Abstract
The aim of the present work was to investigate possible protective effects of febuxostat, a highly potent xanthine oxidase inhibitor, against acute lung injury (ALI) induced by lipopolysaccharide (LPS) in rats. Male Sprague Dawley rats were randomly divided into six groups, as follows: (i) vehicle control group; (ii) and (iii) febuxostat 10 and febuxostat 15 groups, drug-treated controls; (iv) LPS group, receiving an intraperitoneal injection of LPS (7.5 mg/kg); (v) and (vi) febuxostat 10-LPS and febuxostat 15-LPS groups, receiving oral treatment of febuxostat (10 and 15 mg/kg/day, respectively) for 7 days before LPS. After 18 h administration of LPS, blood was collected for C-reactive protein (CRP) measurement. Bronchoalveolar lavage fluid (BALF) was examined for leukocyte infiltration, lactate dehydrogenase (LDH) activity, protein content, and total nitrate/nitrite. Lung weight gain was determined, and lung tissue homogenate was prepared and evaluated for oxidative stress. Tumor necrosis factor-α (TNF-α) was assessed in BALF and lung homogenate. Moreover, histological changes of lung tissues were evaluated. LPS elicited lung injury characterized by increased lung water content (by 1.2 fold), leukocyte infiltration (by 13 fold), inflammation and oxidative stress (indicated by increased malondialdehyde (MDA), by 3.4 fold), and reduced superoxide dismutase (SOD) activity (by 34 %). Febuxostat dose-dependently decreased LPS-induced lung edema and elevations in BALF protein content, infiltration of leukocytes, and LDH activity. Moreover, the elevated levels of TNF-α in BALF and lung tissue of LPS-treated rats were attenuated by febuxostat pretreatment. Febuxostat also displayed a potent antioxidant activity by decreasing lung tissue levels of MDA and enhancing SOD activity. Histological analysis of lung tissue further demonstrated that febuxostat dose-dependently reversed LPS-induced histopathological changes. These findings demonstrate a significant dose-dependent protection by febuxostat against LPS-induced lung inflammation in rats.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) and its more severe form, the acute respiratory distress syndrome (ARDS), are common causes of acute respiratory failure. The ALI/ARDS may develop due to a direct injury to lung, mediated by insults such as pneumonia and aspiration, as well as indirect mechanisms, such as sepsis (Ware and Matthay 2000). ALI is a disorder of acute inflammation that causes disturbance of the lung endothelial and epithelial barriers (Bhatia and Moochhala 2004). Cellular characteristics of ALI involve loss of alveolar-capillary membrane integrity, excessive trans-epithelial neutrophil migration, and liberation of pro-inflammatory cytotoxic mediators (Matthay and Zimmerman 2005; Ware and Matthay 2000).
Lipopolysaccharide (LPS), also known as endotoxin, is the key component of the outer membrane of gram-negative bacteria (Brigham and Meyrick 1986). LPS-induced lung injury in experimental animals is a very useful in vivo model closely resembling ALI/ARDS in humans (Kabir et al. 2002; Matute-Bello et al. 2008). Exposure to LPS, either by inhalation or via systemic administration (intravenous and intraperitoneal), elicits major features of microvascular lung injury, including leukocyte accumulation in the lung tissue, pulmonary edema, profound lung inflammation, and mortality (Gao et al. 2004; Kabir et al. 2002; Shen et al. 2009).
The inflammatory milieu of LPS-induced ALI is complex, comprising epithelial cells, neutrophils, alveolar macrophages, pro-inflammatory mediators, proteolytic enzymes, and reactive oxygen species (ROS) (Kabir et al. 2002). LPS binds Toll-like receptor-4 (TLR-4) on the airway epithelium, leading to the activation of the transcription factor nuclear factor-kappa B (NF-κB), which enhances the production of pro-inflammatory cytokines and chemokines, including tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), IL-6, and monocyte chemotactic protein-1 (MCP-1) that mediate leukocyte infiltration (Zhang and Ghosh 2000). These cytokines also contribute to excess ROS generation, producing oxidative stress, which plays a central role in the progression of ALI-associated inflammation (Berkow and Dodson 1988).
Xanthine oxidase is one of the major enzymatic pathways that generate ROS during inflammatory conditions and oxidative stress (Nomura et al. 2013). It catalyzes the oxidation of purine substrates, such as xanthine and hypoxanthine, producing uric acid and ROS (Berry and Hare 2004). Xanthine oxidase has been suggested to participate in the pathogenesis of lung injury. The activity of xanthine oxidase exhibited a 400-fold increase in the bronchoalveolar lavage fluid (BALF) of mice infected with the influenza virus (Akaike et al. 1990). Moreover, the activity and expression of xanthine oxidase have been reported to be up-regulated in the lung tissue by various inflammatory stimuli such as LPS, hypoxia, and cytokines (Hassoun et al. 1998; Nomura et al. 2013). Furthermore, inhibition/inactivation of xanthine oxidase attenuated ischemia/reperfusion-induced lung injury in rabbit (Adkins and Taylor 1990; Nielsen et al. 1996) and rat (Poggetti et al. 1992). However, pretreatment of endotoxemic mice with the xanthine oxidase inhibitor allopurinol failed to inhibit LPS-induced pulmonary neutrophil infiltration or pro-inflammatory cytokine overexpression by lung neutrophils (Shenkar and Abraham 1999).
