of the β subunit of human chorionic gonadotropin on various tumors. Eur J Cancer 16:433–439
Blackman MR, Weintraub BD, Rosen SW (1980) Human placetal and pituitary glycoprotein hormones and their subunits as tumor markers: a quantitative assessment. J Natl Cancer Inst 65:81–93
Braunstein GD, Vaitukaites JL, Carbone PP, Ross GT (1973) Ectopic production of human chorionic gonadotropin by neoplasms. Ann Intern Med 78:39–45
Buckley CH, Fox H (1979) An immunohistochemical study of the significance of HCG secretion by large bowel adenocarcinomata. J Clin Pathol 32:368–372
Cordell JL, Falini B, Erber WN, Ghosh AK, Abdulaziz Z, Macdonald St, Pulford KAF, Stein H, Mason DY (1984) Immunoencymatic labeling of monoclonal antibodies using immune complexes of alkaline phosphatase and monoclonal anti-alkaline phosphatase (APAAP complexes). J Histochem Cytochem 32: 219–229
Dericks-Tan JSE, Taubert HD (1993) Fallacious hCGβ in patients with choriocarcinoma. Lab Med 17:559–565
Fairman C, Colwell JA, Ryan RJ (1967) Gonadotropin secretion from a bronchiogenic carcinoma. N Engl J Med 275: 1395–1399
Fukayama M, Hayashi Y, Koike M (1987) Human chorionic gonadotropin in gastric carcinoma. An immunohistochemical study suggesting independent regulation of subunits. Virchows Arch 411:205–212
Hattori M, Fukase M, Yoshimi H, Matsukura S, Imura H (1978) Ectopic production of human chorionic gonadotropin in malignant tumors. Cancer 42:2328–2333
Hermanek P, Sobin LH (1992) UICC TNM classification of malignant tumours, 4th edn, 2nd rev. Springer, Berlin Heidelberg New York Toyko
Inaba N, Renk T, Wurster K, Rapp W, Bohn H (1980) Ectopic synthesis of pregnancy specific β1, glycoprotein (SP1) and placental specific tissue proteins (PP5, PP10, PP12) in nontrophoblastic malignant tumors: possible markers in oncology. Klin Wochenschr 58:789–791
Kodama T, Kameya T, Hirota T, Shimosato Y, Ohkura H, Mukojima T, Kitaoka H (1981) Production of alpha-fetoprotein, normal serum proteins, and human chorionic gonadotropin in stomach cancer: histologic and immunohistochemical analyses of 35 cases. Cancer 48:1647–1655
Manabe T, Adachi M, Hirao K (1985) Human chorionic gonadotropin in normal, inflammatory, and carcinomatous gastric tissue. Gastroenterology 89:1319–1325
Nishimura R, Kitajima T, Hasegawa K, Takeuchi K, Mochizuki M (1989) Molecular forms of human chorionic gonadotropin in choriocarcinoma serum and urin. Jpn J Cancer Res 80:968–974
O'Reilly SM, Rustin GJS (1993) Mismanagement of choriocarcinoma due to a false how hCG measurement. Int J Gynecol Cancer 3:186–188
Ozturk M, Bellet D, Manil L, Hennen G, Frydman R, Wands J (1987) Physiological studies of human chorionic gonadotropin (hCG), ahCG, and βhCG as measured by specific monoclonal immunoradiometric assays. Endocrinology 120:549–558
Pierce JG, Parsons TF (1981) Glycoprotein hormones: structures and function. Ann Rev Biochem 50:465–495
Remaley AT, Senior MB, Goodman DBP (1989) Discordant hCG measurements in a patient with a carcinoma. Clin Chem 35: 1259- 1261
Thomas TM,Morgan DB, Swaminathan R (1978) Severe hyponatremia. Lancet 1:621–624
Tomita K, Kuwajima M (1981) Chorionic gonadotropin in gastric cancer tissue, especially its relation to patients prognosis. Jpn J Cancer Clin 27:1281–1282
Vaitukaites JL, Ross GT, Braunstein GD, Rayford PL (1977) Gonadotropins and their subunits: basic and clinical studies. Recent Prog Horm Res 32:289–321
Wheeler CA, Davis S, Degefu S, Thorneycroft IH, O'Quinn AG (1990) Ovarian choriocarcinoma: a difficult diagnosis of an unusual tumor and a review of the hook effect. Obstet Gynecol 75:547–549
Wittekind Ch, Wachner R, Henke W (1986) Localization of CEA, HCG, isozyme, alpha- 1-antitrypsin, and alpha-1-antichy-motrypsin in gastric cancer and prognosis. Virchows Arch 409:715–724
Yakeishi Y, Mori M, Enjoji M (1990) Distribution of β-human chorionic gonadotropin-positive cells in noncancerous gastric mucosa and in malignant gastric tumors. Cancer 66: 695–701
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rau, B., Below, C., Haensch, W. et al. Zur Bedeutung von β-hCG im serum als tumormarker fur das magenkarzinom. Langenbecks Arch Chir 380, 359–364 (1995). https://doi.org/10.1007/BF00207226
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF00207226