Summary
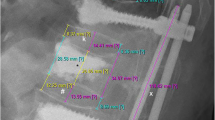
Dorsal fusion with the internal fixator has become the standard treatment of instabilities and deformities of the thoracolumbar spine. With our new device, the modular spine fixator (MSF), which has been specially designed for short-distance instrumentations, we have increasingly been treating unstable injuries of the thoracolumbar spine by one-level stabilization. Prerequisite is an accurate evaluation of the indication, including CT and MRI to assess the involvement of the intervertebral disc and the ligamental structures. The operative technique differs in some details from the procedure in moremulti-level instrumentations, especially concerning the application of the pedicle screws. The instrumentation is always combined with posterior allogenic bone grafting. Since the beginning of 1993 we also perform anterior autogenic transpedicular bone grafting. Between Januar 1991 and July 1995, 57 one-level stabilizations with the MSF were performed. Of the 57 patients operated on 39, 27 men and 12 women, with an average age of 41 years, have had a clinical and radiographic follow-up examination so far, on average, 27 months after the accident. Seventeen patients were completely free of pain and 17 patients (were only) sensivite to weather changes or had minor pain during great physical stress. Five patients had pain even during slight physical stress or at rest. The preoperatively measured Cobb angle was 15.1 ° on average, after the operation 5.2 °, and at the time of the follow-up examination amounted to 8.1 °. The patients' range of motion was normal. Only five minor complications have been seen. No implant fatigue failure has been noted in this series. We derive from these results that, for correct indications, one-level stabilization can be performed successfully and should be firmly established in the operative treatment of unstable fractures of the thoracolumbar spine.
Zusammenfassung
Die dorsale Instrumentation der verletzten thorakolumbalen Wirbelsäule mit dem Fixateur interne ist als Standardverfahren allgemein anerkannt und international verbreitet. Gängig ist dabei die bi- oder sogar mehrsegmentale Fusion. Mit der Einführung unseres eigenen Fixateurs steht ein Implantat zur Verfügung, das sich besonders für die Durchführung monosegmentaler Spondylodesen eignet. Nach ersten ermutigenden Ergebnissen sind wir daher seit 1991 zunehmend dazu übergegangen, Verletzungen der thorakolumbalen Wirbelsäule monosegmental zu versorgen. Dabei weicht die Operationstechnik etwas von der der mehrsegmentalen Fixateur-interne-Instrumentation ab. Des weiteren ist die Indikation zum monosegmentalen Vorgehen sorgfältig zu stellen. Die Voraussetzungen dazu werden unter besonderer Berücksichtigung einer umfassenden röntgenologischen Diagnostik erläutert. Die Ergebnisse von 39 mittlerweile klinisch und radiologisch nachuntersuchten Patienten werden vorgestellt. Dabei ergaben sich bei der Analyse des Bewegungsausmaßes Normalwerte. Ebenso war der röntgenologisch gemessene Repositionsverlust äußerst gering. Klinisch relevante Komplikationen waren kaum zu verzeichnen, ein Versagen des Implantats wurde in keinem Fall beobachtet.
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Junge, A., Gotzen, L., v. Garrel, T. et al. One-level instrumentation and fusion with the internal fixator in the treatment of fractures of the thoracolumbar spine. Indication, technique and results. Unfallchirurg 100, 880–887 (1997). https://doi.org/10.1007/s001130050208
Issue Date:
DOI: https://doi.org/10.1007/s001130050208