Abstract
Three further cardiovascular (CV) outcome studies of glucose-lowering drugs (linagliptin, albiglutide and dapagliflozin) have recently been published, adding to the twelve earlier within-class studies. The linagliptin study (CARMELINA) recruited people with renal disease as well as prior CV events and confirms the overall CV safety (and other safety) of the dipeptidylpeptidase-4 (DPP4) inhibitors, with no heart failure risk associated with this agent. However, taken together with the findings from two previous studies of DPP4 inhibitors (sitagliptin and saxagliptin), the three DPP4 inhibitor CV outcome trials (CVOTs) have highlighted a safety signal regarding risk of pancreatitis. Like CARMELINA, the albiglutide study (Harmony Outcome) had a very high CV event rate. Despite being a short duration study, albiglutide showed strong superiority for reduction in the major adverse CV events (MACE) composite in people with extant cardiovascular disease (CVD), in line with the earlier studies on the GLP-1 receptor agonists (GLP-1RAs) liraglutide and semaglutide. Positive effects can be detected for all these medications from before 12 months and continue for the whole study duration. No new safety issues for albiglutide are identified and the lack of a pancreatitis or a pancreatic cancer signal for this class is now clear. For the sodium–glucose cotransporter-2 (SGLT2) inhibitor class, the DECLARE-TIMI 58 study (of dapagliflozin) clearly indicates strong protection for heart failure in those with CVD, and probably in those with no prior CVD. There is also strong protection against renal decline with dapagliflozin, with similar risk estimates in DECLARE as previously reported for empagliflozin and canagliflozin. However, findings for MACE outcomes with dapagliflozin are not concordant with the empagliflozin and canagliflozin studies, and are not convincingly superior across class and for the longer term. Care is required when prescribing the SGLT2 inhibitor class of medications to people with foot vascular issues or prior amputation, and to insulin users in regard of ketoacidosis. In summary, taking into account the findings from these new studies, it is suggested that a GLP-1RA should be offered to all people with CVD and type 2 diabetes, and SGLT2 inhibitors should be prescribed for those at high risk of heart failure or with progressive decline in eGFR. DPP4 inhibitors are a safe choice within the glucose-lowering stepped algorithm.
Similar content being viewed by others

Introduction and background
Prior to the year 2000, the only glucose-lowering medication major cardiovascular (CV) outcome trials (CVOTs) in type 2 diabetes were from the University Group Diabetes Program and the UK Prospective Diabetes Study (UKPDS) [1, 2]. Preclinical signals of cardiac adverse effects with the thiazolidinediones later led the European regulator to mandate a CVOT for rosiglitazone and pioglitazone [3, 4]. However, it was only with the signal for increased myocardial infarction (MI) in phase 2/3 studies with rosiglitazone, identified by GlaxoSmithKline in 2006 and Nissen and Wolski in 2007 [5, 6], that concern was highlighted that neither conventional development programmes (of >2000 patient-year exposure) nor post-marketing surveillance (because occurrence of CV events is unremarkable in the type 2 diabetes population) could reliably detect increased CV events. Anxieties around other medications increased that concern [7, 8].
Accordingly, the US Food and Drugs Administration (FDA) mandated that, after licensing, glucose-lowering medications should achieve a maximum hazard of 1.30 (upper 95% CI) in a CVOT with a composite endpoint of first MI, stroke or CV death event [9]. This was applied even to medications with CVOTs that began before the mandate was issued [4, 10] and eventually to a new insulin analogue [11]. Prior to the studies highlighted in this review, that is those with results presented and published in October/November 2018, none of the twelve CVOTs would have failed the ‘1.30 test’, although some studies did have a CV-related adverse signal and, in others, safety signals were detected for non-CV outcomes [3, 4, 12,13,14,15,16].
The three most recently reported CVOTs were on albiglutide (Harmony Outcome), linagliptin (CARMELINA), and dapagliflozin (DECLARE-TIMI 58) [17,18,19], and hence allow discussion of the findings of three classes of glucose-lowering agents. It is noted that other studies will be reported on in 2019 (with top level announcements already made), namely REWIND (dulaglutide CVOT), PIONEER 6 (oral semaglutide, phase 3 CVOT), CREDENCE (canagliflozin renal outcome study) and, later, CAROLINA (linagliptin vs glimepiride study) [20,21,22,23]. The questions that might be asked a priori of a CVOT in a field where previous medications in the same class have already been reported on are: (1) are the findings in a comparable population; (2) are the findings consistent with previous results; (3) do the findings assist in understanding unexpected results from previous studies; (4) are there any novel insights or signals worth consideration; and (5) how should this further study affect clinical guidelines in relation to this class of drug?
Methods
A systematic search was not performed for this review, as findings for the criteria that would have been used to reject an upper 95% CI of hazard of <1.30 (a priori study power for major adverse CV events [MACE; CV death, MI, stroke], or prima facie post-priori power to detect superiority in a single study) are limited to a handful of recently published studies. Moreover, meta-analyses were not carried out either because the study findings are so consistent and robust that it would not have been useful (e.g. MACE for the studies on dipeptidylpeptidase-4 [DPP4] inhibitors) or because the studies are so disparate in the population and design that the meta-analysis findings would not apply to any group of people with diabetes in clinical practice (e.g. studies on the sodium–glucose cotransporter-2 [SGLT2] inhibitors).