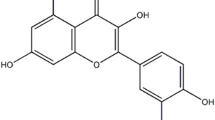
Febuxostat is a selective and potent inhibitor of xanthine oxidase (Okamoto et al. 2003), which has been reported to have antioxidant and anti-inflammatory effects in various disease models (Hwang et al. 2014; Nomura et al. 2014; Omori et al. 2012; Tsuda et al. 2012), presumably via inhibition of ROS production. Recently, febuxostat has also been shown to inhibit LPS-induced expression of MCP-1, independently of its effect on uric acid level, in human macrophages in vitro (Nomura et al. 2013). Therefore, the present study aimed to investigate the possible protective effects of febuxostat against LPS-induced ALI in rats. Probable mechanisms involved in febuxostat-mediated effects were also studied.
Materials and methods
Experimental animals
Male Sprague Dawley rats (200–250 g) were used. The animals were housed in an air-conditioned room maintained at 25 ± 2 °C with regular 12 h light/12 h dark cycle. They were allowed free access to standard food and water. The experiments were conducted in accordance with the ethical guidelines for investigations in laboratory animals and were approved by the Ethical Committee of Faculty of Pharmacy, Mansoura University, Egypt.
Drugs and chemicals
LPS (Escherichia coli serotype O111:B4) was purchased from Sigma Chemical Co. (St. Louis, MO, USA). The LPS solutions were freshly prepared in sterile pyrogen-free saline (0.9 %) on the day of experiment. Febuxostat was obtained in the form of a pharmaceutical product (Febucip (80 mg/tablet), Cipla Limited, India) and was given as a solution in distilled water. All other chemicals used in the current study were of fine analytical grade.
Experimental protocol
Rats were randomly divided into six groups each of six animals as follows:
Control group: received a 7-day oral treatment of distilled water (2 ml/kg) followed by an intraperitoneal injection of sterile pyrogen-free saline (0.9 %, 2 ml/kg) on the eighth day.
Febuxostat 10 and febuxostat 15 groups: received a 7-day oral treatment of febuxostat (10 and 15 mg/kg/day, respectively) followed by an intraperitoneal injection of sterile pyrogen-free saline (0.9 %, 2 ml/kg) on the eighth day.
LPS group: received a 7-day oral treatment of distilled water (2 ml/kg). On the eighth day, ALI was induced by a single intraperitoneal injection of LPS (7.5 mg/kg), as previously reported (Brauer et al. 2000; Lu et al. 2002).
Febuxostat 10-LPS and febuxostat 15-LPS groups: received a 7-day oral treatment of febuxostat (10 and 15 mg/kg/day, respectively) followed by an intraperitoneal injection of LPS (7.5 mg/kg) on the eighth day.
Selection of doses of febuxostat in the current study was based on previously reported doses in animal studies (Hwang et al. 2014; Tsuda et al. 2012), with a slight modification.
After 18 h of LPS/saline injection, blood was collected via retro-orbital puncture under light ether anesthesia, and serum was separated by centrifugation for 20 min at 1000×g for determination of C-reactive protein (CRP). Rats were sacrificed by cervical dislocation. The chest was immediately opened and the trachea was exposed and cannulated. The left main bronchus was tied with a hemostatic clamp, and BALF was collected from the right lung by intratracheal injection of 1 ml of ice-cold sterile 0.9 % saline six times followed by gentle aspiration. The recovered BALF fractions were pooled and centrifuged (1000×g, 10 min, 4 °C) using a cooling centrifuge (Damon/IEC Division, model CRU-5000, Needham, MA, USA) to collect the cell pellet for total cell count determination. The cell-free supernatant of BALF was stored at −80 °C for assessment of protein content, lactate dehydrogenase (LDH) activity, total nitrate/nitrite (NOx), and TNF-α.
Moreover, the left lungs were harvested, washed, and perfused with ice-cold saline and processed for determination of wet/dry (W/D) lung weight ratio and histological evaluation. In a separate set of experiments, animals received the same treatments and the right lungs were removed for homogenate preparation.
BALF biochemical parameters
Determination of the protein content of BALF
The total protein concentration in BALF was assessed using a commercial kit (Biodiagnostic, Giza, Egypt).
Measurement of LDH activity in BALF
LDH activity in BALF was evaluated using a commercial kit (Biosystems S.A., Barcelona, Spain), based on its ability to catalyze the reduction of pyruvate, in the presence of nicotinamide adenine dinucleotide hydride (NADH), to form lactate and NAD+. The catalytic concentration was determined from the rate of decrease of NADH in the reaction medium, measured at 340 nm.
