Abstract
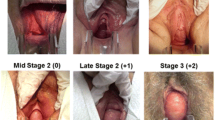
We sought to describe the relationship between patient symptoms and pelvic organ prolapse (POP) and report the sensitivity, specificity, and positive and negative predictive value of these POP symptoms. Two urologists and four urogynecologists developed a standardized pelvic floor questionnaire based on face validation for use at three female pelvic floor disorder clinics. Specific questions related to prolapse included questions on urinary splinting, digital assistance for defecation, and a bulge per vagina. Prolapse was assessed with the standardized Pelvic Organ Prolapse Quantitative (POP-Q) terminology. The analysis included 1912 women. Urinary splinting was uncommon (<10%) when Ba <0, but ranged between 23 and 36% for stage III and IV Ba prolapse. Digital assistance was equally common in stage II Bp prolapse (21–38%) and stage III-IV Bp prolapse (26–29%). Only 6–11% of women with stage 0 or I POP reported symptoms of bulge, but with stage II it increased to 77%. Urinary splinting is 97% specific for anterior prolapse. The report of a bulge has an 81% positive predictive value and a 76% negative predictive value. Very few patients without anterior prolapse will report urinary splinting. Digital assistance for fecal evacuation is no more common with massive posterior prolapse than with moderate posterior prolapse. Patient report of a bulge is a valuable screening tool for POP and should prompt a careful exam.


Similar content being viewed by others
References
Peterson M, Holbrook JH, Von Hales D et al (1992) Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med 156:163–165
Hampton JR, Harrison MJ, Mitchell JR, Prichard JS, Seymour C (1975) Relative contributions of history-taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients. Br Med J 2:486–489
Jensen JK, Nielsen FR Jr, Ostergard DR (1994) The role of patient history in the diagnosis of urinary incontinence. Obstet Gynecol 83:904–910
Melville JL, Miller EA, Fialkow MF et al (2003) Relationship between patient report and physician assessment of urinary incontinence severity (miscellaneous article). Am J Obstet Gynecol 189:76–80
Thakar R, Stanton S (2002) Regular review: management of genital prolapse. BMJ 324:1258–1262
Spence-Jones C, Kamm MA, Henry MM, Hudson CN (1994) Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and urinary stress incontinence. Br J Obstet Gynaecol 101:147–152
Zbar AP, Lienemann A, Fritsch H, Beer-Gabel M, Pescatori M (2003) Rectocele: pathogenesis and surgical management. Int J Colorectal Dis 18:369–384
Fialkow MF, Gardella C, Melville J et al (2002) Posterior vaginal wall defects and their relation to measures of pelvic floor neuromuscular function and posterior compartment symptoms. Am J Obstet Gynecol 187:1443–1449
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA (1994) Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res 3:291–306
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Weber AM, Abrams P, Brubaker L et al (2001) The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12:178–186
Ellerkmann RM, Cundiff GW, Melick CF et al (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185:1332–1338
Bump RC, Fantl JA, Hurt WG (1988) The mechanism of urinary continence in women with severe uterovaginal prolapse: results of barrier studies. Obstet Gynecol 72:291–295
Barber MD, Cundiff GW, Weidner AC et al (1999) Accuracy of clinical assessment of paravaginal defects in women with anterior vaginal wall prolapse. Am J Obstet Gynecol 181:87–90
Weber AM, Walters MD, Ballard LA et al (1998) Posterior vaginal prolapse and bowel function. Am J Obstet Gynecol 179:1446–1449; discussion 1449–1450
Nygaard I, Bradley C, Brandt D (2004) Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol 104:489–497
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The authors listed above wrote this contribution on behalf of the San Diego Pelvic Floor Consortium. We acknowledge additional members of the San Diego Pelvic Floor Consortium including Michael E. Albo (University of California, San Diego Medical Center, San Diego, CA, USA) and Karl M. Luber (Kaiser Permanente Medical Center, San Diego, CA, USA)
Rights and permissions
About this article
Cite this article
Tan, J.S., Lukacz, E.S., Menefee, S.A. et al. Predictive value of prolapse symptoms: a large database study. Int Urogynecol J 16, 203–209 (2005). https://doi.org/10.1007/s00192-004-1243-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-004-1243-8