Findings are given as HRs, concentrating on 95% CIs rather than central estimates, unless otherwise stated. p values are not used, except with caution to identify possible sub-group interactions or where strong enough (p < 0.001) to justify positive consideration of a secondary or observational outcome (for example, heart failure and CV death in the EMPA-REG OUTCOME study [13]).
CARMELINA: a CVOT of linagliptin
Design and populations
CARMELINA [18] complements two previous placebo-blinded, standard-of-care-controlled, CVOTs of DPP4 inhibitors (ignoring the EXAMINE study of alogliptin in people with recent acute coronary syndrome [ACS] [24]); like the TECOS study on sitagliptin and SAVOR-TIMI 53 (saxagliptin) (hereafter referred to as SAVOR), CARMELINA was performed in people with type 2 diabetes and extant CV disease, or at high risk of CV events. However, there are some differences in the populations used between these studies [10, 12, 18] (Table 1). CARMELINA recruited people with previous CV events and micro/macroalbuminuria, or those with some impairment of eGFR (<75 ml min−1 [1.73 m]−2) with macroalbuminuria, or with more severe renal impairment (eGFR <45 ml min−1 [1.73 m]−2) alone. As a result, 62% of the population had eGFR <60 ml min−1 [1.73 m]−2. Of note, linagliptin is not known to have any special effect on the kidney. This also resulted in two overlapping but distinct populations: one with extant CV disease (CVD; 57%) and one with renal disease (eGFR <60 ml min−1 [1.73 m]−2 or macroalbuminuria (74%); 33% of the population were in both groups [18]. This limits generalisability of the findings as, while the highest event rates were seen in those with more advanced renal impairment rather than prior CV disease, it is unclear how results from the combined population might be applied to a general diabetes population. However, the interaction of renal groups and major study outcomes are presented in the supplementary materials of the original publication and, while the numbers within subgroups provide low power, no concerns are obvious [18].
While the three studies of DPP4 inhibitors agree that short-term (<3 year) outcomes do not differ between DPP4 inhibitors and standard of care, they are less similar regarding the studied populations than the previous paragraph might imply. CARMELINA, like SAVOR, had only a small Asian population (and all three studies include barely any black/Afro-Caribbean people) but TECOS recruited in Asia (Table 1). More strikingly, CARMELINA had very high baseline use of insulin and high rates of new insulin starters during the study (Table 1), to the extent that it could be argued that the results are only generalisable to insulin-treated populations.
The generalisability issue is further marred by the very high event rate in this study (Table 1). Event rates in CVOTs have shown inflation over the years, but the rate of 5.6% per year reported in the placebo group has only previously been exceeded in post-ACS studies. The chronic kidney disease (CKD) population does have high CVD rates, which may have contributed to the high event rate observed in this study. That the observed event rate is far in excess of previous studies recruiting only a secondary prevention population (e.g. PROactive, TECOS), or the intensive therapy studies ACCORD and ADVANCE [3, 10, 25, 26], leads to unanswered questions as to how the population was recruited in CARMELINA. Were these perhaps cardiology patients with diabetes rather than people with diabetes with CV/renal disease?
Findings
The above being said, the headline findings are entirely consistent with TECOS and SAVOR and confirm, with adequate power, that in the short-term linagliptin shows no CV safety signal (Table 2). The heart failure signal unexpectedly observed with saxagliptin [12] was not found in CARMELINA and, with its absence also in TECOS [10], it is now clear that this is not a class effect. The EXAMINE (alogliptin) data are non-contributory to this evaluation as its CIs for heart failure are very wide thus being consistent with any of the other three studies [27]. Useful sensitivity analyses were performed, including per-protocol, a more robust test of non-inferiority. Breakdown of MACE by its components suggests there is no reason to doubt the validity of this composite endpoint (unlike with SGLT2 inhibitors, as discussed further below), but CARMELINA does not have the power to be as convincing as TECOS in regard to this (Table 2). The positive interaction test result for MACE based on HbA1c levels is unadjusted and one of 25 such tests [18], and thus unlikely to be a reliable finding.
A major secondary endpoint in CARMELINA was the composite endpoint for kidney disease, prospectively allocated the greater part of the alpha power at that level. This was mainly defined as a confirmed >40% decline in eGFR, with minor contributions (due to low event number) from end stage renal disease and renal death. As might be anticipated given the SAVOR and TECOS results, this did not differ between linagliptin vs standard of care (HR 1.04 [95% CI 0.89, 1.22]) [18, 28, 29]. TECOS showed a sustained decline in eGFR with sitagliptin use, to a clinically insignificant extent [28], but CARMELINA does not report this data.
The authors of CARMELINA also present findings of two other composites (nephropathy and microvascular disease), both of which were driven by progression of albuminuria and showed advantage to linagliptin vs standard-of-care. Albuminuria in type 2 diabetes is, however, a marker of vascular inflammation rather than microvascular disease and positive findings have been reported for a wide range of glucose-lowering medications, including sulfonylureas, PPAR-γ agonists, other DPP4 inhibitors and GLP-1 receptor agonists (GLP-1RAs) [2, 14, 26, 28,29,30]. This is therefore not a remarkable or useful finding.