Measurement of NOx in BALF
The levels of total nitrite and nitrate, the stable metabolites of nitric oxide (NO), in BALF were assessed using a commercial assay kit (R and D Systems, Minneapolis, MN, USA). Briefly, the nitrate content was reduced to nitrite by incubation of samples with nitrate reductase and NADH at 37 °C for 30 min. The total nitrite was then determined colorimetrically as an azo dye product of the Griess reaction. The absorbance was measured at 540 nm, and the total NOx levels were calculated from the linear regression of sodium nitrate standard curve (Bories and Bories 1995; Granger et al. 1996).
Measurement of lung W/D weight ratio
The magnitude of pulmonary edema was evaluated by determining the W/D ratio of lung tissues. The left lower lung lobe was removed, rinsed with saline, blotted, and weighed to obtain the wet weight. The lung was then dried at 80 °C for 24 h and weighed to obtain the dry weight. The W/D ratio was then calculated.
Preparation of lung tissue homogenates
The right lung tissues of the rats were rapidly removed and immediately homogenized in 10 volumes of 50 mM phosphate buffer (pH 7.4) at 4 °C using a variable-speed homogenizer (Omni international, USA). Lung homogenates were centrifuged for 15 min at 1000×g, 4 °C to obtain supernatants, which were used for measurement of oxidative stress-related parameters and TNF-α.
Assessment of oxidative stress in lung homogenate
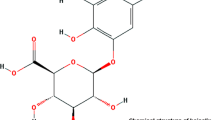
Commercially available kits (glutathione-reduced, lipid peroxides (MDA), and superoxide dismutase) from Biodiagnostic (Giza, Egypt) were used for accurate determination of the lung tissue levels of reduced glutathione (GSH), malondialdehyde (MDA), an index of lipid peroxidation, and superoxide dismutase (SOD) activity, respectively, according to the manufacturer’s instructions. The level of GSH in the lung was assayed colorimetrically, based on its ability to reduce [5,5′ dithiobis (2-nitrobenzoic acid), DTNB] (Beutler et al. 1963). MDA concentration was determined as thiobarbituric acid reactive substances formed by its reaction with thiobarbituric acid in acidic medium at 95 °C (Satoh 1978). SOD activity was assessed based on the ability of SOD to inhibit the phenazine methosulfate-mediated reduction of nitroblue tetrazolium dye (Nishikimi et al. 1972).
Determination of TNF-α level
The levels of TNF-α in the supernatants of the lung homogenate and BALF were assayed using rat TNF-α Platinum ELISA kit (eBioscience, San Diego, CA, USA) according to the manufacturer’s instructions. The concentrations of TNF-α in samples were determined from a 5-parameter fit of the standard curve constructed using a standard provided with the kit.
Histopathological examination
The upper left lung lobe from each animal was immediately fixed in 10 % neutral buffered formalin. Lungs were gradually dehydrated, embedded in paraffin, cut into 4-μm sections and stained with hematoxylin and eosin (H&E). Lung specimens were evaluated for histological alterations characteristic of ALI, which included alveolar congestion, hemorrhage, neutrophil infiltration, the thickness of the alveolar wall, and interstitial edema. The results were scored semi-quantitatively on a scale of 0–3 for each item, as previously described (Shen et al. 2009; Yao et al. 2006), where 0 = minimal damage, 1 = mild damage, 2 = moderate damage, and 3 = severe damage. The five variables were summed to represent the total lung injury score, ranging from 0 to 15. Grading was performed by a pathologist who was unaware of the experimental design of the present study.
Statistical analysis
Data are expressed as mean ± SEM. Statistical analysis was performed using one-way analysis of variance (ANOVA) followed by Tukey–Kramer multiple comparisons test. Histopathological scores were compared using Kruskal–Wallis followed by Dunn’s multiple comparison test. A P value < 0.05 was considered as statistically significant. Statistical analyses were carried out using Graphpad Prism software (GraphPad Software Inc. V4.03, San Diego, CA, USA).
Results
Effect of febuxostat on serum CRP level in rats with LPS-induced ALI
Intraperitoneal administration of LPS caused acute inflammation, indicated by a significant elevation in serum CRP level (P < 0.0001 versus control group). Pretreatment of rats with febuxostat (10 and 15 mg/kg/day) restored CRP concentration to near-normal levels of control group (P > 0.05). These results are shown in Fig. 1.
Effects of febuxostat on serum C-reactive protein (CRP) in rats with lipopolysaccharide (LPS)-induced acute lung injury. Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, serum was obtained to assess CRP level. Data are represented as means ± SEM, n = 6 in each group. #### P < 0.0001 versus control group, **** P < 0.0001 versus LPS-treated group
Effect of febuxostat on lung W/D weight ratio in rats with LPS-induced ALI
The lung W/D weight ratio is a commonly used approach for assessment of experimental lung edema. Compared with control animals, injection of LPS caused a significant increase (P < 0.05) in the lung W/D ratio. Pretreatment of rats with febuxostat (15 mg/kg/day) prevented the LPS-induced elevation in the lung W/D ratio (P > 0.05 versus control group, P < 0.01 versus LPS-treated group). These results are shown in Fig. 2.
