Summary
Magnetic resonance imaging (MRI) has undergone a rapid development which is still continuing. In this article a survey is given of the present status of this new diagnostic tool in the evaluation of diseases of the central nervous system.
When atoms with uneven numbers of protons or neutrons in a homogeneous magnetic field are tilted against the main vector of this field by a radiofrequency pulse, nuclear magnetic resonance can be observed. During the relaxation of the little dipoles back to the direction of the underlying magnetic field, a resonance signal is generated. The superposition of variable field gradients enables the scanning of sectional images in the axial, frontal and sagittal plane.
The variables of H+-magnetic resonance which can be utilized for imaging are: the proton density, the relaxation times T1 (spin-lattice) and T2 (spin-spin) and flow effects. While the proton density in organic tissue fluctuates only by some 10%, the relaxation times may vary by several hundred per cent. Tissue contrast, therefore, is mainly based on relaxation times differences. The image character can also be influenced by variations of imaging parameters (i.e. repetition rate, interpulse delay, read out or echo delay) in different imaging sequences, such as the spin-echo and the inversion recovery technique. Depending on these imaging parameters T1 and T2 will contribute to the signal to a varying degree. This fact is most important for the diagnostic information of MRI.
In initial clinical experiences in the diagnosis of diseases of the central nervous system, MRI has demonstrated high sensitivity in the detection of lesions (such as oedema, neoplasms, demyelinating disease), but less significance in lesion discrimination.
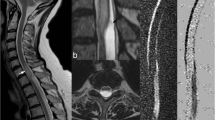
In spinal disease the direct sagittal imaging of MRI enables MRI-myelography without contrast medium, superior to conventional myelography in many cases. For detailed evaluation of disc disease, however, the spatial resolution still has to be improved.
Promising results have been obtained from flow effects. Depending on the flow velocity of blood, vessels appear white with intensive signals (slow flow) or black due to low signal intensities (rapid flow). MRI-angiography including measurement of blood flow seems possible.
MRI-contrast media are not yet available for routine clinical use. Promising results have been reported on the basis of rare-earth elements, such as gadolinium Gd3+. These substances decrease T1 and T2 with subsequent increase in signal intensity.
Concerning harmful side-effects of MRI, three possible sources have to be considered: the static magnetic field, the changing magnetic field, and radiofrequency heating. No permanent damage to organisms has been described up to the present time, in relation to the magnetic field strength used in MRI. However, there is known risk for patients who carry cardiac pace makers or metal implants such as aneurysm clips.
Similar content being viewed by others
References
Araki, T., T. Inouye, H. Suzuki, et al.: Work in Progress. Magnetic Resonance Imaging of Brain Tumors: Measurement of T1. Radiology 150 (1) (1984) 95–98
Bloch, F., W. W. Hansen, H. Packard: The nuclear induction experiment. Phys. Rev. 70 (1946) 474–485
Bowman, R. L., V. Kudravcev: Blood Flowmeter Utilizing Nuclear Magnetic Resonance. IRE Trans. Med. Electron. 6 (1959) 267–269
Brady, T. B., F. S. Buonanno, I. L. Pykett, et al.: Preliminary Clinical Results of Proton (1H) Imaging of Cranial Neoplasms: In vivo Measurements of T1 and Mobile Proton Density. AJNR 4 (1983) 225–228
Brant-Zawadzki, M., P. L. Davis, L. E. Crooks, et al.: NMR Demonstration of Cerebral Abnormalities: Comparison with CT. AJR 140 (1983) 847–854
Budinger, Th.F.: Nuclear Magnetic Resonance (NMR) in Vivo Studies: Known Thresholds for Health Effects. J. Cat. 5 (6) (1981) 800–811
Bydder, G. M., R. E. Steiner, I. R. Young, et al.: Clinical NMR Imaging of the Brain: 140 Cases. AJR 139 (1982) 215–236
Caille, J. M., B. Lemanceau, B. Bonnemain: Gadolinium as a Contrast Agent for NMR AJNR 4 (1983) 1041–1042