Safety and tolerability
DPP4 inhibitors have an excellent safety and tolerability record, the exceptions being the heart failure signal in SAVOR (as discussed above) and the possibility of increased risk of pancreatitis. With the relatively small study population exposed to linagliptin (n = 3494) for only 1.9 years on average, CARMELINA does not answer any question regarding low-frequency safety signals, including pancreatitis. Indeed, the data on confirmed acute pancreatitis from the three DPP4 inhibitor studies discussed here are not strong, even after combined analysis (events: n = 49 on DPP4 inhibitor vs n = 26 on placebo). Hence, although the signal is a clear, it is by no means a certain one and provides no reassurance that the drugs are safe in this respect (Table 3).
Summary and consequences
The CARMELINA findings are not derived from a population that is directly comparable with TECOS and SAVOR but are consistent with findings from these studies. The absence of a heart failure signal makes it more likely that the ‘finding’ in SAVOR is due to chance. Nonetheless, given that sitagliptin and linagliptin do not show this heart failure signal, these agents would appear to be the better choice over saxagliptin and any other DPP4 inhibitor without a proper CV study in a regular diabetes populations, unless the individual’s risk of heart failure is known to be low. However, the absence of any clear benefit, except for their excellent tolerability, would seem to put this class behind medications showing some CV or kidney disease advantage, where this need is identified (see below for GLP-1RAs and SGTL2 inhibitors).
Harmony Outcome: a CVOT of albiglutide
Design and populations
Albiglutide is no longer actively marketed, but the mixed findings from other GLP-1RA CVOTs mean that the findings from Harmony Outcome [17] (hereafter referred to as Harmony) are interesting and useful. As with CARMELINA, however, the study population was relatively small, particularly for such a short study duration (Table 4). The very high event rate in the placebo group (5.9% per year) was unexpected [31] and again raises questions of generalisability to ambulant diabetes populations, even to those with extant CVD, as was required for entry into this study.
Harmony complements three other placebo-blinded, standard-of-care-controlled CVOTs of GLP-1RAs, excluding the ELIXA study of lixisenatide in people who had recent ACS [14, 15, 32, 33]. The three prior studies included individuals with CV risk factors but no prior CVD, and, unlike Harmony, two of these studies had total event numbers that were clearly aimed at testing superiority [14, 33]. Nevertheless, hierarchical testing for superiority after inferiority analysis was pre-specified in Harmony. SUSTAIN-6 was a phase 3 study designed to exclude the 1.80 (not 1.30) upper confidence limit for hazard (this is perceived by some as a limitation of the study) [15, 34]. As with CARMELINA, SUSTAIN-6 and LEADER, Harmony had very high rates of combination insulin therapy, with 62% of participants taking insulin by the study end (Table 4); this too raises concern over generalisability of the findings. Indeed, the test for interaction for baseline use or non-use of insulin nearly reaches conventional statistical significance (p = 0.053) but with CV outcome advantage to the non-insulin group, these findings thus mitigating possible concern.
Harmony had a very low proportion of Asian and black participants (Table 4), indeed to an extent that any determination of interaction of the primary outcome between ethnic groups is unsound. None of the GLP-1RA studies are then directly applicable to the majority of the world’s population with type 2 diabetes. In Harmony, there was no interaction for the primary outcome between subgroups of Hispanic and non-Hispanic white ethnicity.
Findings
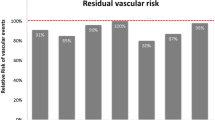
Despite being powered for non-inferiority, in Harmony the central HR for MACE was 0.78, which, with 766 primary events (Table 4), brings the upper CI down to 0.90 (Table 2), which is a more comfortable margin over equivalence to standard of care than for the three earlier GLP-1RA studies (Tables 2 and 5). While numerically this is driven by MI events, the HRs of the components of MACE in this study are consistent with the primary outcome and each other (Table 2). At the doses used in Harmony, albiglutide was less efficacious in lowering glucose and body weight than the other agents in the other CV-positive studies, consistent with phase 3 findings [35], but the CV outcomes with albiglutide are at least as impressive. These findings suggest that the beneficial effect of albiglutide on CV outcomes is not mediated by changes in plasma glucose or energy balance, and that the dose–response curve for vascular protection is not coincident with that for glucose-lowering between the four GLP-1RA agents investigated in LEADER, SUSTAIN-6, EXSCEL and Harmony. These findings perhaps even suggest that the effect of this class of drug on CV risk may not be mediated through the classic GLP-1 receptor or, alternatively that they may reflect differential tissue access [36].
It is possible to put together a panel of HRs and their CIs for the four GLP-1RA CVOTs for MACE, its components and all-cause mortality (Table 5). If this is done, the best of these five variables (using the criteria of best upper CI) are scattered amongst the studies, with EXSCEL and LEADER tying for all-cause death. This suggests that the findings are drawn by chance from the same population of effect. Harmony, then, can be regarded as entirely consistent in terms of CV outcomes with the other three agents.
Tests for subgroup interaction in Harmony, with a couple of p values <0.05, are as to be expected for multiple testing. The ‘significant’ findings for age and smoking [17] are both inconsistent in direction within the subgroups.
Harmony is unusual in that the phase 2/3 programme for albiglutide included, by design, a number of studies that continued for at least 2 years, in which MACE events were prospectively adjudicated [37]. Indeed, composite exposure to albiglutide and placebo at phase 2/3 was not very different from that in Harmony Outcome [37]. However, the number of people with MACE events was just 105 (HR 0.99 [95% CI 0.65, 1.49]), emphasising (as has been shown with rosiglitazone and DPP4 inhibitors) how phase 2/3 studies with low numbers can give misleading findings for CV outcomes [6, 38].
