Abstract
Summary
Interpretation of change in serial bone densitometry using least significant change (LSC) may not lead to optimal decision making. Using the principles of Bayesian statistics and decision sciences, we developed the Optimal Decision Criterion (ODC) which resulted in 11–12.5% higher rate of correct classification compared with the LSC method.
Introduction
The interpretation of change in serial bone densitometry emphasizes using least significant change (LSC) to distinguish between true changes and measurement error.
Methods
Using the principles of Bayesian statistics and decision sciences, we developed the optimal decision criterion (ODC) based on maximizing a ‘utility’ function that rewards the correct and penalizes the incorrect classification of change. The relationship between LSC and ODC is demonstrated using a clinical sample from the Manitoba Bone Density Program.
Results
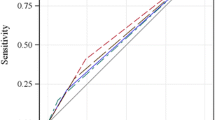
Under certain conditions, it can be shown that using LSC at the 95% confidence level implicitly equates the benefit of 39 true positive diagnoses with the harm of one false positive classification of BMD change. ODC resulted in an 11% higher rate of correct classification for lumbar spine BMD change and a 12.5% better performance for classifying total hip BMD change compared with LSC with this method.
Conclusions
ODC has the same clinical interpretation as LSC but with two major advantages: it can incorporate prior knowledge of the likely values of the true change and it can be fine-tuned based on the relative value placed on the correct and incorrect classifications. Bayesian statistics and decision sciences could potentially increase the yield of a BMD monitoring program.


Similar content being viewed by others
References
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. JAMA 288:1889–1897
Lewiecki EM, Watts NB, McClung MR et al (2004) Official positions of the international society for clinical densitometry. J Clin Endocrinol Metab 89:3651–3655
Lenchik L, Kiebzak GM, Blunt BA (2002) What is the role of serial bone mineral density measurements in patient management? J Clin Densitom 5(Suppl):S29–S38
Baim S, Wilson CR, Lewiecki EM et al (2005) Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 8:371–378
Bonnick SL, Johnston CC Jr, Kleerekoper M et al (2001) Importance of precision in bone density measurements. J Clin Densitom 4:105–110
Cummings SR, Palermo L, Browner W et al (2000) Monitoring osteoporosis therapy with bone densitometry: misleading changes and regression to the mean. Fracture Intervention Trial Research Group. JAMA 283:1318–1321
Sterne JA, Davey SG (2001) Sifting the evidence-what’s wrong with significance tests? BMJ 322:226–231
Lilford RJ, Braunholtz D (1996) The statistical basis of public policy: a paradigm shift is overdue. BMJ 313:603–607
Chesnut CH III, Rosen CJ (2001) Reconsidering the effects of antiresorptive therapies in reducing osteoporotic fracture. J Bone Miner Res 16:2163–2172
Gluer CC, Blake G, Lu Y et al (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5:262–270
Nguyen TV, Pocock N, Eisman JA (2000) Interpretation of bone mineral density measurement and its change. J Clin Densitom 3:107–119
Pauker SG, Kassirer JP (1980) The threshold approach to clinical decision making. N Engl J Med 302:1109–1117
Leslie WD, Metge C (2003) Establishing a regional bone density program: lessons from the Manitoba experience. J Clin Densitom 6:275–282
Leslie WD, Caetano PA, MacWilliam LR et al (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8:25–30
Leslie WD (2006) The importance of spectrum bias on bone density monitoring in clinical practice. Bone 39:361–368
Weiss NA (eds) (2005) A Course in Probability. Addison-Wesley
Van DS (2006) Prior specification in Bayesian statistics: three cautionary tales. J Theor Biol 242:90–100
Tversky A, Kahneman D (1974) Judgment under Uncertainty: Heuristics and Biases. Science 185:1124–1131
Karpf DB, Shapiro DR, Seeman E et al (1997) Prevention of nonvertebral fractures by alendronate. A meta-analysis. Alendronate Osteoporosis Treatment Study Groups. JAMA 277:1159–1164
Nguyen TV, Sambrook PN, Eisman JA (1997) Sources of variability in bone mineral density measurements: implications for study design and analysis of bone loss1. J Bone Miner Res 12:124–135
Jones G, Nguyen T, Sambrook P et al (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. BMJ 309:691–695
Hoch JS, Briggs AH, Willan AR (2002) Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ 11:415–430
Dalkey N, Helmer O (1963) An experimental application of the Delphi method to the use of experts. Manage Sci 9:458–467
Patel JK, Read CB (eds) (1982) Handbook of the normal distribution. New York, Dekker, M
Acknowledgments
This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee. The author and committee would like to express their gratitude to Manitoba Health, the Winnipeg Regional Health Authority and the Brandon Regional Health Authority for their vision, trust and support in the establishment of this Program.
Funding
none
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Appendix 1. Calculation of the probability of TP, TN, FP, and FN
Using the notations describes in the text and the general assumptions of our approach (see Methods), we have
Based on the properties of the normal distribution [24], and that e and x are assumed independent, the joint distribution of the x and y is a bivariate normal:
The first and second parameters are the mean and covariance matrix of the bivariate normal distribution, respectively. The probability that a subject falls into each category can, therefore, be calculated using the cumulative distribution function of the bivariate normal distribution from the above equation. Defining the function Ф(a,b,ρ) as the cumulative distribution function of the standard bivariate normal distribution with at point (a, b) with correlation function ρ, we will have:
Appendix 2. Derivation of ODC
One way to derive ODC is to solve the derivate of the utility function in Eq. 4 for T x . However, an easier way is to consider the utility of a decision based on observing change Y
while from Eq. 2:
The goal is to find T y that results in the selection of the maximum of the two terms in U for all Y. This would be achieved by matching T y to a Y for which the utilities for positive and negative classification are equal. For any Y below this critical value, our policy would detect an unfavorable change and the utility of our decision equals the first term, which is also the maximum of the two for the same Y given the fact it is a descending function of Y as long as S TP > S FP and S TN > S FN . Setting the two terms equal and solving for Y, we will have:
Solving for Y yields Eq. 6 for ODC.
Rights and permissions
About this article
Cite this article
Sadatsafavi, M., Moayyeri, A., Wang, L. et al. Optimal decision criterion for detecting change in bone mineral density during serial monitoring: A Bayesian approach. Osteoporos Int 19, 1589–1596 (2008). https://doi.org/10.1007/s00198-008-0615-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0615-1