Abstract
In the present study, the effect of three controversially discussed risk factors for colorectal cancer, a fat-rich diet (16% raw fat content), dietary folic acid supplementation (50 mg folic acid/kg lab chow) and a human-relevant concentration (0.1 ppm) of the heterocyclic aromatic amine 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP), either alone or in combination, on the induction of aberrant crypt foci (ACF) in the colon of male Fischer 344 rats was analyzed. The mean number of ACF per rat in the case of the four groups fed a fat-rich diet tended to be higher than that of the four groups being fed a standard diet. However, the increase in the mean number of ACF per rat only reached statistical significance in the case of the rats receiving a fat-rich lab chow supplemented with 50 mg/kg folic acid. Moreover, a concentration of 0.1 ppm PhIP per se, either in the standard or in the fat-rich lab chow, did not lead to an increase in the mean number of ACF per rat. In conclusion, the present study provides additional evidence for a colon cancer promoting effect of folic acid supplementation when rodents are fed the compound in supraphysiological concentrations.
Similar content being viewed by others
Introduction
Colorectal cancer is the third most common cancer in men (6,63,000 cases, 10% of the total) and the second in women (5,71,000 cases, 9.4% of the total) worldwide (Ferlay et al. 2010; Jemal et al. 2011). Moreover, about 6,08,000 deaths from colorectal cancer are estimated worldwide, accounting for 8% of all cancer deaths and making it the fourth most common cause of death from cancer. As early as in 1999, a scientific panel of the World Health Organization postulated that consumption of red meat and particularly of processed meat most probably enhances the risk to develop colorectal cancer (Scheppach et al. 1999). In 2007, a joint committee of the World Cancer Research Fund and the American Institute for Cancer Research reviewed the available scientific literature and concluded that red meat as well as processed meat is a convincing cause of colorectal cancer (World Cancer Research Fund/American Institute for Cancer Research 2007). In this regard, it has been suggested that heterocyclic aromatic amines (HCAs) being formed when muscle meat is strongly heated may trigger colorectal cancer development (Sinha et al. 2001, 2005; Shin et al. 2007; Rohrmann et al. 2009; Zheng and Lee 2009; Cross et al. 2010).
HCAs are pyrolysis products derived from amino acids or proteins that emerge when protein-rich food is fried, grilled, or cooked. They are particularly formed on the surface of strongly heated fish and meat, but low levels of HCAs have also been detected in white and red wine, in different beer types and in the tar fraction of cigarettes. Among the various HCAs known, the quantitatively most important one in fish and meat samples is 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP). PhIP is mutagenic in bacteria and in mammalian cells (Thompson et al. 1987) and carcinogenic in the colon of male rats (Ito et al. 1991; Hasegawa et al. 1993). It should be noted that in the case of the studies by Ito et al. (1991) and Hasegawa et al. (1993) as well as in most of the later reports having been published in the scientific literature and dealing with the induction of colon carcinomas by PhIP, rats were fed with extremely high (i.e., totally human-irrelevant) amounts of PhIP in the range of 100 to 400 ppm. In contrast, in those feeding studies, in which PhIP was used in human-relevant concentrations (i.e., <0.1 ppm), no preneoplastic or neoplastic lesions were induced (Fukushima et al. 2004; Doi et al. 2005; Kühnel et al. 2009), whereby in these three studies PhIP was added to standard rat chow.
Various studies reported that high levels of dietary fat were able to enhance colon epithelial cell proliferation, thereby promoting colon carcinogenesis (Thornton and MacDonald 1997; Kim et al. 1998; Fujise et al. 2007). In accordance with these observations Ochiai et al. (1996) and Ubagai et al. (2002) showed that a fat-rich diet strongly enhanced the induction of preneoplastic lesions in the colon of rats fed 400 ppm PhIP (Ochiai et al. 1996; Ubagai et al. 2002). However, up to now it is not known whether a human-relevant concentration of PhIP added to a fat-rich diet could eventually lead to the formation of colonic lesions.