Safety and tolerability
Interestingly, the rather patient-unfriendly injection system for weekly albiglutide in Harmony did seem to lead to a higher discontinuation rate from study medication than for semaglutide (allowing for exposure period) (Table 4). This problem was also noticeable for the original exenatide modified release formulation (MR; long-acting) in the EXSCEL study over a longer exposure period [33]. Albiglutide was already known to show a modest degree of gastrointestinal intolerance and a low but measurable rate of injection-site reactions [39]; these findings were confirmed in Harmony [17]. The data for other pre-defined adverse outcomes of special interest, including pancreatitis (Table 3), are not concerning. However, actual exposure to albiglutide in Harmony was low (~7000 person-years), so the power to detect uncommon side effects was low.
Harmony also has little power to address the issue of accelerated progression of retinopathy with GLP-1RA use, which was raised by SUSTAIN-6, with a weak signal being revealed in LEADER [14, 15]. However, the absence of this issue with albiglutide would be consistent with the glucose-lowering hypothesis, semaglutide being much more effective in this regard [15].
Summary and consequences
Because albiglutide is no longer promoted for use, the findings here are of indirect significance and importance. Nevertheless, the observed clear benefits regarding CV outcomes confirms that there is a class effect of clinical significance, probably extending to all longer-acting agents (Tables 2 and 5). The divergence between CV and glucose-/body weight-lowering efficacy is important for our understanding of how the GLP-1RA class mechanistically achieves amelioration of MACE events within 12 months of taking the medication, with this effect (according to Kaplan–Meier curves) continuing to the end of each study. While injection therapies are not always welcome, it does now seem that the offer of CV protection cannot be denied to anyone with type 2 diabetes and extant CVD, if resources allow. No serious safety signals have emerged for this class.
The detailed results of the REWIND study are awaited (expected June 2019) and should throw further light on the issue of whether people without extant CVD can benefit from prescription of GLP-1RAs [20]. Details of the CVD/non-CVD subgroups within REWIND and the interactions between them will be needed to assess the implications for the non-CVD population.
DECLARE-TIMI 58: a CVOT of dapagliflozin
Design and populations
DECLARE-TIMI 58 [19] (herein referred to as DECLARE) joins the EMPA-REG OUTCOME study and the CANVAS Program (composed of two studies) as reported CVOTs of SGLT2 inhibitors [13, 16, 19]. However, these three studies are of different designs; DECLARE, like the original CANVAS study, had a majority population (59%) without extant CVD (Table 6). However, because of its very large base population and relatively long duration of follow-up, the power of this new study for those with CVD remained relatively good. This mixed population might have allowed a better assessment of effects in those with and without CVD, which was not possible in EMPA-REG OUTCOME (in which 99% of participants had known atherosclerotic CVD) and was only possible with limited power in the CANVAS Program. However, with the exception of heart failure and the renal composite outcome, DECLARE’s headline findings are less certain than expected (Table 2).
DECLARE had a somewhat lower proportion of participants on insulin therapy at baseline (mitigated for safety by the high exposure) and a better sex mix than in the EMPA-REG OUTCOME (empagliflozin) study (Table 6). However, the number of participants who were of black ethnicity is again too small to make meaningful conclusions regarding differences between ethnic groups. Further, due to the exclusion of people with eGFR <60 ml min−1 [1.73 m]−2, meaningful data in this group is not provided, with one useful exception (discussed below).
This large study had a longer follow-up (4.2 years) compared with the other SGLT2 inhibitor CVOTs, and a low discontinuation rate when taking the study duration into account; hence, in DECLARE, exposure to dapagliflozin was usefully high (Table 6).
Findings
Discussion of the findings of DECLARE is complicated due to the multiple composite endpoints analysed, each of these often driven by one component and, therefore, invalid. A composite endpoint analysis is only valid if the components of the composite behave similarly or, if they do not, if they are of similar clinical impact. For example, CV death plus hospitalisation for heart failure is a composite that makes sense in heart failure studies but not in diabetes-care studies. Here, the hazard findings are of a 5–27% reduction for the composite but, when each component is analysed individually, this is clearly driven by a strong reduction in heart failure (HR 0.73 [95% 0.61, 0.88]), with no evidence of change in CV death (HR 0.98 [0.82, 1.17]; Table 2). The effect of dapagliflozin on heart failure risk is consistent with that for empagliflozin and canagliflozin [13, 16]. Further, for the composite, this is a clear finding on interaction testing in both the CVD and non-CVD subgroups. Although information on these subgroups is unavailable for canagliflozin, this has been hypothesised from a large observational study of SGLT2 inhibitors [40].
The MACE findings in DECLARE are presented as being of interest for non-inferiority testing only, but clearly do not support superiority (Table 2). They are, however, otherwise useful since the data from EMPA-REG OUTCOME and CANVAS are not easy to interpret. For example, the form of the Kaplan–Meier curves is different between the three studies: in EMPA-REG OUTCOME and CANVAS Program, after 18 and 24 months, respectively, the lines converge or are parallel (meaning no further advantage from the drug); in DECLARE, however, the lines begin to diverge in a way that is indicative of putative advantage with dapagliflozin use [13, 16, 19]. Overall, there is no evidence of any MACE advantage in the non-CVD group on subgroup analysis [19]. The conservative interpretation of these findings would be that the differences between studies (medications) are due to chance and that there is no reliable evidence of MACE advantage with use of SGLT2 inhibitors, except perhaps in the short-term. This interpretation even then would apply only to high-risk individuals with extant CVD, as observed in CANVAS [41].