Chafetz, N. I., H. K. Genant, K. L. Moon, et al.: Recognition of Lumbar Disk Herniation with NMR AJR 141 (1984) 1153–1156
Crooks, L., C. M. Mills, P. L. Davis, et al.: Visualization of Cerebral and Vascular Abnormalities by NMR Imaging. The Effect of Imaging Parameters on Contrast. Radiology 144 (1982) 843–852
Devine, R. A., L. P. Clarke, S. Vaughan, et al.: Theoretical and Experimental Analysis of the Single-Coil Pulsed-NMR Method for Measuring Fluid Flow. J. Nucl. Med. 23 (1982) 1020–1024
Edelstein, W. A., P. A. Bottomley, H. R. Hart, et al.: Signal, Noise, and Contrast in Nuclear Magnetic Resonance (NMR) Imaging. J. CAT. 7 (1983) 391–401
Ganssen, A.: Nuclear Magnetic Resonance for Vessel Anatomy, Blood Flow and Metabolism Studies. Personal communication
Habermehl, A., E. H. Graul: Kernspinresonanz-Tomographie. Dtsch. Ärzteblatt 79 (30) (1982) 17–29
Han, J. S., B. Kaufman, R. J. Alfidi, et al.: Head Trauma Evaluated by Magnetic Resonance and Computed Tomography: A Comparison. Radiology 150 (1) (1984) 71–79
Herfkens, R. J., C. B. Higgins, H. Hricak, et al.: Nuclear Magnetic Resonance Imaging of Arteriosclerotic Disease. Radiology 148 (1983) 161–166
Huk, W.: NMR bei Erkrankungen des Gehirns und Rückenmarks. In: Wende, S., M. Thelen: Kernspintomographie in der Medizin. Springer, Berlin-Heidelberg-New York-Tokyo 1983, 57–67
Huk, W., W. Heindel, M. Deimling, et al.: Nuclear Magnetic Resonance (NMR) Tomography of the Central Nervous System: Comparison of Two Imaging Sequences. J. CAT. 7 (3) (1983) 468–475
Jezernik, M., M. Sentjurc, M. Schara: Proton Magnetic Resonance Characterization of Brain Tumours. Acta Neurochir. 67 (1983) 1–9
Kaufman, L., L. E. Crooks, P. E. Sheldon, et al.: Evaluation of NMR Imaging for Detection and Quantification of Obstructions in Vessels. Invest. Radiol. 17 (1982) 554–560
Lukes, S. A., L. E. Crooks, M. J. Aminoff, et al.: Nuclear Magnetic Resonance Imaging in Multiple Sclerosis. Ann. Neurol. 13 (1983) 592–601
Mills, C. M., L. E. Crooks, L. Kaufman, et al.: Cerebral Abnormalities: Use of Calculated T1 and T2 Magnetic Resonance Images for Diagnosis. Radiology 150 (1) (1984) 87–94
Mills, C. M., M. Brant-Zawadzki, L. E. Crooks, et al.: Nuclear Magnetic Resonance: Principles of Blood Flow Imaging. AJR 142 (1984) 165–170
Modic, T. M., M. A. Weinstein, W. Pavlicek, et al.: Nuclear Magnetic Resonance Imaging of the Spine. Radiology 148 (1983) 757–762
Norman, D., C. M. Mills, M. Brant-Zawadzki, et al.: Magnetic Resonance Imaging of the Spinal Cord and Canal: Potentials and Limitations. AJR 141 (1983) 1147–1152
Purcell, E. M., H. C. Torrey, R. V. Pound: Resonance absorption by nuclear magnetic moments in a solid. Phys. Rev. 69 (1946) 37, 38
Pykett, I. L., J. H. Newhouse, F. S. Buonanno, et al.: Principles of Nuclear Magnetic Resonance Imaging. Radiology 143 (1982) 157–168
Reuther, G., W. Huk: Magnetic Resonance Imaging of Flow. Work in Progress
Runge, V. M., J. A. Clanton, C. M. Lukehart, et al.: Paramagnetic Agents for Contrast-Enhanced NMR Imaging: A Review. AJR 141 (1983) 1209–1215
Simmonds, D., L. M. Banks, I. R. Young: NMR Anatomy of the Brain Using Inversion Recovery Sequences. Neuroradiology 25 (1983) 113–118
Sipponen, J. T., M. Kaste, L. Ketonen, et al.: Serial Nuclear Magnetic Resonance (NMR) Imaging in Patients with Cerebral Infarction. J. CAT. 7 (4) (1983) 585–589
Sipponen, J. T., R. E. Sepponen, A. Siluva: Chronic Subdural Hematoma: Demonstration by Magnetic Resonance. Radiology 150 (1) (1984) 79–86
Yeates, A., M. Brant-Zawadzki, D. Norman, et al.: Nuclear Magnetic Resonance Imaging of Syringomyelia. AJNR 4 (1983) 234–237
Young, I. R., G. M. Bydder, A. S. Hall, et al.: Extracerebral Collections: Recognition by NMR Imaging. AJNR 4 (1983) 833–834
Young, I. R., C. P. Randell, P. W. Kaplan, et al.: Nuclear Magnetic Resonance (NMR) Imaging in White Matter Disease of the Brain Using Spin-Echo Sequences. J. CAT. 7 (2) (1983) 290–294
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Huk, W.J., Gademann, G. Magnetic resonance imaging (MRI): Method and early clinical experiences in diseases of the central nervous system. Neurosurg. Rev. 7, 259–280 (1984). https://doi.org/10.1007/BF01892907
Issue Date:
DOI: https://doi.org/10.1007/BF01892907