Folic acid fortification of cereal grain flour was fully implemented in the United States and Canada in 1998 and has led to a significant reduction in neural tube defects in neonates (Berry et al. 2010). In this context, the possibility that folic acid fortification may enhance the risk to develop colorectal carcinomas is a matter of considerable debate. On the one hand, Mason et al. (2007) highlighted a temporal association between folic acid fortification of enriched cereal grains in the United States and Canada and an increase in the incidence of colorectal carcinomas in these two countries. Furthermore, in a multicenter study by Cole et al. (2007), the safety and efficacy of folic acid supplementation (1 mg/day, in part in combination with aspirin) for preventing colorectal adenomas was analyzed in participants with a recent history of colorectal adenomas. Three to 5 years after beginning folic acid supplementation, the risk of developing advanced colorectal lesions, multiple (≥3) colorectal adenomas as well as noncolorectal cancers (prostate cancer) was significantly increased (Cole et al. 2007). On the other hand, very recent studies show that folic acid fortification actually reduces the risk to develop colorectal cancer (Gibson et al. 2011; Kennedy et al. 2011; Lee et al. 2011; Stevens et al. 2011).
In a limited number of animal studies, the effect of supraphysiological levels of folic acid on colon carcinogenesis has been analyzed. Kim et al. (1996) reported a nonsignificant trend toward increased colorectal tumorigenesis in Sprague–Dawley rats treated with 1,2-dimethylhydrazine and fed a supraphysiological dose of folic acid (40 mg folic acid/kg diet, i.e., 20 times the daily folic acid requirement of rats). In support of this early finding, azoxymethane in combination with a dietary folic acid supplementation exceeding the basal requirements of rats by 1,000 times (2.0–5.0 g folic acid/kg diet) significantly increased the number of so-called aberrant crypt foci (ACF), preneoplastic lesions in the rat colon (Bird 1987; Tudek et al. 1989), when compared to the combination of the above-mentioned colon carcinogen and a standard diet including 2 mg folic acid/kg diet in Fischer 344 rats (Reddy et al. 1996; Wargovich et al. 1996, 2000). Kim (2004) hypothesized that in a strongly procarcinogenic environment, in which the appearance of microscopic neoplasms is inevitable, exceptionally high folic acid supplementation may promote the progression of chemically induced colorectal neoplastic lesions. Up to now, it is not known whether a supraphysiological level of folic acid combined with a fat-rich diet and/or a human-relevant concentration of PhIP will enhance the induction of ACF in the rat colon.
In the present study, the effect of three controversially discussed risk factors for colorectal cancer, a fat-rich diet, dietary folic acid supplementation and a human-relevant concentration of PhIP, either alone or in combination, on the induction of ACF in the colon of Fischer 344 rats was analyzed.
Materials and methods
Chemicals
All chemicals were of reagent grade and from commercial sources. PhIP was obtained from Albrecht Seidel (Biochemisches Institut für Umweltcarcinogene, Großhansdorf, Germany).
Animals and diets
Five to six-week-old male Fischer 344 rats were purchased from Charles River WIGA (Deutschland) GmbH (Sulzfeld, Germany) and allowed to acclimatize to the housing conditions for 4 weeks before the start of the experiment. One animal per cage was held under specific pathogen-free conditions at a room temperature of 22°C, 40–60% air humidity, a fixed 16/8 h day and night cycle and free access to food and water. PhIP was added to a standard rodent lab chow and a fat-rich rodent lab chow from Altromin Spezialfutter (Lage, Germany) to give a final PhIP concentration of 0.1 ppm. The raw fat content of the standard and the fat-rich lab rodent chow was 5 and 16%, respectively. The concentration of the various fatty acids in the standard and fat-rich diet is listed in Table 1. The physiological and supraphysiological concentration of folic acid in the standard and the fat-rich rodent lab chow was 2 and 50 mg/kg, respectively. All diets were regularly analyzed for the presence of mutagenic compounds such as N-nitrosamines and aflatoxins by the manufacturer (Altromin Spezialfutter) and were consistently tested negative throughout the whole experimental period. The animal study was approved by the local regulatory agency for animal experiments (Niedersächsisches Landesamt für Verbraucherschutz und Lebensmittelsicherheit, Oldenburg, Germany [approval number 33.9-42502-04-09/1729]).