Furthermore, the MACE components also behave differently between the SGLT2 inhibitor studies (Table 2). In EMPA-REG OUTCOME the HRs were very different (to the extent where empagliflozin has now been granted a US licence for the prevention of CV death only), while, in CANVAS, the HRs for the individual components were fairly consistent (thus, canagliflozin now has a US licence for CVD prevention) [42, 43]. In DECLARE, the findings for the MACE components are mostly consistent, albeit with no suggestion of superiority, and with, as noted above, no effect on risk of CV death.
An issue here is stroke; the SGLT2 inhibitors reduce blood pressure to a seemingly useful degree, consistent with their volumetric effects, but stroke hazard was not reduced in any of the SGLT2 inhibitor CVOTs and, indeed, there was a signal for harm with empagliflozin (Table 2). An explanation may be that the increases in haemoglobin/haematocrit induced by this class of agents, and the blood volumetric/hypotensive effect, are countering the blood pressure advantage, preventing stroke reduction. This may have clinical consequences for those with diabetes who experience a transient ischaemic attack (TIA) or stroke while taking these medications, and others at particular risk of such an event.
DECLARE gives evidence for the impact of dapagliflozin on two renal composites, one including CV death and renal death and the other (more conventionally) only renal death, with both composites also including end stage kidney failure and a 40% reduction in eGFR. The latter composite provided a very strong finding (HR 0.53 [95% CI 0.43, 0.66]), consistent with EMPA-REG OUTCOME and CANVAS. This finding is driven by the eGFR component (judging by the steps in the Kaplan–Meier curve), although we do not yet have crucial information on rate of eGFR decline in DECLARE participants and whether this finding is preserved below an eGFR of 60 ml min−1 [1.73 m]−2 [44, 45]. However, despite the few participants in DECLARE with an eGFR <60 ml min−1 [1.73 m]−2 (thus only 59 events for this renal composite), the interaction analysis across the spectrum of eGFR in the population is consistent by subgroups.
Safety and tolerability
The DECLARE findings are, in general, neutral for safety and tolerability except for genital infections, which may account for the majority of the excess in discontinuations [19]. Notably, there is a curious absence of an excess of reports vs placebo related to volumetric effects. Toe amputations and subsequent higher-level amputations were raised as an issue with SGLT2 inhibitor use by the CANVAS study and by observational studies [16, 46]. These were not increased in DECLARE, but it is not made clear whether a signal may have been developing before preventative measures were put into place (in response to the CANVAS findings). In DECLARE, peripheral vascular disorder as an adverse event doubled with dapagliflozin use, but numbers of events are small. Ankle fractures were numerically higher on dapagliflozin vs placebo, and humerus fractures were lower. Diabetic ketoacidosis numbers in the main text (which are substantially different to those reported in the supplementary tables in the publication) were approximately doubled in the dapagliflozin group; this was said to be mainly an effect in the insulin-treated population [19]. The 0.17% excess rate of ketoacidosis with dapagliflozin vs placebo over the study duration would, if all ketoacidosis events were in the insulin-treated group, imply an excess rate of approximately 1 per 1000 people per year. The severity of these ketoacidosis events is unclear.
Summary and consequences
The disparity of the design of and findings from the CVOTs for empagliflozin, canagliflozin and, now, dapagliflozin, means that some uncertainty still remains, with the current study not adding much clarity. However, the exceptions are very important clinically, with renal protection being perhaps the most significant of these. Even in the absence of longitudinal eGFR data from DECLARE, the findings regarding renal protection are strong and consistent between the three studies; hence, this is clearly a class effect. The results of the CREDENCE study (of canagliflozin) are not yet available in detail, but the primary endpoint is renal outcome and the study closed early because of a strong finding of efficacy on interim analysis [21]. This kidney protection by SGLT2 inhibitors is possibly the biggest clinical gain in diabetes care since laser photocoagulation and statins. Furthermore, heart failure protection was consistently observed in the SGLT2 inhibitor CVOTs and, thus, this is also a clear class effect. In both these areas DECLARE is important because it has provided an opportunity to perform subgroup analyses, which indicate that, compared with standard of care, the relative effects of dapagliflozin are as strong for the non-CVD population as they are for the CVD population.
Other than the beneficial impact on renal events and heart failure, the advantages, and indeed side effects, of these medications are unclear, both individually and as a class. Unlike EMPA-REG OUTCOME, the benefits regarding CV death with SGLT2 inhibitors was not found in CANVAS or DECLARE. This is perhaps owing to the beneficial impact of empagliflozin on heart failure in a particularly high-risk CV population, with the placebo group in EMPA-REG OUTCOME having a three times higher CV death rate than in DECLARE [19, 47]. For EMPA-REG OUTCOME, the very divergent findings for CV death and stroke invalidate, for clinical and statistical purposes, the MACE finding [13], while the findings for MACE in DECLARE are equivocal [19]. For the CANVAS Program, MACE is improved only for the majority subgroup with prior CVD, with no clear evidence of advantage after 24 months [16, 41]. Though underpowered as an individual MACE component in all three studies, only the MI effect seems consistent between the CVOTs for SGLT2 inhibitors, with no heterogeneity observed following meta-analysis of these studies [47].