Effects of febuxostat (10 and 15 mg/kg) on lung wet/dry (W/D) weight ratio in rats with lipopolysaccharide (LPS)-induced acute lung injury. Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, lung tissue samples were collected for determination of the lung W/D weight ratio. Data are represented as means ± SEM of six rats in each group. # P < 0.05 versus control group, ** P < 0. 01 versus LPS-treated group
Effect of febuxostat on protein content and total cell count in BALF of rats with LPS-induced ALI
Rats challenged with LPS exhibited an increased capillary leakage, as shown by a significant increase of BALF protein concentration (Fig. 3a) and total cell count (Fig. 3b). These LPS-induced changes were significantly attenuated by pretreatment with febuxostat (10 and 15 mg/kg/day) in a dose-dependent manner.
Effects of febuxostat on protein content (a) and total cell count (b) in bronchoalveolar lavage fluid (BALF) of rats with lipopolysaccharide (LPS)-induced acute lung injury. Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, BALF samples were obtained to assess total protein content and total cell count. Data are represented as means ± SEM of six rats in each group. # P < 0.05 and #### P < 0.0001 versus control group, ** P < 0. 01 and **** P < 0.0001 versus LPS-treated group, $$ P < 0.01 versus febuxostat 10-LPS group
Effect of febuxostat on LDH activity and total NOx levels in BALF of rats with LPS-induced ALI
The BALF of LPS-treated rats showed significant elevations of LDH activity (P < 0.01, Fig. 4a) and total NOx (P < 0.0001, Fig. 4b) in comparison with control rats. Pretreatment with febuxostat dose-dependently reduced the elevated levels of LDH and NOx in LPS-treated rats.
Effects of febuxostat on lactate dehydrogenase (LDH) activity (a) and total nitrite/nitrate (b) in bronchoalveolar lavage fluid (BALF) of rats with lipopolysaccharide (LPS)-induced acute lung injury. Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, BALF samples were prepared to assess LDH and nitrate/nitrite levels. Data are represented as means ± SEM, n = 6 in each group. ## P < 0.01 and #### P < 0.0001 versus control group, ** P < 0. 01 versus LPS-treated group
Effect of febuxostat on oxidative stress parameters in lung tissues of rats with LPS-induced ALI
Administration of LPS in rats elicited a significant increase in MDA (P < 0.01) and significant reductions in GSH (P ˂ 0.0001) and SOD activity (P < 0.01) levels compared to control rats. Pretreatment with febuxostat (15 mg/kg/day) reversed LPS-induced increase in MDA levels and abolished LPS-mediated decrease of SOD activity. However, it failed to reverse the depleted GSH level in lung tissues of LPS-treated rats. These results are shown in Fig. 5.
Effects of febuxostat on oxidative stress parameters in lung tissue homogenates of rats with lipopolysaccharide (LPS)-induced acute lung injury. a Malondialdehyde (MDA), b glutathione (GSH), and c superoxide dismutase (SOD). Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, lung homogenates were prepared to assess MDA, GSH, and SOD. Data are represented as means ± SEM of six rats in each group. ## P < 0.01 and #### P < 0.0001 versus control group, ** P < 0. 01 and **** P < 0.0001 versus LPS-treated group
Effect of febuxostat on TNF-α level in BALF and lung tissue homogenate of rats with LPS-induced ALI
Levels of TNF-α in the BALF and lung tissues of LPS-treated rats were significantly increased compared to control animals. The elevation of TNF-α level in LPS-challenged rats was significantly reduced by pretreatment with febuxostat (10 and 15 mg/kg/day, Fig. 6).
Effects of febuxostat on tumor necrosis factor-α (TNF-α) level in bronchoalveolar lavage fluid (BALF) (a) and lung tissue homogenate (b) of rats with lipopolysaccharide (LPS)-induced acute lung injury. Febuxostat (10 and 15 mg/kg/day, orally) was administrated for 7 days prior to LPS administration (7.5 mg/kg, intraperitoneal). After 18 h of LPS challenge, lung homogenates and BALF samples were prepared to assess TNF-α concentration. Data are represented as means ± SEM of six rats in each group. ## P < 0.01 and #### P < 0.0001 versus control group, ** P < 0. 01 and **** P < 0.0001 versus LPS-treated group
Effect of febuxostat on lung histology of rats with LPS-induced ALI
In contrast to control rats (Fig. 7a) and febuxostat control groups (Fig. 7b, c), which exhibited normal pulmonary histology, lung tissues from LPS-treated (Fig. 7d) rats were substantially damaged, showing marked interstitial edema, congestion, hemorrhage, alveolar wall thickening, and infiltration of inflammatory cells into the interstitial and alveolar spaces. These histological changes were dose-dependently attenuated in the groups pretreated with 10 (Fig. 7e) and 15 (Fig. 7f) mg/kg/day febuxostat. The histological features of ALI in lung tissues of experimental groups were semi-quantitatively graded, and the scores were summed to provide a total lung injury score for each rat. The total lung injury scores in febuxostat 10-LPS (3–7; median = 5.5) and febuxostat 15-LPS (2–3; median = 3) groups were lower than that in the non-treated LPS group (9–14; median = 11), indicating a dose-dependent protection of febuxostat pretreatment against LPS-induced lung injury. These results are shown in Fig. 8.