Experimental design
Rats were randomly divided into 8 groups of 12 animals each. Group 1 was fed with the standard lab chow (5% raw fat and 2 mg/kg folic acid), group 2 with the standard lab chow (5% raw fat, 2 mg/kg folic acid) containing 0.1 ppm PhIP, group 3 with the lab chow containing 5% raw fat and 50 mg/kg folic acid, group 4 with the lab chow containing 5% raw fat, 50 mg/kg folic acid and 0.1 ppm PhIP, group 5 with the fat-rich lab chow (16% raw fat and 2 mg/kg folic acid), group 6 with the fat-rich lab chow (16% raw fat, 2 mg/kg folic acid) containing 0.1 ppm PhIP, group 7 with the lab chow containing 16% raw fat and 50 mg/kg folic acid, and group 8 with the lab chow containing 16% raw fat, 50 mg/kg folic acid and 0.1 ppm PhIP. Body weight and food consumption were recorded weekly. All animals were killed after 12 months by decapitation following CO2 inhalation. The entire large intestine was removed for dissection and flushed with cold phosphate buffered saline solution (PBS) to remove intestinal content. The tissue was opened longitudinally, washed extensively with PBS, and fixed in 4% formalin (Roti®-Histofix 4%; Carl Roth, Karlsruhe, Germany).
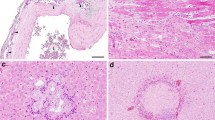
Histology
The formalin-fixed tissues were stained with a 0.1% w/v methylene blue solution in PBS for 10 min. Thereafter, the tissue was washed with PBS and the number of ACF per animal was determined by making use of a SZX16 stereomicroscope from Olympus (Hamburg, Germany).
Statistics
The body and liver weight data were subjected to an analysis of variance, and the statistical significance was established by using Tukey’s post hoc test. The data on the number of ACF per animal were analyzed with the Kruskal–Wallis test and Dunn’s post hoc test.
Results
Six out of 96 rats died before the end of the feeding period of 12 months (one animal in group 2, three animals in group 5, and two animals in group 6), the overall mortality of 6.25% being very low. No statistically significant difference in food consumption was observed between the different groups, rats in groups 1–8 consuming 90 ± 8, 89 ± 8, 94 ± 8, 91 ± 11, 86 ± 11, 101 ± 9, 101 ± 10, and 103 ± 10 g food/week, respectively. Based on the weekly food consumption, rats fed 0.1 ppm PhIP (i.e., those in groups 2, 4, 6, and 8) took up 8.8–10.2 μg PhIP/rat/week. In the case of the groups 5–8, which had been fed the fat-rich lab chow, the body weight was 12–21% higher than in the groups 1–4, which had received the standard lab chow (Table 2). Furthermore, the mean weight of the rats in the groups 6–8 was significantly higher than that of the rats in group 5. The feeding of the fat-rich lab chow led to a strong fat accumulation in the liver, the mean liver weight in the groups 5–8 being 2 to 2.4-fold higher than in the groups 1–4 (Table 2).
