Summary
The disposition of paracetamol following an oral dose of 1.0 g was compared in 10 healthy volunteers, 7 patients with moderate chronic renal failure and 6 patients with end stage renal failure on maintenance haemodialysis.
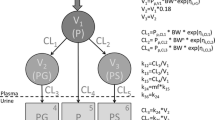
Paracetamol absorption was normal in the patients with renal failure. The mean plasma half-life of paracetamol from 2 to 8 h was similar in the 3 groups (2.1 to 2.3 h) but from 8 to 24 h it disappeared much more slowly in the renal failure patients (half-life 11.7 compared with 4.9 h in the healthy volunteers). Plasma concentrations of paracetamol glucuronide and sulphate conjugates were greatly increased in the patients with moderate renal failure and the mean plasma half-lives were 30.5 and 21.8 h respectively compared with about 3 h in the healthy volunteers. Plasma concentrations of these metabolites were even higher in the dialysis patients and there was no significant fall over 24 h. The cysteine and mercapturic acid conjugates of paracetamol could only be measured in plasma in the patients with renal failure and concentrations were very low.
The fractional urinary recovery of paracetamol and its glucuronide, sulphate, cysteine and mercapturic acid conjugates was similar in healthy volunteers and patients with moderate renal failure. The mean renal clearances of paracetamol and its glucuronide and sulphate conjugates in the healthy volunteers and patients with moderate renal failure were 15.7, 137 and 172, and 5.9, 14.5 and 14.8 ml/min respectively. In the latter patients the mean renal clearances of the cysteine and mercapturic acid conjugates were much greater at 35.4 and 80.2 ml/min. In the patients with moderate renal failure the AUC's of the glucuronide and sulphate conjugates were related to the plasma creatinine and there were significant negative correlations with the renal clearances of these metabolites and total urinary recovery. Marked cumulation of the polar glucuronide and sulphate conjugates of paracetamol would seem inevitable in patients with renal failure and the parent drug is apparently regenerated to a limited extent from retained metabolites.
Similar content being viewed by others
References
Levy G (1977) Pharmacokinetics in renal disease. Amer J Med 62: 461–465
Reidenberg MM (1977) The binding of drugs to plasma proteins and the interpretation of measurements of plasma concentrations of drugs in patients with poor renal function. Am J Med 62: 466–470
Verbeeck RK, Branch RA, Wilkinson GR (1981) Drug metabolites in renal failure: Pharmacokinetic and clinical implications. Clin Pharmacokinet 6: 329–345
Drayer DE (1977) Active drug metabolites and renal failure. Am J Med 62: 486–489
Mawer GE (1982) Dosage adjustments in renal insufficiency. Br J Clin Pharmacol 13: 145–153
Stone WJ, Walle T (1980) Massive propranolol metabolite retention during maintenance hemodialysis. Clin Pharmacol Ther 28: 449–455
Lieberman JA, Cooper TB, Suckow RF, Steinberg H, Borenstein M, Brenner R, Kane JM (1985) Tricyclic antidepressant and metabolite levels in chronic renal failure. Clin Pharmacol Ther 37: 301–307
Forrest JAH, Clements JA, Prescott LF (1982) Clinical pharmacokinetics of paracetamol. Clin Pharmacokinet 7: 93–107
Prescott LF, Wright N (1973) The effects of hepatic and renal damage on paracetamol metabolism and excretion following overdosage. A pharmacokinetic study. Br J Pharmacol 49: 602–613
Øie S, Lowenthal DT, Briggs WA, Levy G (1975) Effect of hemodialysis on kinetics of acetaminophen elimination by anephric patients. Clin Pharmacol Ther 18: 680–686
Lowenthal DT, Øie S, Van Stone JC, Briggs WA, Levy G (1976) Pharmacokinetics of acetaminophen elimination by anephric patients. J Pharmacol Exp Ther 196: 570–578
Clements JA, Critchley JAJH, Prescott LF (1984) The role of sulphate conjugation in the metabolism and disposition of oral and intravenous paracetamol in man. Br J Clin Pharmacol 18: 481–485
Clements JA, Prescott LF (1976) Data point weighting in pharmacokinetic analysis: Intravenous paracetamol in man. J Pharm Pharmacol 28: 707–709
Odar-Cederlöf I, Vessman J, Alvan G, Sjöqvist F (1977) Oxazepam disposition in uremic subjects. Acta Pharmacol Toxicol 20 [Suppl 1]: 52–62
Verbeeck R, Tjandramaga TB, Mullie A, Verbesselt R, Verberckmoes R, De Schepper PJ (1979) Biotransformation of diflunisal and renal excretion of its glucuronides in renal insufficiency. Br J Clin Pharmacol 7: 273–283
Faed EM, McQueen EG (1979) Plasma half-life of clofibric acid in renal failure. Br J Clin Pharmacol 7: 407–409
Meffin PJ, Zilm DM, Veenendaal JR (1983) Reduced clofibric acid clearance in renal dysfunction is due to a futile cycle. J Pharmacol Exp Ther 227: 732–738
Jayasinghe KSA, Roberts CJC, Read AE (1986) Is biliary excretion of paracetamol significant in man? Br J Clin Pharmacol 22: 363–366
Duggin GG, Mudge GH (1975) Renal tubular transport of paracetamol and its conjugates in the dog. Br J Pharmacol 54: 359–366
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Prescott, L.F., Speirs, G.C., Critchley, J.A.J.H. et al. Paracetamol disposition and metabolite kinetics in patients with chronic renal failure. Eur J Clin Pharmacol 36, 291–297 (1989). https://doi.org/10.1007/BF00558162
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00558162