Abstract
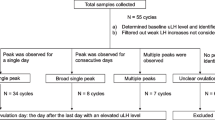
A prospective study of the reliability of the CUE Fertility Monitor to identify the fertile time of the menstrual cycle was conducted. The device provides a digital measurement of the electrical resistance of saliva (SER) and vaginal secretions (VL). The readings of the device were compared with the fertile time detected by ultrasonography of the growing follicle and estimation of the LH surge to detect ovulation. Thirteen women participated in the study. Sixteen cycles contained both signals (SER, VL) for the beginning and the end of the fertile period. In 2 cycles a CUE signal could not be found by the device.
Using a computerized algorithm for evaluation of the CUE signals, the beginning of the fertile period was accurately detected in 14 cycles; in 2 cycles the signal was found less than five days prior to ovulation.
The last day of fertility was identified correctly by the CUE Fertility Monitor in 10 cycles; in 6 it was incorrectly identified during the time when the woman was still fertile. This suggests that the CUE Fertility Monitor utilizing the algorithm on which it currently is based cannot be recommended for natural family planning. However, we think that the algorithm for evaluation should be improved as useful signals in the menstrual cycle are detected.
Resumé
Une étude prospective a été menée sur la fiabilité du “contrôleur de fécondité CUE” permettant de cerner la période de fécondité du cycle menstruel. Ce dispositif affiche une mesure numérique de la résistance électrique de la salive (RES) et des sécrétions vaginales (SV). Les mesures indiquées sur le dispositif sont comparées aux périodes de fécondité décelées par l'échographie des follicules en développement et l'estimation de la LH libérée pour détecter l'ovulation. Treize femmes ont pris part à cette étude. Seize cycles ont fait apparaître les deux signes (RES, SV) correspondant au début et à la fin de la période de fécondité. Dans 2 cycles, le dispositif n'a pas décelé de signes CUE.
A l'aide d'un algorithme informatisé pour l'évaluation des signes CUE, le début de la période de fécondité a été décelé avec exactitude dans 14 cycles; dans 2 cas, le signe est apparu moins de 5 jours avant l'ovulation.
Le contrôleur de fécondité CUE a fait apparaître le dernier jour de fécondité, correctement dans 10 cycles, mais incorrectement dans 6 cycles alors que la femme était encore en période de fécondité. Ces résultats laissent à penser que le contrôleur de fécondité CUE utilisant l'algorithme sur lequel il est actuellement fondé, ne peut être recommandé pour le planning familial naturel. Nous pensons cependant que cet algorithme d'évaluation devrait être amélioré car il permet de détecter des signes utiles au cours du cycle menstruel.
Resumen
Se realizó un estudio prospectivo de la fiabilidad del Monitor de Fertilidad CUE para identificar el período fértil del ciclo menstrual. Este dispositivo proporciona una medición digital de la resistencia eléctrica de la saliva (SER) y de las secreciones vaginales (VL). Las mediciones del dispositivo se compararon con el período de fertilidad detectado por ecograía del folículo en crecimiento y la estimación del aumento de la HL a fin de detectar la ovulación. Trece mujeres participaron en el estudio. Dieciséis ciclos contenían ambas señales (SER, VL) en lo relativo al comienzo y fin del período fértil. En 2 ciclos, el dispositivo no pudo detectar ninguna señal CUE.
Utilizando un algoritmo computadorizado para evaluar las señales CUE, el comienzo del período fértil fue detectado con precisión en 14 ciclos; en 2 ciclos, la señal fue detectada menos de cinco días antes de la ovulación.
El último día de la fertilidad fue identificado correctamente por el Monitor de la Fertilidad CUE en 10 ciclos, y en 6 fue identificado incorrectamente durante el período en que la mujer continuaba siendo fértil. Esto sugiere que el Monitor de la Fertilidad CUE, utilizando el algoritmo en el que se basa actualmente, no puede recomendarse para la planificación familiar natural. Sin embargo, se considera que el algoritmo de evaluación debe mejorarse, ya que se detectan señales útiles en el ciclo menstrual.
Similar content being viewed by others
References
SpielerJ, ThomasS. Demographic aspects of natural family planning. Int J Gynecol Obstet. 1989;1:133–44.
Elkind-HirschK, GoldzieherJ, GibbonsWE, BeschPK. Evaluation of Ovustick-Urinary luteinizing hormone kit in normal and stimulated menstrual cycles. Obstet Gynecol. 1986;67:450–52.
BrownJB, BlackwellLF, BillingsJJ et al. Natural family planning. Am J Obstet Gynecol. 1987;157:1082–9.