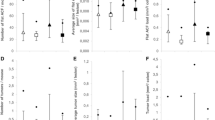
The mean number of ACF per rat in the different groups is shown in Fig. 1. It is evident that the mean number of ACF per rat in the case of the four groups that received a fat-rich lab chow tended to be higher than that of the four groups being fed a standard lab chow. However, the above-mentioned increase in the mean number of ACF per rat only reached statistical significance in the case of the rats receiving a fat-rich lab chow supplemented with 50 mg/kg folic acid (group 7) (Fig. 1). Moreover, a concentration of 0.1 ppm PhIP per se, either in the standard or in the fat-rich lab chow, did not lead to an increase in the mean number of ACF per rat (Fig. 1).
Discussion
Various surveys have shown that the daily uptake of HCAs in general does not exceed the amount of 1 μg per person (Rohrmann et al. 2009; Carthew et al. 2010). Because of this extremely low exposure level, the Senate Commission on Food Safety of the German Research Foundation (1998) came to the conclusion that the risk to develop colorectal cancer due to the presence of HCAs in food is very low. This early evaluation is supported by a very recent study by Carthew et al. (2010), in which the calculated “Margin Of Exposure” (MOE) value for PhIP was extremely high (i.e., >100.000). The MOE value represents the quotient between the doses of a compound causing cancer in animals and the estimated exposure level of humans to that compound. If the calculated MOE value is lower than 10.000, the European Food Safety Authority (EFSA) considers the carcinogenic risk of a compound to humans to be high; if it is greater than 10.000, the carcinogenic risk is supposed to be low. In the present study, feeding a human-relevant concentration of PhIP either in a standard diet or in a fat-enriched diet to rats did not lead to an increase in the number of preneoplastic lesions (ACF) in the rat colon. Thus, the results obtained herein experimentally support previous evaluations that human-relevant concentrations of PhIP alone or in combination with a fat-rich diet is not a major factor leading to colorectal cancer in humans (Senate Commission on Food Safety of the German Research Foundation 1998; Santarelli et al. 2008; Carthew et al. 2010).
The fact that feeding 0.1 ppm PhIP for up to 12 months did not lead to a statistically significant increase in the number of ACF per rat is in accordance with previous reports (Fukushima et al. 2004; Doi et al. 2005; Kühnel et al. 2009). In this context, Fukushima et al. (2004) postulated that a threshold of 50 ppm for the PhIP-mediated induction of aberrant crypt foci in the rat colon can actually be defined. Whereas it is evident from this and previous studies (Fukushima et al. 2004; Doi et al. 2005; Kühnel et al. 2009) that a human-relevant concentration of PhIP alone is not sufficient to initiate colon carcinogenesis, a mixture of food contaminants (e.g., HCAs, polycyclic aromatic hydrocarbons, nitrosamines, acrylamide) could very well overcome the threshold to induce preneoplastic lesions in the colon. Further experiments are needed to clarify this important open question in chemically induced colon carcinogenesis.
The fact that the number of ACF pro rat in all four experimental groups having been fed a fat-rich diet was, although not statistically significant, higher than the number of ACF pro animal in the four experimental groups receiving a standard lab chow suggests that a fat-rich diet per se may support the development of ACF. In this context, it has indeed been demonstrated that a fat-rich diet strongly enhances the number of ACF in rats fed extremely high concentrations of PhIP (400 ppm; Ochiai et al. 1996; Ubagai et al. 2002) or azoxymethane (Nigro et al. 1975; Bull et al. 1979). However, as shown in the present study, a fat-rich diet does not lead to an increase in the number of ACF pro animal when these are concomitantly fed a human-relevant concentration of PhIP.
