Abstract
Purpose
The indicator “concurrent use of three or more psychotropic drugs” has been used as a measure of quality in drug use among the elderly. The aim of our study was to assess to what extent the indicator captures the use of specific psychotropics associated with an increased risk of adverse events among the elderly, i.e., potentially inappropriate psychotropic drugs (PIP).
Methods
All individuals aged 75 years and older in Sweden purchasing prescribed psychotropic drugs in 2006 constituted the study population (n = 384,904). Data on purchased psychotropic drugs from the Swedish Prescribed Drug Register were used. The overlap between individuals with the indicator and individuals using PIP was assessed with sensitivity, specificity, positive and negative predictive values and likelihood ratio as outcome measures.
Results
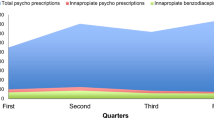
Among the psychotropic drug users, 15% had the indicator and 39% used PIP. The proportion of individuals with the indicator among all individuals using PIP was 27% (sensitivity). The proportion of individuals without the indicator among all individuals not using PIP was 93% (specificity). The positive predictive value was 72%, and the negative predictive value was 67%. Differences in outcome measures were observed between different categories of PIP.
Conclusions
The indicator “concurrent use of three or more psychotropics” can be technically easy to use, but PIP is more specific. Three quarters of all individuals who used PIP in this study were not captured by the indicator. However, two thirds of all individuals with the indicator used PIP. When selecting instruments to assess appropriateness in drug therapy in the elderly, clinical relevance should be balanced against convenience of use.


Similar content being viewed by others
References
Shi S, Morike K, Klotz U (2008) The clinical implications of ageing for rational drug therapy. Eur J Clin Pharmacol 64:183–199
Report of a working group prepared for the Director of Research and Development of the NHS Management Executive (1993) What do we mean by appropriate health care? Qual Health Care 2:117–123
Spinewine A, Schmader KE, Barber N et al (2007) Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet 370:173–184
Beers MH (1997) Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med 157:1531–1536
Fick DM, Cooper JW, Wade WE et al (2003) Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 163:2716–2724
McLeod PJ, Huang AR, Tamblyn RM et al (1997) Defining inappropriate practices in prescribing for elderly people: a national consensus panel. Can Med Assoc J 156:385–391
Naugler CT, Brymer C, Stolee P et al (2000) Development and validation of an improving prescribing in the elderly tool. Can J Clin Pharmacol 7:103–107
Laroche ML, Charmes JP, Merle L (2007) Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol 63:725–731
Brekke M, Rognstad S, Straand J et al (2008) Pharmacologically inappropriate prescriptions for elderly patients in general practice: How common? Baseline data from The Prescription Peer Academic Detailing (Rx-PAD) study. Scand J Prim Health Care 26:80–85
Basger BJ, Chen TF, Moles RJ (2008) Inappropriate medication use and prescribing indicators in elderly Australians: development of a prescribing indicators tool. Drugs Aging 25:777–793
Fialova D, Topinkova E, Gambassi G et al (2005) Potentially inappropriate medication use among elderly home care patients in Europe. JAMA 293:1348–1358
Hoven JL, Haaijer-Ruskamp FM, Vander Stichele RH (2005) Indicators of prescribing quality in drug utilisation research: report of a European meeting (DURQUIM). Eur J Clin Pharmacol 60:831–834
Andersen M (2006) Is it possible to measure prescribing quality using only prescription data? Basic Clin Pharmacol Toxicol 98:314–319
Wettermark B, Tomson G, Bergman U (2006) Quality indicators for drug utilization—new European recommendations (in Swedish). Lakartidningen 103:3469–3472
Campbell SM, Braspenning J, Hutchinson A et al (2003) Research methods used in developing and applying quality indicators in primary care. Br Med J 326:816–819
Robertson HA, MacKinnon NJ (2002) Development of a list of consensus-approved clinical indicators of preventable drug-related morbidity in older adults. Clin Ther 24:1595
National Board of Health and Welfare (2003) Indicators for evaluation of the quality in drug use among the eldery: proposal from the National Board of Health and Welfare (in Swedish). Report number 2003-110-20. National Board of Health and Welfare, Stockholm
Ruths S (2008) Evaluation of prescribing quality in nursing homes based on drug-specific indicators: The Bergen district nursing home (BEDNURS) study. Nor J Epidemiol 18:173–178
Linden M, Bar T, Helmchen H (2004) Prevalence and appropriateness of psychotropic drug use in old age: results from the Berlin Aging Study (BASE). In. Psychogeriatr 16:461–480
Draper B, Brodaty H, Low LF et al (2001) Use of psychotropics in Sydney nursing homes: associations with depression, psychosis, and behavioral disturbances. Int Psychogeriatr 13:107–120
Giron MS, Forsell Y, Bernsten C et al (2001) Psychotropic drug use in elderly people with and without dementia. Int J Geriatr Psychiatry 16:900–906
Klarin I, Wimo A, Fastbom J (2005) The association of inappropriate drug use with hospitalisation and mortality - a population-based study of the very old. Drugs Aging 22:69–82
Johnell K, Fastbom J, Rosen M et al (2007) Inappropriate drug use in the elderly: a nationwide register-based study. Ann Pharmacother 41:1243–1248
Association of Local Authorities and Regions and The National Board of Health and Welfare (2008) Quality and efficiency in Swedish health care—regional comparisons 2007. Stockholm, Sweden.
National Association of State Mental Health Report Program Directors (2001) Technical report on psychiatric polypharmacy. Medical Directors Council and State Medicaid Directors, Alexandria
World Health Organization (WHO) Collaborating Centre for Drug Statistics. Methodology ATC index with DDDs. WHOCC, Oslo. Available at: www.whocc.no
Wettermark B, Hammar N, Fored CM et al (2007) The new Swedish Prescribed Drug Register—opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16:726–735
Statistics Sweden (2008) The statistical database (Statistikdatabasen). Available at: http://www.ssd.scb.se/. Accessed 17 June 2008
Johnell K, Fastbom J (2008) Multi-dose drug dispensing and inappropriate drug use: a nationwide register-based study of over 700,000 elderly. Scand. J Prim Health Care 26:86–91
Jano E, Aparasu RR (2007) Healthcare outcomes associated with Beers’ criteria: a systematic review. Ann Pharmacother 41:438–447
Chutka DS, Takahashi PY, Hoel RW (2004) Inappropriate medications for elderly patients. Mayo Clin Proc 79:122–139
Wilson K, Mottram P (2004) A comparison of side effects of selective serotonin reuptake inhibitors and tricyclic antidepressants in older depressed patients: a meta-analysis. Int J Geriatr Psychiatry 19:754–762
Acknowledgements
This study is part of a larger project on quality indicators that has received funding from the county council in Region Västra Götaland. The project was designed by the researchers at the Nordic School of Public Health. The authors would like to thank the responsible persons at Dosapoteket in Gothenburg for providing access to the database.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lesén, E., Petzold, M., Andersson, K. et al. To what extent does the indicator “concurrent use of three or more psychotropic drugs” capture use of potentially inappropriate psychotropics among the elderly?. Eur J Clin Pharmacol 65, 635–642 (2009). https://doi.org/10.1007/s00228-009-0623-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0623-x