Representative images of hematoxylin and eosin (H&E)-stained lung tissues from control (a), febuxostat control (10 and 15 mg/kg/day; b and c, respectively), LPS-challenged (d) and febuxostat-LPS (10 and 15 mg/kg/day; e and f, respectively) groups. Arrows indicate neutrophil infiltration. Images were captured at ×400 magnification
Scatter dot plots of the histopathological assessment scores of lung injury in control, LPS-challenged, and febuxostat-treated (10 and 15 mg/kg) rats. Lung injury was graded from 0 (normal) to 3 (severe) in five categories: alveolar congestion, hemorrhage, edema, thickness of the alveolar wall, and inflammatory cell infiltration. The total lung injury score was calculated by adding up the individual scores of all categories. The median of each data set is indicated. # P < 0.05 versus control group using Kruskal–Wallis followed by Dunn’s multiple comparison test
Discussion
LPS has been shown to induce acute pulmonary injury in rats (Gao et al. 2004; Shen et al. 2009). In the current study, intraperitoneal injection of LPS in rats was used to provoke ALI, which was demonstrated by marked increases in lung W/D weight ratio (indicating lung edema), BALF total cells (indicating lung inflammation through the migration and activation of inflammatory cells), and BALF total proteins (indicating increased permeability of the bronchoalveolar-capillary barrier and subsequent leakage of protein-rich edema fluid into interstitial and alveolar spaces) (Hakansson et al. 2012; Wang et al. 2011). ALI was also histologically confirmed in LPS-treated rats. The present study primarily demonstrates that pretreatment with febuxostat dose-dependently ameliorated LPS-induced ALI in rats, an effect that is possibly mediated via attenuation of oxidative stress and inflammation in the lung milieu of LPS-challenged rats.
LPS injection resulted in a significant oxidative stress in lung tissues, as evidenced by an elevation of lipid peroxidation and significant decreases in SOD activity and GSH levels. Oxidative stress-induced damage is a major contributor to the pathogenesis of ALI (Imai et al. 2008). Activation of neutrophils during lung injury results in excessive production of oxygen radicals, which ultimately leads to alteration in lung function parameters (Guo and Ward 2007). Although several antioxidant enzyme systems are induced in the course of ALI, natural host defenses fail to increase antioxidant capacity, which inevitably results in the damaging sequelae of ALI (Kozar et al. 2000).
In the current investigation, febuxostat displayed potent antioxidant properties against LPS-induced oxidative stress, where it reduced lung lipid peroxidation and counteracted the LPS-induced decease in SOD activity. This is consistent with previous studies showing strong antioxidant effects of febuxostat (Omori et al. 2012; Tsuda et al. 2012). Febuxostat has also been shown to decrease the levels of ROS and MDA in aortas of atherosclerotic mice and streptozocin-diabetic rats, respectively (Hwang et al. 2014; Nomura et al. 2014). Moreover, febuxostat has also been demonstrated to attenuate, more effectively than prototypical xanthine oxidase inhibitors allopurinol and oxypurinol, LPS-induced intracellular ROS formation in human macrophages (Nomura et al. 2013). Febuxostat, but not allopurinol, was able to reduce oxidative stress in high-risk cardiac surgery patients with hyperuricemia (Sezai et al. 2013). Paradoxically, febuxostat failed to reverse LPS-induced depletion of lung GSH. A possible explanation is that the antioxidant effect of febuxostat may be mediated via other mechanisms than enhancing intracellular GSH concentration. These may include inhibition of xanthine oxidase-derived ROS (Nomura et al. 2014; Nomura et al. 2013), direct inactivation of ROS through activation of SOD and attenuation of oxidant production by preventing alveolar infiltration of neutrophils.
The protective effects of febuxostat in the current experimental setting may be also related to its ability to reduce the LPS-dependent elevation of BALF NO level (Fig. 4b). Increases in pulmonary NO have been implicated in the pathogenesis of LPS-induced inflammation, oxidative stress, and cytotoxicity (Crespo et al. 1999; Gao et al. 2004; Wright et al. 1992; Yeh et al. 2007). NO has been shown to react with superoxide anion, forming peroxynitrite anion, which can decompose to generate hydroxyl radicals (Beckman et al. 1990). It can also react with protein tyrosine residues to form nitrotyrosine, a stable oxidation product. This reaction can alter cell signaling processes, resulting in apoptosis and subsequent dysfunction of microvascular endothelial barrier (Blaylock et al. 1998; Gu et al. 2000; Sittipunt et al. 2001). LPS-mediated overproduction of NO has been attributed to an increased expression of the inducible isoform of NO synthase (iNOS) (Crespo et al. 1999; Gao et al. 2004; Yeh et al. 2007). Whether febuxostat attenuates NO production in LPS-challenged rats via inhibition of iNOS expression needs to be explored in future investigations.