The most striking result of this study is that the feeding of rats with a supraphysiological concentration of folic acid and a fat-rich diet leads to a significant increase in the number of ACF per rat. These observations are the first to be made in rats that have not concomitantly received a known carcinogen. Since folic acid is not mutagenic (i.e., does not possess tumor initiating activity) and the fat-rich diet did not include any genotoxins such as N-nitrosamines and aflatoxins (see “Materials and methods”) with tumor initiating activity, the question as to the initiating stimulus for the ACF remains unanswered. However, it has been known for a number of years now that Fischer 344 rats spontaneously develop a limited number of ACF throughout their lifespan (Furukawa et al. 2002), and this has been corroborated in this study: a low number of ACF were seen in the group of rats fed a standard diet containing physiological amounts of folic acid. Hence, the results obtained herein could very well be the consequence of a supraphysiological concentration of folic acid promoting the growth of spontaneously initiated ACF and together with previous reports demonstrating that the growth of chemically initiated ACF is significantly stimulated by supraphysiological levels of folic acid (Reddy et al. 1996; Wargovich et al. 1996, 2000; Lindzon et al. 2009) lend support to the concept that folic acid supplementation, once early preneoplastic lesions such ACF (Bird 1987; Tudek et al. 1989) have developed, promotes carcinogenesis (Kim 1999; Choi and Mason 2002; Kim 2003, 2004).
As to the mechanisms involved in the tumor promoting activity of folic acid, it has been proposed that increased DNA methylation leads to the silencing of the expression of regulatory or mismatch repair genes, which in turn may provide a growth advantage to the initiated cells (Shen and Issa 2002; Issa 2004; Wallace et al. 2010). Furthermore, it has very recently been shown that multiple pathways related to inflammation and immune response were upregulated in rectosigmoid biopsies from volunteers receiving supplemental folic acid (1 mg/day) for 8 weeks (Protiva et al. 2011). In the case of the fat-rich diet, it has been proposed that it upregulates the activity of cyclooxygenase-2 (Singh et al. 1997; Rao et al. 2001), thereby leading to the enhanced production of prostaglandin E2, which results in the activation of multiple intracellular signaling pathways, including the transactivation of the epidermal growth factor receptor and G-protein-mediated activation of β-catenin/TCF-dependent transcription (Wu et al. 2010).
In summary, the present study provides additional evidence for a colon cancer promoting effect of folic acid supplementation when rodents are fed the compound in supraphysiological concentrations. While folic acid supplementation in humans may prevent the development of a colorectal tumor in those people without a preexisting preneoplastic lesion in the colorectum, folic acid supplementation in those people with an existing preneoplastic colorectal lesion may support the development of a colorectal tumor (Cole et al. 2007; Fife et al. 2011). Regardless of the ongoing discussion on the pros and cons of folic acid supplementation to prevent colorectal cancer and based on the overwhelming body of evidence supporting the protective effect of periconceptional folic acid supplementation against neural tube defects, cleft palate, spina bifida, and anencephaly, the advice for women planning a pregnancy to increase folic acid intake during the preconception period to prevent the above-mentioned pregnancy outcomes remains valid.
References
