Abstract
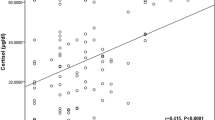
A prospective randomised study was performed on 25 children aged 1.4 to 15.8 years with severe head injury (Glasgow Coma Scale⪕7) to determine the clinical effectiveness and the impact on endogenous cortisol production of high-dose steroid therapy. Thirteen patients (group 1) received dexamethasone 1 mg/kg/day during the first 3 days and 12 (group 2) not. All patients were treated with a standardized regimen. Urinary free cortisol was measured by radioimmunoassay, and the clinical data were recorded at hourly intervals. Outcome was assessed 6 months later using the Glasgow Outcome Scale. We found a higher frequency of bacterial pneumonias in the dexamethasone-treated patients (7/13 versus 2/12). Group 1 showed a suppression of endogenous cortisol production from day 1 to day 6. In group 2, menu free cortisol was up to 5-fold higher than under basal conditions. The results in group 2 showed taht the endogenous steroid production reacts adequately to the stress of severe head injury. It probably is sufficient to elicit maximum glucocorticoid effects. There was no other statistically significant difference in the clinical and laboratory data between the two groups. We conclude that dexamethasone in high doses suppresses endogenous cortisol production up to 6 days and may increase the risk of bacterial infection without affecting the outcome or the clinical and laboratory data.
Similar content being viewed by others
References
Miller JD, Leech P (1975) Effects of mannitol and steroid therapy on intracranial volume-pressure relationships in patients. J Neurosurg 42:274
Becks JWF, Bosch DA, Brock M (1976) Treatment of acute cerebral edema with high dose of dexamethasone. Intracranial pressure III. Springer, Berlin Heidelberg New York, pp 231–235
Gudeman SK, Miller JD, Becker DP (1979) Failure of high-dose steroid therapy to influence intracranial pressure in patients with severe head injury. J Neurosurg 51:301
Cooper PR, Moody S, Clark WK, Kirkpatrick J, Maravilla K, Gould AL, Drane W (1979) Dexamethasone and severe head injury: a prospective double-blind study. J Neurosurg 51:307
Saul TG, Ducker TB, Salcman M, Carro E (1981) Steroids in severe head injury: a prospective randomized clinical trial. J Neurosurg 54:596
Braakman R, Schouten HJA, Blaauw-van Dyshoeck M, Minderhoud JM (1983) Megadose steroids in severe head injury: results of a prospective double-blind clinical trial. J Neurosurg 58:326
Dearden NM, Gibson JS, Mcdowall DG, Gibson RM, Cameron MM (1986) Effect of high-dose dexamethasone on outcome from severe head injury. J Neurosurg 64:81
Galicich JH, French LA (1961) Use of dexamethasone in the treatment of cerebral edema resulting from brain tumors and brain surgery. Am Pract Dig Treat 12:169
Stolecke H (1970) The determination of free urinary cortisol: a modification of the method described by Gerdes and Staib and normal values in infants. Horm Metab Res 2:298
Deutschman CS, Konstantinides FN, Raup S, Cerra FB (1986) Steroids potentiate hypermetabolism and acquired malnutrition in isolated closed-head injury. Crit Care Med 14:336
Piek J, Lumenta CB, Bock WJ (1985) Protein and amino acid metabolism after severe cerebral trauma. Intensive Care Med 11:192
Braun SR, Levin AB, Clark KL (1986) Role of corticosteroids in the development of pneumonia in mechanically ventilated head-trauma victims. Crit Care Med 14:198
DeMaria EJ, Reichman W, Kenney PR, Armitage JM, Gann DS (1985) Septic complications of corticosteroid administration after central nervous system trauma. Ann Surg 202:248
Zachmann M, Fanconi A, Prader A (1974) Plasma cortisol in children with fulminating meningococcal infection. Helv Paediat Acta 29:245
Brandt M, Dorsic D, Herter T, Hidding J (1983) The effects of dexamethasone on surgical stress in neuro-surgical patients assessed by the measurement of hormone levels LH, FSH, GH, ACTH, cortisol and testosterone. Intracranial pressure V. Springer, Berlin Heidelberg New York, pp 777–783
Gabrielsen J, Bendtsen A, Eriksen H, Andersen S (1985) Methylprednisolone half-life during simultaneous barbiturate treatment and mechanical hyperventilation of neurosurgical patients. J Neurosurg 62:182
Andrassy RJ, Dubois T (1985) Modified injury severity scale and concurrent steroid therapy: independent correlates of negative nitrogen balance in pediatric trauma. J Pediat Surg 20:799
Clifton GL, Robertson CS, Grossman RG, Hodge S, Foltz R, Garza C (1984) The metabolic response to severe head injury. J Neurosurg 60:687
Goris RJA, Draaisma J (1982) Causes of death after blunt trauma. J Trauma 22 (2):141
Baker CJ, Oppenheimer L, Stephens B (1980) Epidemiology of trauma deaths. Am J Surg 140:144
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fanconi, S., Klöti, J., Meuli, M. et al. Dexamethasone therapy and endogenous cortisol production in severe pediatric head injury. Intensive Care Med 14, 163–166 (1988). https://doi.org/10.1007/BF00257471
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00257471