Data in the current study also suggest that febuxostat pretreatment mitigates LPS-induced inflammation. Febuxostat-treated groups showed significant reductions in W/D lung weight ratio and BALF cell count and protein content compared to LPS group. Moreover, as demonstrated by histological evaluation of lung tissues, febuxostat administration attenuated the diffuse inflammatory cell infiltration in lungs of LPS-challenged rats. Collectively, these effects support an anti-inflammatory effect of febuxostat.
Furthermore, febuxostat suppressed the elevations of serum CRP and TNF-α level in BALF and lung homogenate of LPS-challenged rats. Previous studies have demonstrated pulmonary overproduction of TNF-α after LPS exposure, suggesting that it is involved in the pathogenesis of LPS-induced ALI (Chen et al. 2010; Shi et al. 2010; Yeh et al. 2007). TNF-α has been shown to activate neutrophils, stimulating their adhesion to endothelial cell surface, and to up-regulate the expression of adhesion molecules on circulating neutrophils and endothelial cells (Bhatia and Moochhala 2004). Moreover, TNF-α enhances ROS production and chemotactic factors by neutrophils (Berkow and Dodson 1988). It is therefore possible that the anti-inflammatory effect of febuxostat in LPS-induced ALI involves the suppression of the pro-inflammatory TNF-α and possibly other cytokines, in the lung tissue and neutrophils. Supporting this notion, febuxostat inhibited LPS-induced TNF-α and MCP-1 expression in human macrophages (Nomura et al. 2013). Febuxostat has also been reported to attenuate the expression of pro-inflammatory cytokine genes in aortas of atherosclerotic mice (Nomura et al. 2014) and in ischemia–reperfusion injured rat kidneys (Tsuda et al. 2012). Febuxostat-mediated anti-inflammatory effects are potentially related to its ability to limit oxidative stress. ROS are known to induce the expression of inflammation-related cytokines, which in turn promote the infiltration of inflammatory cells and subsequent further ROS generation by infiltrated neutrophils (Bhatia and Moochhala 2004; Guo and Ward 2007; Li et al. 2014).
LPS injection also resulted in lung tissue damage, as evidenced by high BALF levels of the cytosolic enzyme, LDH, an indicator of cytotoxicity (Henderson et al. 1979). Febuxostat administration to LPS-treated rats attenuated the elevated LDH level, which suggests a cytoprotective effect. Evaluation of the lung tissues further demonstrated that febuxostat was effective in protecting against LPS-induced histological alterations.
Two dose levels of febuxostat (10 and 15 mg/kg/day) were used in the current study, of which the latter dose appears to be more effective in protection against LPS-induced ALI. Whereas febuxostat was administered at doses of 5 or 10 mg/kg/day in previous studies in rats (Hwang et al. 2014; Tsuda et al. 2012), the need to increase the dose of febuxostat in the present study may be related the short duration of pretreatment (7 days) and/or due to the likely alteration of febuxostat pharmacokinetics in endotoxemic rats (De Paepe et al. 2002). Nevertheless, chronic toxicology studies have shown that the use of febuxostat at a daily dose of 15 mg/kg/day is safe in rats (Takeda Pharmaceuticals America 2009).
In conclusion, data from the current study further support, and extend to in vivo conditions, the recently reported protective effects of febuxostat against LPS-induced inflammation and oxidative stress in human macrophages (Nomura et al. 2013). The present results clearly demonstrates that pretreatment with febuxostat dose-dependently attenuated ALI-associated vascular permeability, pulmonary edema, and lung histopathological alterations. Future studies are required to assess whether febuxostat could offer a therapeutic potential after LPS-induced ALI has already been established. Moreover, further clinical studies should be conducted to evaluate the protective potential of febuxostat in patients at high risk of developing ALI.