The findings of increased fracture rate with canagliflozin in CANVAS, though consistent with time, were clearly absent in CANVAS-R and do not appear with the other SGLT2 inhibitor agents. The findings from CREDENCE may help to shed light on this matter.
In terms of risk of amputation, a problem is that the data collected in the EMPA-REG OUTCOME study was apparently not sufficient to address the question with confidence [48]. In addition, in DECLARE, once aware of this issue, the problem is likely to have been ameliorated by avoiding SGLT2 inhibitor use if there had been a prior amputation, and stopping the medication if risk of peripheral ischaemia or infection appeared.
Neither EMPA-REG OUTCOME nor CANVAS appear able to address the potential ketoacidosis issue with SGLT2 inhibitor use. However, on the basis of data from DECLARE [19], it is both a real and a low-frequency problem in people using insulin alongside dapagliflozin, although for reasons still unclear.
Overall conclusion and messages for guidelines
Clearly the three recent CVOTs provide knowledge to help develop diabetes guidelines and clinical management algorithms and protocols. Within the DPP4 inhibitor class, the linagliptin findings (from CARMELINA) perhaps have the least impact, with no reach beyond glucose-lowering, except perhaps in confirming the absence of a class adverse effect on heart failure and confirming safety in the presence of renal impairment. A lingering doubt remains over increased risk of pancreatitis with DPP4 inhibitor use. Nevertheless, the DPP4 inhibitors remain the best tolerated of any glucose-lowering medications and, therefore, they should retain their position in the stepped approached to diabetes therapy, when other agents are not specifically indicated or preferred [49].
The study findings for the GLP-1RAs (including the new Harmony findings) indicate that this class of drugs does not have a pancreatitis signal. This suggests that the possible increase in this signal with the DPP4 inhibitors does not occur through increased GLP-1 concentrations, but rather they may be affecting degradation of some other mediator relevant to the pancreatic vasculature or ducts, but this is speculative. GLP-1RAs have a relatively early beneficial effect on already damaged arteries, which persists over time, with evidence for both protection for MI and stroke. That this effect is seen with albiglutide, which has relatively low potency (clinically), might hint that it is not mediated through the classical GLP-1 receptor pathway. However, these findings could also be caused by the albumin moiety of this medication, which may prevent access to GLP-1 receptors in some sites, while the endothelium and inflamed arterial wall allow direct access [36]. Acylated GLP-1RAs, like liraglutide and semaglutide, could also have better access to hypothalamic centres. It has also been speculated that the human sequence medications have intrinsic advantage for CV protection over the exendin peptides, but this does not fit with our knowledge of receptor interactions [36]. Nonetheless, GLP-1RAs are now clearly indicated in people with diabetes and extant CVD, whether a weight-loss effect is desired or not [49]. The remaining negatives of GLP-1RAs are administration via injections and gastrointestinal side effects. In summary, the findings from the Harmony study do not seem to change the recent suggestions of the EASD/American Diabetes Association (ADA) Consensus Group [49].
The clinical positioning of the SGLT2 inhibitors is less easy. Clearly, if there is a risk of heart failure, these medications are indicated and perhaps we should now be performing pro brain natriuretic peptide (proBNP) estimations as part of annual surveillance of individuals with diabetes. However, it is not clear whether SGLT2 inhibitors should be used merely because of extant CVD. It is clear that if eGFR is declining, particularly if it is declining through 60 ml min−1 [1.73 m]−2 but above 30 ml min−1 [1.73 m]−2, then these agents are strongly indicated. Precautions, including continuing foot surveillance, are mandatory in anyone with prior peripheral vascular problems, or those developing these problems, while on SGLT2 inhibitor-based medications. Use in people on insulin therapy should only be undertaken when users are aware of the small risk of ketoacidosis, and with the appropriate continuing education to counter this risk.
