Abstract
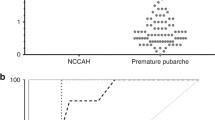
Recent studies have described mild adrenal enzymatic defects in patients presenting with precocious pubarche. In order to identify these defects we have evaluated basal and ACTH — (25 IU iv) stimulated serum adrenal steroid levels in 19 girls, 2 - to 8.3-year-old, with precocius pubarche (pubic hair Tanner II–III). Two patients had clitorial enlargement. Bone age was moderatly advanced in 10 patients and 2 to 3.7 yr in four others. Four patients had high basal serum levels of 17-hydroxyprogesterone (17OHP) (525+202 ng/dl, mean +SD), compatible with the diagnosis of nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency (NCCAH-21OH), which was confirmed by an increased response of 17OHP to ACTH (3425±953 ng/dl). Fifteen patients had moderatly elevated basal 17OHP levels (56+38 ng/dl) but a normal 17OHP response (191±71 ng/dl) to ACTH, compatible with the diagnosis of idiopathic precocious pubarche (IPP). The Cortisol response to ACTH was normal in both groups. Basal values of DHEA-S were 651 ±256 and 506+462 ng/ml and of DHEA 380±24 ng/dl and 205±102 ng/dl, in NCCAH- 21OH and IPP, respectively. We conclude that: i) clinical findings and baseline levels of DHEA-S and DHEA in IPP can be indistinguishable from the late onset 21 hydroxylase deficiency; ii) baseline levels of 17OHP are sufficient for the diagnosis of NCCAH-21OH; iii) the ACTH stimulation test is indicated only when baseline levels of 17OHP are moderately elevated (100–300 ng/dl).
Similar content being viewed by others
References
Forest M.G., Peretti E., David M., Sempè M. L’adrénarche: joue-t-elle vraiment un role determinant dans le développement pubertaire? Etude des dissociations entre adrénarche et gonadarche. Echec du traitement par la déhydroépiandrostérone sulfate dans les retards d’adrénarche. Ann. Endocr. (Paris) 43: 465, 1982.
Sizonenko P.C., Paunier L. Hormonal changes in puberty III: Correlation of plasma dehydroepiandrosterone, testosterone, FSH and LH with stages of puberty and bone age in normal boys and girls and in patients with premature or late adrenarche. J. Clin. Endocrinol. Metab. 41: 894, 1975.
Dhom G. The prepubertal and pubertal growth of the adrenal (adrenarche). Beitr. Pathol. 150: 357, 1973.
Shiebinger R.J., Albertson B.D., Cassorla F.G., Bowyer D.W., Cutler G.B. The development changes in plasma adrenal androgens during infancy and adrenarche are associated with changing activities of adrenal microsomal 17-hydroxylase and 17–20 desmolase. J. Clin. Invest. 67: 1177, 1981.
Kelnar C.J.H., Brook C.G.D. A mixed longitudinal study of adrenal steroid excretion in childhood and the mechanism of adrenarche Clin. Endocrinol. Metab. 19: 117, 1983.
Kaplowitz P.B., Coekrell J.L., Young R.B. Premature adrenarche. Clinical and diagnosis features. Clin. Pediatr. (Phila) 25: 28, 1986.
Temeck J. W., Pang S., Nelson C., New M.I. Genetic defects of steroidogenesis in premature pubarche. J. Clin. Endocrinol. Metab. 64: 609, 1987.
Rappaport R., Forest M.G., Bayard F, Duval-Beanpere G., Blizzard R.M., Migeon C.J. Plasma androgens and LH in scoliotic patients with premature pubarche. J. Clin. Endocrinol. Metab. 38: 401, 1974.
Voutilainen R., Perheentupa S., Apter D. Benign premature adrenarche: Clinical features and serum steroid levels. Acta Pediatr. Scand. 72: 707, 1983.
Pang S., Levine L.S., Stoner E., Optiz J.M., Pollack M.S., Dupont B., New M.I. Nonsalt losing congenital adrenal hyperplasia due to 3-beta -hydroxysteroid dehydrogenase deficiency with normal glomerulosa function. J. Clin. Endocrinol. Metab. 56: 802, 1983.
Zachmann M., Tassinari D., Prader A. Clinical and biological variability of congenital adrenal hyperplasia, due to 11-beta-hydroxylase deficiency. A study of 25 patients. J. Clin. Endocrinol. Metab. 56: 222, 1983.
Marshall W.A., Tanner J.M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child. 44: 291, 1969.
Marques R.M., Marcondes E., Berquo E., Prany R., Yunes J. Crescimento e desenvolvimento pubertario em criancas e adolescentes brasileiros. In: Marcondes E. (Eds.) Altura e Peso. Editora Brasileira de Ciencias, Sao Paulo, 1982, p. 30.
Greulich W.W., Pyle SI: Radiographic atlas of skeletal development of the hand and wrist. Stanford University Press, Stanford, California, 1959.
Abraham G.E. Radioimmunoassay of steroids in biological materia Acta Endocrinol. (Copenh) (Suppl.) 183: 1, 1974.
Forest M.G., Peretti E., David M. Late onset 21OH deficiency (21OHD) can be misdiagnosed as “typical premature pubarche (PP)” in childhood. Pediat. Res. 10: 624 1982, (abstract).
Rosenfield R.L., Rich B.H., Lucky A.W. Adrenarche as a cause of benign pseudopuberty in boys. J. Pediatr. 101: 1005, 1982.
Marris A.H., Reiter E.O., Geffener M.E., Lippe B.M., Itami R.M. Absence of nonclassical congenital adrenal hyperplasia in patients with precocious adrenarche. J. Clin. Endocrinol. Metab. 69: 709, 1989.
Knorr D., Bidlingmaier F., Holler W., Kernkle W., Muller B., Zachmann M. Is heterozygosity for the steroid 21-hydroxylase deficiency responsible for hirsutism, premature pubarche, early puberty and precocious puberty in children. Acta Endocrinol. (Copenh) (Suppl.) 279: 284, 1986.
New M.I., Lorenzen F., Lerner A.J., Kohn B., Oberfield S.E., Pollack M.S., Dupont B., Stonner E., Levy D.J., Pang S., Levine L.S. Genotyping steroid 21-hydroxylase deficiency: Hormonal reference data. J. Clin. Endocrinol. Metab. 46: 326, 1983.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vasconcelos Leite, M., Mendonça, B.B., Arnhold, I.J.P. et al. Identification of nonclassical 21-hydroxylase deficiency in girls with precocious pubarche. J Endocrinol Invest 14, 11–15 (1991). https://doi.org/10.1007/BF03350247
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03350247