References
Adkins WK, Taylor AE (1990) Role of xanthine oxidase and neutrophils in ischemia-reperfusion injury in rabbit lung. J Appl Physiol (1985) 69:2012–2018
Akaike T, Ando M, Oda T, Doi T, Ijiri S, Araki S, Maeda H (1990) Dependence on O2- generation by xanthine oxidase of pathogenesis of influenza virus infection in mice. J Clin Invest 85:739–745
Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA (1990) Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci U S A 87:1620–1624
Berkow RL, Dodson MR (1988) Biochemical mechanisms involved in the priming of neutrophils by tumor necrosis factor. J Leukoc Biol 44:345–352
Berry CE, Hare JM (2004) Xanthine oxidoreductase and cardiovascular disease: molecular mechanisms and pathophysiological implications. J Physiol 555:589–606
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Bhatia M, Moochhala S (2004) Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol 202:145–156
Blaylock MG, Cuthbertson BH, Galley HF, Ferguson NR, Webster NR (1998) The effect of nitric oxide and peroxynitrite on apoptosis in human polymorphonuclear leukocytes. Free Radic Biol Med 25:748–752
Bories PN, Bories C (1995) Nitrate determination in biological fluids by an enzymatic one-step assay with nitrate reductase. Clin Chem 41:904–907
Brauer RB, Gegenfurtner C, Neumann B, Stadler M, Heidecke CD, Holzmann B (2000) Endotoxin-induced lung inflammation is independent of the complement membrane attack complex. Infect Immun 68:1626–1632
Brigham KL, Meyrick B (1986) Endotoxin and lung injury. Am Rev Respir Dis 133:913–927
Chen Z, Zhang X, Chu X, Song K, Jiang Y, Yu L, Deng X (2010) Preventive effects of valnemulin on lipopolysaccharide-induced acute lung injury in mice. Inflammation 33:306–314
Crespo E, Macias M, Pozo D, Escames G, Martin M, Vives F, Guerrero JM, Acuna-Castroviejo D (1999) Melatonin inhibits expression of the inducible NO synthase II in liver and lung and prevents endotoxemia in lipopolysaccharide-induced multiple organ dysfunction syndrome in rats. FASEB J 13:1537–1546
De Paepe P, Belpaire FM, Buylaert WA (2002) Pharmacokinetic and pharmacodynamic considerations when treating patients with sepsis and septic shock. Clin Pharmacokinet 41:1135–1151
Gao J, Zeng BX, Zhou LJ, Yuan SY (2004) Protective effects of early treatment with propofol on endotoxin-induced acute lung injury in rats. Br J Anaesth 92:277–279
Granger DL, Taintor RR, Boockvar KS, Hibbs Jr JB (1996) Measurement of nitrate and nitrite in biological samples using nitrate reductase and griess reaction. Methods Enzymol 268:142–151
Gu Z, Ling Y, Cong B (2000) Peroxynitrite mediated acute lung injury induced by lipopolysaccharides in rats. Zhonghua Yi Xue Za Zhi 80:58–61
Guo RF, Ward PA (2007) Role of oxidants in lung injury during sepsis. Antioxid Redox Signal 9:1991–2002
Hakansson HF, Smailagic A, Brunmark C, Miller-Larsson A, Lal H (2012) Altered lung function relates to inflammation in an acute LPS mouse model. Pulm Pharmacol Ther 25:399–406
Hassoun PM, Yu FS, Cote CG, Zulueta JJ, Sawhney R, Skinner KA, Skinner HB, Parks DA, Lanzillo JJ (1998) Upregulation of xanthine oxidase by lipopolysaccharide, interleukin-1, and hypoxia. Role in acute lung injury. Am J Respir Crit Care Med 158:299–305
Henderson RF, Rebar AH, Pickrell JA, Newton GJ (1979) Early damage indicators in the lung. III. Biochemical and cytological response of the lung to inhaled metals salts. Toxicol Appl Pharmacol 50:123–136
Hwang SJ, Lee KH, Jang HH, Lee SR, Woo JS, Lee HJ, Jung KH, Kim W (2014) Febuxostat contributes to improvement of endothelial dysfunction in an experimental model of streptozocin-induced diabetic rats. Int J Cardiol 171:e110–e112
Imai Y, Kuba K, Neely GG, Yaghubian-Malhami R, Perkmann T, van Loo G, Ermolaeva M, Veldhuizen R, Leung YH, Wang H, Liu H, Sun Y, Pasparakis M, Kopf M, Mech C, Bavari S, Peiris JS, Slutsky AS, Akira S, Hultqvist M, Holmdahl R, Nicholls J, Jiang C, Binder CJ, Penninger JM (2008) Identification of oxidative stress and toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell 133:235–249
Kabir K, Gelinas JP, Chen M, Chen D, Zhang D, Luo X, Yang JH, Carter D, Rabinovici R (2002) Characterization of a murine model of endotoxin-induced acute lung injury. Shock 17:300–303
Kozar RA, Weibel CJ, Cipolla J, Klein AJ, Haber MM, Abedin MZ, Trooskin SZ (2000) Antioxidant enzymes are induced during recovery from acute lung injury. Crit Care Med 28:2486–2491
Li W, Huang H, Niu X, Fan T, Hu H, Li Y, Yao H, Li H, Mu Q (2014) Tetrahydrocoptisine protects rats from LPS-induced acute lung injury. Inflammation 37:2106–2115