To conclude, what does this mean for CVOTs in general? From the point of view of MACE safety, they have been a complete failure, with no issues identified. Unlike the PPAR-γ agonists, for which a preclinical signal had been shown to exist, no CV issues have arisen with use of DPP4 inhibitors, GLP-1RAs and SGLT2 inhibitors, apart from the heart failure signal with saxagliptin. Of course, the benefits of these drugs (discussed above) have been evidenced by the trials discussed in this review, but not as mandated by the US FDA. One view is that large pragmatic safety studies ought to continue, not specifically directed at CVD, but including brain health, malignancy, bone health and the like, with directed superiority studies as felt appropriate by manufacturers and the academic community. An exception would be where a preclinical or phase 2/3 safety signal had been found.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- CVOT:
-
Cardiovascular outcome trial
- DPP4:
-
Dipeptidylpeptidase-4
- FDA:
-
US Food and Drugs Administration
- GLP-1RA:
-
GLP-1 receptor agonist
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
- SGLT2:
-
Sodium–glucose cotransporter-2
References
University Group Diabetes Program (1970) A study of the effects of hypoglycemic agents on vascular complications in patients with adult-onset diabetes: sections I and II. Diabetes 19(Suppl 2):747–830
Holman RR, Paul SK, Bethel MA et al (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15):1577–1589. https://doi.org/10.1056/NEJMoa0806470
Dormandy JA, Charbonnel B, Eckland DJ et al (2005) Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 366(9493):1279–1289. https://doi.org/10.1016/S0140-6736(05)67528-9
Home PD, Pocock SJ, Beck-Nielsen H et al (2009) Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet 373(9681):2125–2135. https://doi.org/10.1016/S0140-6736(09)60953-3
European Medicines Agency (2010) Assessment report for Avandia. https://www.ema.europa.eu/documents/variation-report/avandia-h-c-268-a20-75-epar-assessment-report_en.pdf. Accessed 1 Nov 2018
Nissen SE, Wolski K (2007) Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 356(24):2457–2471. https://doi.org/10.1056/NEJMoa072761
Bombardier C, Laine L, Reicin A (2000) Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. N Engl J Med 343(21):1520–1528. https://www.nejm.org/doi/full/10.1056/NEJM200011233432103
Nissen SE, Wolski K, Topol EJ Effect of muraglitazar on death and major adverse cardiovascular events in patients with type 2 diabetes mellitus. JAMA 294(20):2581–2586. https://jamanetwork.com/journals/jama/fullarticle/201927. https://doi.org/10.1001/jama.294.20.joc50147
Food and Drugs Administration (2008) Guidance for industry diabetes mellitus — evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. https://www.fda.gov/downloads/Drugs/Guidances/ucm071627.pdf. Accessed 1 Nov 2018
Green JB, Bethel A, Armstrong PW (2015) Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 373(3):232–242. https://doi.org/10.1056/nejmoa1501352
Marso SP, McGuire DK, Zinman B, Poulter NR et al (2017) Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med 377(8):723–732. https://doi.org/10.1056/NEJMoa1615692
Scirica BM, Bhatt DL, Braunwald E et al (2013) Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 369(14):1317–1326. https://doi.org/10.1056/NEJMoa1307684
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128. https://doi.org/10.1056/NEJMoa1504720
Marso SP, Daniels GH, Brown-Frandsen K et al (2016) Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 375(4):311–322. https://doi.org/10.1056/NEJMoa1603827
Marso SP, Bain SC, Consoli A et al (2016) Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 375(19):1834–1844. https://www.nejm.org/doi/full/10.1056/nejmoa1607141
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657. https://doi.org/10.1056/NEJMoa1611925
Hernandez AF, Green JB, Janmohamed S et al (2018) Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony outcomes): a double-blind, randomised placebo-controlled trial. Lancet 392(10157):1519–1529. https://doi.org/10.1016/S0140-6736(18)32261-X
Rosenstock J, Perkovic V, Johansen OE et al (2018) Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA randomized clinical trial. JAMA. https://doi.org/10.1001/jama.2018.18269
Wiviott SD, Raz I, Bonaca MP et al (2018) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. https://doi.org/10.1056/NEJMoa1812389
Eli Lilly and Company (2018) Trulicity® (dulaglutide) demonstrates superiority in reduction of cardiovascular events for broad range of people with type 2 diabetes. Available from https://www.multivu.com/players/English/8442751-lilly-trulicity-rewind-trial-type-2-diabetes/. Accessed 01 Nov 2018
Janssen (2018) Phase 3 CREDENCE renal outcomes trial of INVOKANA® (canagliflozin) is being stopped early for positive efficacy findings. Available from https://www.janssen.com/phase-3-credence-renal-outcomes-trial-invokanar-canagliflozin-being-stopped-early-positive-efficacy. Accessed 1 Nov 2018
Marx N, Rosenstock J, Kahn SE et al (2015) Design and baseline characteristics of the CARdiovascular Outcome Trial of LINAgliptin Versus Glimepiride in Type 2 Diabetes (CAROLINA®). Diab Vasc Dis Res 12(3):164–174. https://doi.org/10.1177/1479164115570301
Novo Nordisk (2018) Oral semaglutide demonstrates a favourable cardiovascular safety profile and a significant reduction in cardiovascular death and all-cause mortality in people with type 2 diabetes in the PIONEER 6 trial. Available from https://www.novonordisk.com/bin/getPDF.2226789.pdf. Accessed 1 Nov 2018
White WB, Cannon CP, Heller SR et al (2013) Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 369(14):1327–1335. https://doi.org/10.1056/NEJMoa1305889
Gerstein HC, Miller ME, Byington RP et al (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358(24):2545–2559. https://doi.org/10.1056/NEJMoa0802743
Patel A, MacMahon S, Chalmers J et al (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358(24):2560–2572. https://doi.org/10.1056/NEJMoa0802987