Berry RJ, Bailey L, Mulinare J, Bower C, Folic Acid Working Group (2010) Fortification of flour with folic acid. Food Nutr Bull 31(1 Suppl):S22–S35
Bird RP (1987) Observation and quantification of aberrant crypts in the murine colon treated with a colon carcinogen. Preliminary findings. Cancer Lett 37:147–151
Bull AW, Soullier BK, Wilson PS, Hayden MT, Nigro ND (1979) Promotion of azoxymethane-induced intestinal cancer by high-fat diet in rats. Cancer Res 39:4956–4959
Carthew P, DiNovi M, Woodrow Setzer R (2010) Application of the Margin of Exposure (MOE) approach to substances in food that are genotoxic and carcinogenic. Example: CAS No: 105650–23-5 PhIP (2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine). Food Chem Toxicol 48(Suppl 1):S98–S105
Choi SW, Mason JB (2002) Folate status: effects on pathways of colorectal carcinogenesis. J Nutr 132(Suppl):2413S–2418S
Cole BF, Baron JA, Sandler RS, Haile RW, Ahnen DJ, Bresalier RS, McKeown-Eyssen G, Summers RW, Rothstein RI, Burke CA, Snover DC, Church TR, Allen JI, Robertson DJ, Beck GJ, Bond JH, Byers T, Mandel JS, Mott LA, Pearson LH, Barry EL, Rees JR, Marcon N, Saibil F, Ueland PM, Greenberg ER, Polyp Prevention Study Group (2007) Folic acid for the prevention of colorectal adenomas: a randomized clinical trial. JAMA 297:2351–2359
Cross AJ, Ferrucci LM, Risch A, Graubard BI, Ward MH, Park Y, Hollenbeck AR, Schatzkin A, Sinha R (2010) A large prospective study of meat consumption and colorectal cancer risk: an investigation of potential mechanisms underlying this association. Cancer Res 70:2406–2414
Doi K, Wanibuchi H, Salim EI, Morimura K, Kinoshita A, Kudoh S, Hirata K, Yoshikawa J, Fukushima S (2005) Lack of large intestinal carcinogenicity of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine at low doses in rats initiated with azoxymethane. Int J Cancer 115:870–878
Ferlay J, Shin HR, Bray F, Forman D, Mathers CD, Parkin D (2010) GLOBOCAN 2008, Cancer incidence and mortality worldwide: IARC cancerbase No. 10. Lyon. International Agency for Research on Cancer, France. http://globocan.iarc.fr. Accessed 27 Oct 2011
Fife J, Raniga S, Hider PN, Frizelle FA (2011) Folic acid supplementation and colorectal cancer risk: a meta-analysis. Colorectal Dis 13:132–137
Fujise T, Iwakiri R, Kakimoto T, Shiraishi R, Sakata Y, Wu B, Tsunada S, Ootani A, Fujimoto K (2007) Long-term feeding of various fat diets modulates azoxymethane-induced colon carcinogenesis through Wnt/beta-catenin signaling in rats. Am J Physiol Gastrointest Liver Physiol 292:G1150–G1156
Fukushima S, Wanibuchi H, Morimura K, Iwai S, Nakae D, Kishida H, Tsuda H, Uehara N, Imaida K, Shirai T, Tatematsu M, Tsukamoto T, Hirose M, Furukawa F (2004) Existence of a threshold for induction of aberrant crypt foci in the rat colon with low doses of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Toxicol Sci 80:109–114
Furukawa F, Nishikawa A, Kitahori Y, Tanakamaru Z, Hirose M (2002) Spontaneous development of aberrant crypt foci in F344 rats. J Exp Clin Cancer Res 21:197–201
Gibson TM, Weinstein SJ, Pfeiffer RM, Hollenbeck AR, Subar AF, Schatzkin A, Mayne ST, Stolzenberg-Solomon R (2011) Pre- and postfortification intake of folate and risk of colorectal cancer in a large prospective cohort study in the United States. Am J Clin Nutr 94:1053–1062
Hasegawa R, Sano M, Tamano S, Imaida K, Shirai T, Nagao M, Sugimura T, Ito N (1993) Dose-dependence of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) carcinogenicity in rats. Carcinogenesis 14:2553–2557
Issa JP (2004) CpG island methylator phenotype in cancer. Nat Rev Cancer 4:988–993
Ito N, Hasegawa R, Sano M, Tamano S, Esumi H, Takayama S, Sugimura T (1991) A new colon and mammary carcinogen in cooked food, 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Carcinogenesis 12:1503–1506