Lu MY, Kang BH, Wan FJ, Chen CS, Huang KL (2002) Hyperbaric oxygen attenuates lipopolysaccharide-induced acute lung injury. Intensive Care Med 28:636–641
Matthay MA, Zimmerman GA (2005) Acute lung injury and the acute respiratory distress syndrome: four decades of inquiry into pathogenesis and rational management. Am J Respir Cell Mol Biol 33:319–327
Matute-Bello G, Frevert CW, Martin TR (2008) Animal models of acute lung injury. Am J Physiol Lung Cell Mol Physiol 295:L379–L399
Nielsen VG, Tan S, Weinbroum A, McCammon AT, Samuelson PN, Gelman S, Parks DA (1996) Lung injury after hepatoenteric ischemia-reperfusion: role of xanthine oxidase. Am J Respir Crit Care Med 154:1364–1369
Nishikimi M, Appaji N, Yagi K (1972) The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem Biophys Res Commun 46:849–854
Nomura J, Busso N, Ives A, Matsui C, Tsujimoto S, Shirakura T, Tamura M, Kobayashi T, So A, Yamanaka Y (2014) Xanthine oxidase inhibition by febuxostat attenuates experimental atherosclerosis in mice. Sci Rep 4:4554
Nomura J, Busso N, Ives A, Tsujimoto S, Tamura M, So A, Yamanaka Y (2013) Febuxostat, an inhibitor of xanthine oxidase, suppresses lipopolysaccharide-induced MCP-1 production via MAPK phosphatase-1-mediated inactivation of JNK. PLoS one 8:e75527
Okamoto K, Eger BT, Nishino T, Kondo S, Pai EF (2003) An extremely potent inhibitor of xanthine oxidoreductase. Crystal structure of the enzyme-inhibitor complex and mechanism of inhibition. J Biol Chem 278:1848–1855
Omori H, Kawada N, Inoue K, Ueda Y, Yamamoto R, Matsui I, Kaimori J, Takabatake Y, Moriyama T, Isaka Y, Rakugi H (2012) Use of xanthine oxidase inhibitor febuxostat inhibits renal interstitial inflammation and fibrosis in unilateral ureteral obstructive nephropathy. Clin Exp Nephrol 16:549–556
Poggetti RS, Moore FA, Moore EE, Koeike K, Banerjee A (1992) Simultaneous liver and lung injury following gut ischemia is mediated by xanthine oxidase. J Trauma 32:723–727 discussion 727-728
Satoh K (1978) Serum lipid peroxide in cerebrovascular disorders determined by a new colorimetric method. Clin Chim Acta 90:37–43
Sezai A, Soma M, Nakata K, Hata M, Yoshitake I, Wakui S, Hata H, Shiono M (2013) Comparison of febuxostat and allopurinol for hyperuricemia in cardiac surgery patients (NU-FLASH Trial). Circ J 77:2043–2049
Shen W, Gan J, Xu S, Jiang G, Wu H (2009) Penehyclidine hydrochloride attenuates LPS-induced acute lung injury involvement of NF-kappaB pathway. Pharmacol Res 60:296–302
Shenkar R, Abraham E (1999) Mechanisms of lung neutrophil activation after hemorrhage or endotoxemia: roles of reactive oxygen intermediates, NF-kappa B, and cyclic AMP response element binding protein. J Immunol 163:954–962
Shi JR, Mao LG, Jiang RA, Qian Y, Tang HF, Chen JQ (2010) Monoammonium glycyrrhizinate inhibited the inflammation of LPS-Induced acute lung injury in mice. Int Immunopharmacol 10:1235–1241
Sittipunt C, Steinberg KP, Ruzinski JT, Myles C, Zhu S, Goodman RB, Hudson LD, Matalon S, Martin TR (2001) Nitric oxide and nitrotyrosine in the lungs of patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 163:503–510
Takeda Pharmaceuticals America (2009) Uloric (febuxostat) tablets prescribing information Reference ID: 2898038, Deerfield, IL
Tsuda H, Kawada N, Kaimori JY, Kitamura H, Moriyama T, Rakugi H, Takahara S, Isaka Y (2012) Febuxostat suppressed renal ischemia-reperfusion injury via reduced oxidative stress. Biochem Biophys Res Commun 427:266–272
Wang B, Gong X, Wan JY, Zhang L, Zhang Z, Li HZ, Min S (2011) Resolvin D1 protects mice from LPS-induced acute lung injury. Pulm Pharmacol Ther 24:434–441
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342:1334–1349
Wright CE, Rees DD, Moncada S (1992) Protective and pathological roles of nitric oxide in endotoxin shock. Cardiovasc Res 26:48–57
Yao HW, Mao LG, Zhu JP (2006) Protective effects of pravastatin in murine lipopolysaccharide-induced acute lung injury. Clin Exp Pharmacol Physiol 33:793–797
Yeh CC, Kao SJ, Lin CC, Wang SD, Liu CJ, Kao ST (2007) The immunomodulation of endotoxin-induced acute lung injury by hesperidin in vivo and in vitro. Life Sci 80:1821–1831
Zhang G, Ghosh S (2000) Molecular mechanisms of NF-kappaB activation induced by bacterial lipopolysaccharide through toll-like receptors. J Endotoxin Res 6:453–457
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fahmi, A.N.A., Shehatou, G.S.G., Shebl, A.M. et al. Febuxostat protects rats against lipopolysaccharide-induced lung inflammation in a dose-dependent manner. Naunyn-Schmiedeberg's Arch Pharmacol 389, 269–278 (2016). https://doi.org/10.1007/s00210-015-1202-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-015-1202-6