Zannad F, Cannon CP, Cushman WC et al (2015) Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet 385(9982):2067–2076. https://doi.org/10.1016/S0140-6736(14)62225-X
Cornel JH, Bakris GL, Stevens SR et al (2016) Effect of sitagliptin on kidney function and respective cardiovascular outcomes in type 2 diabetes: outcomes from TECOS. Diabetes Care 39(12):2304–2310. https://doi.org/10.2337/dc16-1415
Mosenzon O, Leibowitz G, Bhatt DL et al (2017) Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care 40(1):69–76. https://doi.org/10.2337/dc16-0621
Viberti GC (2003) Rosiglitazone: potential beneficial impact on cardiovascular disease. Int J Clin Pract 57(2):128–134
Green JB, Hernandez AF, D’Agostino RB et al (2018) Harmony outcomes: a randomized, double-blind, placebo-controlled trial of the effect of albiglutide on major cardiovascular events in patients with type 2 diabetes mellitus—rationale, design, and baseline characteristics. Am Heart J 203:30–38. https://doi.org/10.1016/j.ahj.2018.03.030
Pfeffer MA, Claggett B, Diaz R et al (2015) Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 373(23):2247–2257. https://doi.org/10.1056/NEJMoa1509225
Holman RR, Bethel MA, Mentz RJ et al (2017) Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med 377(13):1228–1239. https://doi.org/10.1056/NEJMoa1612917
Kaul S (2017) Mitigating cardiovascular risk in type 2 diabetes with antidiabetes drugs: a review of principal cardiovascular outcome results of EMPA-REG OUTCOME, LEADER, and SUSTAIN-6 trials. Diabetes Care 40(7):821–831. https://doi.org/10.2337/dc17-0291
Pratley RE, Nauck MA, Barnett AH et al (2014) Once-weekly albiglutide versus once-daily liraglutide in patients with type 2 diabetes inadequately controlled on oral drugs (HARMONY 7): a randomised, open- label, multicentre, non-inferiority phase 3 study. Lancet Diabetes Endocrinol 2(4):289–297. https://doi.org/10.1016/S2213-8587(13)70214-6
Drucker DJ (2018) The ascending GLP-1 road from clinical safety to reduction of cardiovascular complications. Diabetes 67(9):1710–1719. https://doi.org/10.2337/dbi18-0008
Fisher M, Petrie MC, Ambery PD et al (2015) Cardiovascular safety of albiglutide in the Harmony programme: a meta-analysis. Lancet Diabetes Endocrinol 3(9):697–703. https://doi.org/10.1016/S2213-8587(15)00233-8
Mannucci E, Mosenzon O, Avogaro A (2016) Analyses of results from cardiovascular safety trials with DPP-4 inhibitors: cardiovascular outcomes, predefined safety outcomes, and pooled analysis and meta- analysis. Diabetes Care 39(Suppl 2):S196–S204. https://doi.org/10.2337/dcS15-3024
Ahrén B, Carr MC, Murphy K et al (2017) Albiglutide for the treatment of type 2 diabetes mellitus: an integrated safety analysis of the HARMONY phase 3 trials. Diabetes Res Clin Pract 126:230–239. https://doi.org/10.1016/j.diabres.2017.02.017
Kosiborod M, Lam CSP, Kohsaka S et al (2018) Cardiovascular events associated with SGLT-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL 2 study. J Am Coll Cardiol 71(23):2628–2639. https://doi.org/10.1016/j.jacc.2018.03.009
Mahaffey KW, Neal B, Perkovic V et al (2017) Canagliflozin for primary and secondary prevention of cardiovascular events results from the CANVAS Program (canagliflozin cardiovascular assessment study). Circulation 137(4):323–334. https://doi.org/10.1161/circulationaha.117.032038
Boehringer Ingelheim International GmbH (2018) Prescribing information JARDIANCE. Available from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/204629s018lbl.pdf. Accessed 1 Nov 2018
Janssen Pharmaceutical Companies (2018) Prescribing information INVOKANA. Available from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/204042s027lbl.pdf. Accessed 1 Nov 2018
Wanner C, Inzucchi SE, Lachin JM et al (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334. https://doi.org/10.1056/NEJMoa1515920
Perkovic V, de Zeeuw D, Mahaffey KW et al (2018) Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Lancet Diabetes Endocrinol 6(9):691–704. https://doi.org/10.1016/S2213-8587(18)30141-4
Khouri C, Cracowski JL, Roustit M (2018) SGLT-2 inhibitors and the risk of lower-limb amputation: is this a class effect? Diabetes Obes Metab 20(6):1531–1534. https://doi.org/10.1111/dom.13255
Zelniker TA, Wiviott SD, Raz I et al (2018) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. https://doi.org/10.1016/S0140-6736(18)32590-X
European Medicines Agency (2018) SGLT2 inhibitors: information on potential risk of toe amputation to be included in prescribing information. Available from https://www.ema.europa.eu/medicines/human/referrals/sglt2-inhibitors-previously-canagliflozin. Accessed 1 Nov 2018
Davies MJ, D’Alessio DA, Fradkin J (2018) Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 61(12):2461–2498. https://doi.org/10.1007/s00125-018-4729-5
Acknowledgements
The author thanks colleagues internationally for discussions and insights around the studies on these medications. However, the wording of this review has not been discussed with any other party and the author takes sole responsibility for the views expressed. Reviewers are thanked for the quality of their reports.
Author information
Authors and Affiliations
Contributions
The author was the sole contributor to this paper.
Corresponding author
Ethics declarations
No funding or writing assistance has been provided for this article. The author or institutions with which he is associated has had funding for his research, advisory and/or lecturing activities from the manufacturers of every one of the medications listed in Tables 1, 4 and 6, and in particular in regard of sitagliptin, albiglutide and canagliflozin, and from many competing products. This then specifically includes AstraZeneca, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Hanmi, Janssen, Merck (MSD), Novo Nordisk, Sanofi, and Takeda.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Home, P. Cardiovascular outcome trials of glucose-lowering medications: an update. Diabetologia 62, 357–369 (2019). https://doi.org/10.1007/s00125-018-4801-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4801-1