Abstract
Introduction and hypothesis
We describe the prevalence of symptomatic pelvic organ prolapse (sPOP), urinary incontinence (UI), fecal incontinence (FI) and obstetric anal sphincter injury (OASI) 20 years after one vacuum extraction (VE) delivery compared with one spontaneous vaginal delivery (SVD) or one acute caesarean section (ACS).
Method
We performed a register-based national cohort study of primipara who delivered between 1985 and 1988 and had no further deliveries. Medical Birth Register data were linked to data from postal questionnaires distributed 20 years after the birth (response rate 65.2 %, n = 5 236). Main outcome measures were prevalence and risk factors for pelvic floor disorders (PFDs) and OASI and their impact after VE compared with SVD and ACS. Multivariate logistic regression models were used.
Results
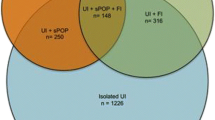
The late prevalence of UI, sPOP, and FI was almost identical between VE and SVD. VE almost tripled the rate of OASI compared with SVD (6.3 vs. 2.4 %, p < 0.001). FI rate after an OASI was similar for both VE and SVD [30.2 vs. 27.8 %, adjusted odds ratio (aOR) 1.12; 95 % confidence interval (CI) 0.49–2.56]. Comparing VE without laceration with VE complicated by OASI increased the rate of FI (from 15.4 to 30.2 %, aOR 2.55; 95 % CI 1.26–5.15) and UI (from 39.0 to 61.4 %, aOR 2.28; 95 % CI 1.19–4.34), but the rate of sPOP was almost unaltered (from 15.0 to 15.9 %).
Conclusions
VE did not result in additional long-term PFDs provided the rate of OASI was similar to that after SVD. OASI after VE substantially increased the prevalence of FI and UI but did not alter the rate of sPOP.
Similar content being viewed by others
References
Malmström T (1954) Vacuum extractor, an obstetrical instrument. Acta Obstet Gynecol Scand Suppl 33:1–31
O’Mahony F, Hofmeyr GJ, Menon V (2010) Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev CD005455
Elvander C, Ekéus C, Gemzell-Danielsson K, Cnattingius S (2013) Reason for the increasing use of vacuum extraction in Sweden: a population based study. Acta Obstet Gynecol Scand 92:1175–1182
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A (2014) Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population based-cohort study. Am J Obstet Gynecol 210:59.e1-6
Rothman KJ, Greenland S, Lash TL (2008) Design strategies to improve study accuracy, restriction. In: Modern Epidemiology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia, pp 168–182
Thomas V, Shek KL, Guzmán Rojas R, Dietz HP (2015) Temporal latency between pelvic floor trauma and presentation for prolapse surgery: a retrospective observational study. Int Urogynecol J 26:1185–1189
Leijonhufvud Å, Lundholm C, Cnattingius S, Granath F, Andolf E, Altman D (2011) Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol 204:70.e1-7
Sultan AH, Kamm MA, Hudson CN, Bartram CI (1994) Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ 308:887–891
de Leeuw JW, Struijk PC, Vierhout ME, Wallenburg HC (2001) Risk factors for third degree perineal ruptures during delivery. BJOG 108:383–387
Gyhagen M, Bullarbo M, Nielsen T, Milsom I (2013) The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:144–151
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H (1993) Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health 47:497–499
Tegerstedt G, Miedel A, Maehle-Schmidt M, Nyren O, Hammarstrom M (2005) A short-form questionnaire identified genital organ prolapse. J Clin Epidemiol 58:41–46
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Sultan AH, Thakar R (2009) Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE (eds.) Perineal and anal sphincter trauma, 2nd edn. Springer Verlag London, p19, pp. 33–51
Groom KM, Paterson-Brown S (2002) Can we improve on the diagnosis of third degree tears? Eur J Obstet Gynecol Reprod Biol 101:19–21
Handa VL, Blomquist JL, McDermott KC, Friedman S (2012) Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol 119:233–239
Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ (2015) Pelvic organ prolapse and incontinence 15–23 years after first delivery: a cross-sectional study. BJOG 122:964–97120
Gyhagen M, Bullarbo M, Nielsen T, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:152–160
DeLancey JOL, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115:979–984
Dietz HP, Franco AV, Shek KL, Kirby A (2012) Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand 91:211–214
Dietz HP (2015) Forceps: towards absolescence or revival? Acta Obstet Gynecol Scand 94:347–351
Robinson JN, Norwitz ER, Cohen AP, McElrath TF, Lieberman ES (1999) Episiotomy, operative vaginal delivery, and significant perineal trauma in nulliparous women. Am J Obstet Gynecol 181:1180–1184
Ekéus C, Nilsson E, Gottvall K (2008) Increasing incidence of anal sphincter tears among primiparas in Sweden: a population-based register study. Acta Obstet Gynecol Scand 87:564–573
Mous M, Muller SA, de Leeuw JW (2008) Long-term effects of anal sphincter rupture during vaginal delivery: faecal incontinence and sexual complaints. BJOG 115:234–238
O’Grady JP, Gimovsky ML, McIlhargie CJ (1995) Vacuum extraction in modern obstetric practice. Parthenon Publishing Group, New York
Samuelsson E, Ladfors L, Wennerholm UB, Gåreberg B, Nyberg K, Hagberg H (2000) Anal sphincter tears: prospective study of obstetric risk factors. BJOG 107:926–931
Pettersson K, Aine J, Yousaf K, Sturm D, Westgren M, Aine G (2015) Traction force during vacuum extraction: a prospective observational study. BJOG 122:1809–1816
Ramphul M, Kennelly MM, Burke G, Murphy DJ (2015) Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial. BJOG 122:558–563
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for the SWEPOP study was obtained from the regional (reference no. 381–07, August 13 2007) and national (34-9148/2007, October 26, 2007) Ethical Review Boards. All women gave written information before participation.
Funding
The study was supported by a National LUA/ALF grant nr 11315, a grant from the Region of Västra Götaland, Sweden, grants from The Göteborg Medical Society and Hjalmar Svenssons Fund, The funding source had no role in study design, data analysis, data interpretation, or writing of the report. MG and IM had full access to all study data and had final responsibility for the decision to submit for publication.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Nilsson, I., Åkervall, S., Milsom, I. et al. Long-term effects of vacuum extraction on pelvic floor function: a cohort study in primipara. Int Urogynecol J 27, 1051–1056 (2016). https://doi.org/10.1007/s00192-015-2928-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2928-x