Summary
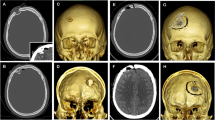
A follow-up study is presented of the initial neurosurgical treatment of 20 patients who sustained penetrating eraniocerebral injuries during “Operation Desert Storm”. Fifteen of these patients had received intracranial debridement through a craniectomy and five patients had received care of scalp wounds only. Following treatment and stabilisation in a frontline hospital, these patients were transferred to the Riyadh Armed Forces Hospital for further evaluation and management.
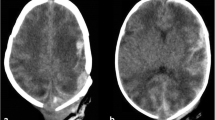
On admission, all the patients received a computerised tomographic scan which revealed shrapnel fragments inside their brain. No attempt had been made to remove the metal fragments. A patient with an infected scalp wound was treated with a course of appropriate antibiotics and the wound dressed. Dexamethasone was not used. Anticonvulsants were used only in one patient who had been treated for a presumed cerebral abscess.
The neurological status of the patients improved along with the reduction of oedema and the swelling of the brain as shown in the follow-up CT scans. No patient died or developed a seizure disorder.
These results suggest that re-operation for removal of retained fragments is unnecessary. It is concluded that the initial treatment of shrapnel wounds of the brain should be to preserve maximal cerebral tissue and function either by limiting the wound debridement performed through a craniectomy or by care of scalp wounds only.
Similar content being viewed by others
References
Aarabi B (1987) Comparative study of bacteriological contamination between primary and secondary exploration of missile head wounds. Neurosurgery 20: 610–616
Aarabi B (1989) Causes of infections in penetrating head wounds in the Iran-Iraq war. Neurosurgery 25: 923–926
Aarabi B (1990) Surgical outcome in 435 patients who sustained missile head wounds during the Iran-Iraq war. Neurosurgery 27: 692–695
Ameen AA (1984) The management of acute craniocerebral injuries caused by missiles: analysis of 110 consecutive penetrating wounds of the brain from Basrah. Injury 16: 88–90
Arendall REH, Meirowsky AM (1983) Air sinus wounds: an analysis of 163 consecutive cases incurred in the Korean War 1950–52. Neurosurgery 13: 377–380
Bakay L (1984) The value of CT scan in gunshot injuries to the brain. Acta Neurochir (Wien) 71: 189–204
Barnett JC, Meirowsky AM (1955) Intracranial hematomas associated with penetrating wounds of the brain. J Neurosurg 12: 34–38
Bashir EM, Choudhury AR, Cybulski GR, Al Moutaery KR (1992) Management of penetrating cranio-cerebral gunshot injuries in civilians. Saudi Medical Journal 13: 170–171
Brandvold B, Levi L, Feinrod M, George ED (1990) Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict, 1982–1985: analysis of a less aggressive surgical approach. J Neurosurg 72: 15–21
Carey ME, Young HF, Mathis JL (1972) The neurosurgical treatment of craniocerebral missile wounds in Vietnam. Surg Gynecol Obstet 135: 386–390
Carey ME, Sacco W, Merkler J (1982) An analysis of fatal and non-fatal head wounds incurred during combat in Vietnam by U.S. forces. Acta Chir Scand [Suppl] 508: 351–356
Clark WC, Muhlbauer MS, Watridge CB,et al (1986) Analysis of 76 civilian craniocerebral gunshot wounds. J Neurosurg 65: 9–14
Grahm TW, Williams FC Jr, Harrington T,et al (1990) Civilian gunshot wounds to the head: a prospective study. Neurosurgery 27: 696–699
Gurgian ES (1974) The treatment of penetrating wounds of the brain sustained in warfare: a historical review. J Neurosurg 39: 157–167
Hammon WM (1971) Analysis of 2187 consecutive penetrating wounds of the brain from Vietnam. J Neurosurg 34: 127–131
Jennet B, Bond M (1975) Assessment of outcome after severe brain damage. A practical scale. Lancet 1: 480–484
Mathews WE (1972) The early treatment of craniocerebral missile injuries; experience with 92 cases. J Trauma 12: 939–954
Myers PW, Brophy J, Salazar AM,et al (1989) Retained bone fragments after penetrating brain wound: long-term follow-up in Vietnam veterans. J Neurosurg 70: 319 A (abstract)
Rappaport ZH, Sahar A, Shaked I,et al (1984) Computerised tomography in combat-related craniocerebral penetrating missile injuries. Br J Med Sci 20: 668–671
Salazar AM, Jabbari B, Vance SC,et al (1985) Epilepsy after penetrating head injury. I: Clinical correlates: a report of the Vietnam Head Injury Study. Neurology 35: 1406–1414
Shoung HM, Sichez JP, Pertuiset B (1985) The early prognosis of craniocerebral gunshot wounds in civilian practice as an aid to the choice of treatment. A series of 56 cases studied by computerised tomography. Acta Neurochir (Wien) 74: 27–30
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Chaudhri, K.A., Choudhury, A.R., Al Moutaery, K.R. et al. Penetrating craniocerebral shrapnel injuries during “Operation Desert Storm”: Early results of a conservative surgical treatment. Acta neurochir 126, 120–123 (1994). https://doi.org/10.1007/BF01476420
Issue Date:
DOI: https://doi.org/10.1007/BF01476420