WHO. Temporal relationships between indices of the fertile period. Fertil Steril. 1983;39:647–55.
FlynnAM, McCarthyAM, DockerM, RoystonJP. The temporal relationship between vaginal fluid volumes obtained with Rovumeter vaginal aspirator and the fertile phase of the cycle. Hum Reprod. 1988;32:201–5.
CalameraJC, VilarO, NicholsonR. Changes in sialic acid concentration in human saliva during the menstrual cycle. Int J Fertil. 1986;31:43–5.
TrevesC, VincenziniMT, VanniP, BardazziF, CattaneoA, OgierE. Changes in enzyme levels in human cervical mucus during the menstrual cycle. Int J Fertil. 1986;31:59–66.
FreundlG, ToncaboniRF. Pilotuntersuchungen zur Bestimmung der fruchtbaren Tage im Zyklus der Frau mittels BABYCOMP. Frauenarzt. 1991;32:1055–61.
FreundlG, BaurS, BremmeM et al. Temperaturcomputer zur Bestimmung der fertilen Zeit im Zyklus der Frau: Babycomp, Bioself 110, Cyclotest D. Fertilität. 1992;8:66–76.
IsmailM, ArshatH, PulcranoJ, RoystonP, SpielerJ. An evaluation of the BIOSELF 110 fertility indicator. Contraception. 1989;39:53–71.
LabrecqueM, DrouinJ, RiouxJE, GingrasS, SpielerJM. Validity of the Bioself 110 fertility indicator. Fertil Steril. 1989;52(4):604–8.
Population Crisis Committee. Natural family planning: periodic abstinence as a method of fertility control. Population Crisis Committee: Washington, 1981.
Aboul-ElaMB, ToppsJH, MacDonaldPC. Relationship between intravaginal electrical resistance, cervicomucus characteristics and blood progesterone and LH. Animal Reprod Sci. 1983;5:259.
Blacker CM, Moghissi KS, Zador IE, Wachsmann KK. Comparison of two methods of ovulation prediction: CUE and urinary LH detection. In: Poster Session of the 35th Annual Meeting of the American College of Obstetricians and Gynecologists, 1986.
FazleabasAT, SegravesMM, Khan-DawoodFS. Evaluation of salivary and vaginal electrical resistance for determination of the time of ovulation. Int J Fertil. 1990;35:106–11.
FernandoRS, RegasJ, BetzG. Physiological mechanism associated with ovulation prediction using the CUE ovulation predictor. Hum Reprod. 1988;3:431.
LoewitK, HoppichlerF, LedermüllerG. Ovulation prediction from cyclic changes in salivary conductivity. Am J Obstet Gynecol. 1990;163:708–10.
MorenoJE, WeitzmannGA, DoodyMC, GibbonsWE, BeschP, GoldzieherJW. Temporal relation of ovulation to salivary and vaginal electrical patterns: implications for natural family planning. Contraception. 1988;38:407–18.
AG NFP, Universität Düss. Natürliche Familienplanung: neue Technologien und Studien zur Methode: Bundesfamilienministerium Bonn: Düsseldorf, 1991.
RoumenFJ, DiebenTO. Ovulation prediction by monitoring salivary electrical resistance with the Cue Fertility Monitor. Obstet Gynecol. 1988;71:49–52.
HackeloerBJ, FlemingBJ, RobinsonL, AdamA. Correlation of ultrasonic and endocrinologic assessment of human follicular development. Am J Obstet Gynecol. 1979;135:122–8.
FreundlG, TerindeR, DistlerW, BaumeisterU, HerbergerJ, KozlowskiP. Serum levels of estradiol-17β and luteinizing hormone related to follicle growth as monitored by ultrasound in women with normal menstrual cycles. Acta Endocrinol (Copenhagen). 1980;96:370–6.
VermeschM, KletzkyO, DavijanV, IsraelR. Monitoring techniques to predict and detect ovulation. Fertil Steril. 1987;47:259–64.
InslerV, MelmedH, EichenbrennerI, SerrD, LunenfeldB. The cervical score. Int J Gynecol Obstet. 1972;10:23–8.
FernandoRS, RegasJ, BetzG. Ovulation prediction by monitoring salivary electrical resistance with the CUE Fertility Monitor. Obstet Gynecol. 1988;72:282–3.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Freundl, G., Bremme, M., Frank-Herrmann, P. et al. The CUE Fertility Monitor compared to ultrasound and LH peak measurements for fertile time ovulation detection. Adv Contracept 12, 111–121 (1996). https://doi.org/10.1007/BF01849632
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF01849632