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Kennedy DA, Stern SJ, Moretti M, Matok I, Sarkar M, Nickel C, Koren G (2011) Folate intake and the risk of colorectal cancer: a systematic review and meta-analysis. Cancer Epidemiol 35:2–10
Kim Y-I (1999) Will mandatory folic acid fortification prevent or promote cancer? Am J Clin Nutr 80:1123–1128
Kim Y-I (2003) Role of folate in colon cancer development and progression. J Nutr 133(Suppl 1):3731S–3739S
Kim Y-I (2004) Folate, colorectal carcinogenesis, and DNA methylation: lessons from animal studies. Environ Mol Mutagen 44:10–25
Kim Y-I, Salomon RN, Graeme-Cook F, Choi SW, Smith DE, James SJ, Mason JB (1996) Dietary folate protects against the development of macroscopic colonic neoplasia in a dose responsive manner in rats. Gut 39:732–740
Kim D-Y, Chung KH, Lee JH (1998) Stimulatory effects of high-fat diets on colon cell proliferation depend on the type of dietary fat and site of the colon. Nutr Cancer 30:118–123
Kühnel D, Taugner F, Scholtka B, Steinberg P (2009) Inflammation does not precede or accompany the induction of preneoplastic lesions in the colon of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine-fed rats. Arch Toxicol 83:763–768
Lee JE, Willett WC, Fuchs CS, Smith-Warner SA, Wu K, Ma J, Giovannucci E (2011) Folate intake and risk of colorectal cancer and adenoma: modification by time. Am J Clin Nutr 93:817–825
Lindzon G, Medline A, Sohn K-J, Depeint F, Croxford R, Kim Y-I (2009) Effect of folic acid supplementation on the progression of colorectal aberrant crypt foci. Carcinogenesis 30:1536–1543
Mason JB, Dickstein A, Jacques PF, Haggarty P, Selhub J, Dallal G, Rosenberg IH (2007) A temporal association between folic acid fortification and an increase in colorectal cancer rates may be illuminating important biological principles: a hypothesis. Cancer Epidemiol Biomarkers Prev 16:1325–1329
Nigro ND, Singh DV, Campbell RL, Sook M (1975) Effect of dietary beef fat on intestinal tumor formation by azoxymethane in rats. J Natl Cancer Inst 54:439–442
Ochiai M, Nakagama H, Watanabe M, Ishiguro Y, Sugimura T, Nagao M (1996) Efficient method for rapid induction of aberrant crypt foci in rats with 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Jpn J Cancer Res 87:1029–1033
Protiva P, Mason JB, Liu Z, Hopkins ME, Nelson C, Marshall JR, Lambrecht RW, Pendyala S, Kopelovich L, Kim M, Kleinstein SH, Laird PW, Lipkin M, Holt PR (2011) Altered folate availability modifies the molecular environment of the human colrectum: implications for colorectal carcinogenesis. Cancer Prev Res 4:530–543
Rao CV, Hirose Y, Indranie C, Reddy BS (2001) Modulation of experimental colon tumorigenesis by types and amounts of dietary fatty acids. Cancer Res 61:1927–1933
Reddy BS, Wang CX, Aliaga C, Rao CV, Lubet RA, Steele VE, Kelloff GJ (1996) Potential chemopreventive activity of perillyl alcohol and enhancement of experimental colon carcinogenesis by folic acid and genistein. Proc Am Assoc Cancer Res 37:A1849
Rohrmann S, Hermann S, Linseisen J (2009) Heterocyclic aromatic amine intake increases colorectal adenoma risk: findings from a prospective European cohort study. Am J Clin Nutr 89:1418–1424
Santarelli R, Pierre F, Corpet DE (2008) Processed meat and colorectal cancer: a review of epidemiologic and experimental evidence. Nutr Cancer 60:131–144
Scheppach W, Bingham S, Boutron-Ruault MC, Gerhardsson de Verdier M, Moreno V, Nagengast FM, Reifen R, Riboli E, Seitz HK, Wahrendorf J (1999) WHO consensus statement on the role of nutrition in colorectal cancer. Eur J Cancer Prev 8:57–62
Senate Commission on Food Safety of the German Research Foundation (1998) Heterocyclic aromatic amines. Opinion dated 14th and 15th December 1998
Shen L, Issa JP (2002) Epigenetics in colorectal cancer. Curr Opin Gastroenterol 18:68–73
Shin A, Shrubsole MJ, Ness RM, Wu H, Sinha R, Smalley WE, Shyr Y, Zheng W (2007) Meat and meat-mutagen intake, doneness preference and the risk of colorectal polyps: the Tennessee colorectal polyp study. Int J Cancer 121:136–142
Singh J, Hamid R, Reddy BS (1997) Dietary fat and colon cancer: modulation of cyclooxygenase-2 by types and amount of dietary fat during the postinitiation stage of colon carcinogenesis. Cancer Res 57:3465–3470
Sinha R, Kulldorff M, Chow WH, Denobile J, Rothman N (2001) Dietary intake of heterocyclic amines, meat-derived mutagenic activity, and risk of colorectal adenomas. Cancer Epidemiol Biomarkers Prev 10:559–562
Sinha R, Peters U, Cross AJ, Kulldorff M, Weissfeld JL, Pinsky PF, Rothman N, Hayes RB (2005) Meat, meat cooking methods and preservation, and risk for colorectal adenoma. Cancer Res 65:8034–8041
Stevens VL, McCullough ML, Sun J, Jacobs EJ, Campbell PT, Gapstur SM (2011) High levels of folate from supplements and fortification are not associated with increased risk of colorectal cancer. Gastroenterology 141:98–105
Thompson LH, Tucker JD, Stewart SA, Christensen ML, Salazar EP, Carrano AV, Felton JS (1987) Genotoxicity of compounds from cooked beef in repair-deficient CHO cells versus Salmonella mutagenicity. Mutagenesis 2:483–487
Thornton WH Jr, MacDonald RS (1997) Dietary fat quantity and composition induce changes in proliferation and membrane lipids in rat colon cells. Ann Nutr Metab 41:260–268
Tudek B, Bird RP, Bruce WR (1989) Foci of aberrant crypts in the colons of mice and rats exposed to carcinogens associated with foods. Cancer Res 49:1236–1240
Ubagai T, Ochiai M, Kawamori T, Imai H, Sugimura T, Nagao M, Nakagama H (2002) Efficient induction of rat large intestinal tumors with a new spectrum of mutations by intermittent administration of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine in combination with a high fat diet. Carcinogenesis 23:197–200
Wallace K, Grau MV, Levine J, Shen L, Hamdan R, Chen X, Gui J, Haile RW, Barry EL, Ahnen D, McKeown-Eyssen G, Baron JA, Issa JPJ (2010) Association between folate levels and CpG island hypermethylation in normal colorectal mucosa. Cancer Prev Res 3:1552–1564
Wargovich MJ, Chen CD, Jimenez A, Steele VE, Velasco M, Stephens LC, Price R, Gray K, Kelloff GJ (1996) Aberrant crypts as a biomarker for colon cancer: evaluation of potential chemopreventive agents in the rat. Cancer Epidemiol Biomarkers Prev 5:355–360
Wargovich MJ, Jimenez A, McKee K, Steele VE, Velasco M, Woods J, Price R, Gray K, Kelloff GJ (2000) Efficacy of potential chemopreventive agents on rat colon aberrant crypt formation and progression. Carcinogenesis 21:1149–1155
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington
Wu WK, Sung JJ, Lee CW, Yu J, Cho CH (2010) Cyclooxygenase-2 in tumorigenesis of gastrointestinal cancers: an update on the molecular mechanisms. Cancer Lett 295:7–16
Zheng W, Lee SA (2009) Well-done meat intake, heterocyclic amine exposure, and cancer risk. Nutr Cancer 61:437–446
Acknowledgments
This study was supported by a grant from the Federal Institute for Risk Assessment in Germany (grant FK 3-1329-303).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicken, P., Brauer, N., Lampen, A. et al. Influence of a fat-rich diet, folic acid supplementation and a human-relevant concentration of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine on the induction of preneoplastic lesions in the rat colon. Arch Toxicol 86, 815–821 (2012). https://doi.org/10.1007/s00204-012-0819-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-012-0819-1