Abstract
Purpose
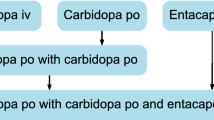
Opicapone (OPC) is a novel catechol-O-methyltransferase (COMT) inhibitor to be used as adjunctive therapy in levodopa-treated patients with Parkinson’s disease. The purpose of this study was to evaluate the effect of moderate liver impairment on the pharmacokinetics (PK) and pharmacodynamics (PD; effect on COMT activity) of OPC.
Methods
An open-label, parallel-group study in patients (n = 8) with moderate liver impairment (Child–Pugh category B, score of 7 to 9) and matched healthy subjects (n = 8, control) with normal liver function. All subjects received a single 50-mg oral dose of OPC, with plasma and urine concentrations of opicapone and its metabolites measured up to 72 h post-dose, including soluble COMT (S-COMT) activity. A one-way analysis of variance (ANOVA) was used to compare the main PK and PD parameters between groups. Point estimates (PE) of geometric mean ratios (GMR) and corresponding 90 % confidence intervals (90%CI) for the ratio hepatic/control subjects of each parameter were calculated and compared with the reference interval (80–125 %).
Results
Exposure to opicapone (AUC and Cmax) increased significantly in patients with moderate hepatic impairment (PE [90%CI]: AUC0-∞, 184 % [135–250 %]; Cmax, 189 % [144–249 %]). Although apparent total clearance (CL/F) of opicapone was decreased by ∼35 %, similar elimination half-life and unbound/bound fractions of opicapone were observed between the two groups. Both rate and extent of exposure to BIA 9-1103 were higher in the hepatically impaired group, but not statistically significant compared with the control group. Similar to the parent (opicapone), the observed increase in exposure to BIA 9-1106 was statistically significant in the hepatically impaired group over the control group. BIA 9-1106 was the only metabolite detected in urine and its urine PK parameters were in accordance with plasma data. Maximum S-COMT inhibition (Emax) occurred earlier for the hepatically impaired group with values of 100 % and 91.2 % for the hepatically impaired and control groups respectively. Both Emax and AUEC for the hepatically impaired group reached statistical significance over the control group. OPC was well tolerated in both hepatically impaired and control groups.
Conclusion
The bioavailability of an orally administered single dose of 50 mg OPC was significantly higher in patients with moderate chronic hepatic impairment, perhaps by a reduced first-pass effect. As the tolerability profile of OPC was favourable under the conditions of this study and its exposure is completely purged from systemic circulation before the subsequent dose administration, no OPC dose adjustment is needed in patients with mild to moderate chronic hepatic impairment. However, as OPC is under clinical development for use as adjunctive therapy in levodopa-treated patients with Parkinson’s disease, an adjustment of levodopa and/or OPC regimens in patients should be carefully considered based on a potentially enhanced levodopa dopaminergic response and the associated tolerability.


Similar content being viewed by others
References
Palma PN, Laszlo K, Soares-da-Silva P (2013) Catechol-O-methyltransferase inhibitors: present problems and relevance of the new ones. In: Martinez A, Gil C (eds) Emerging drugs and targets for Parkinson’s disease. The Royal Society of Chemistry, Cambridge, pp 83–109
Kiss LE, Ferreira HS, Torrao L, Bonifacio MJ, Palma PN, Soares-da-Silva P, Learmonth DA (2010) Discovery of a long-acting, peripherally selective inhibitor of catechol-O-methyltransferase. J Med Chem 53(8):3396–3411
Palma PN, Bonifácio MJ, Loureiro AI, Soares-da-Silva P (2012) Computation of the binding affinities of catechol-O-methyltransferase inhibitors: multisubstate relative free energy calculations. J Comput Chem 33(9):970–986
Bonifácio MJ, Sutcliffe JS, Torrão L, Wright LC, Soares-da-Silva P (2012) Brain and peripheral levodopa pharmacokinetics in the Cynomolgus monkey following administration of opicapone, a novel catechol-O-methyltransferase inhibitor. Parkinsonism Relat Disord 18(2):S125, abstract
Bonifácio MJ, Torrão L, Loureiro AI, Wright LC, Soares-da-Silva P (2012) Opicapone: characterization of a novel peripheral long-acting catechol-O-methyltransferase inhibitor. Parkinsonism Relat Disord 18(2):S125, abstract
Almeida L, Rocha JF, Falcao A, Palma PN, Loureiro AI, Pinto R, Bonifacio MJ, Wright LC, Nunes T, Soares-da-Silva P (2013) Pharmacokinetics, pharmacodynamics and tolerability of opicapone, a novel catechol-O-methyltransferase inhibitor, in healthy subjects: prediction of slow enzyme-inhibitor complex dissociation of a short-living and very long-acting inhibitor. Clin Pharmacokinet 52(2):139–151
Rocha JF, Almeida L, Falcao A, Palma PN, Loureiro AI, Pinto R, Bonifacio MJ, Wright LC, Nunes T, Soares-da-Silva P (2013) Opicapone: a short lived and very long acting novel catechol-O-methyltransferase inhibitor following multiple-dose administration in healthy subjects. Br J Clin Pharmacol 76(5):763–775
Ferreira JJ, Rocha JF, Falcão A, Pinto R, Nunes T, Soares-da-Silva P (2013) Effect of opicapone multiple-dose regimens on levodopa pharmacokinetics, motor response, and erythrocyte-COMT activity in Parkinson’s patients co-administered with levodopa/dopa-decarboxylase inhibitor. Mov Disord 28(1):S154, abstract
Ferreira JJ, Rocha JF, Santos A, Nunes T, Soares-da-Silva P (2012) The design of a double-blind, placebo- and active-controlled, multi-national phase-III trial in patients with Parkinson’s disease and end-of-dose motor fluctuations: opicapone superiority vs. placebo and non-inferiority vs. entacapone. Mov Disord 27(1):S118, abstract
Lees A, Costa R, Oliveira C, Lopes N, Nunes T, Soares-da-Silva P (2012) The design of a double-blind, placebo-controlled, multi-national phase-III trial in patients with Parkinson’s disease and end-of-dose motor fluctuations: opicapone superiority vs. placebo. Mov Disord 27(1):S127, abstract
EMEA/CHMP (2005) Guideline on the evaluation of the pharmacokinetics of medicinal products in patients with impaired hepatic function. Committee for Medicinal Products for Human Use, European Medicines Agency, London
FDA/CDER (2003) Guidance for industry: pharmacokinetics in patients with impaired hepatic function—study design, data analysis, and impact on dosing and labeling. US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Silver Spring, MD
FDA/CDER (2000) Guidance for industry: bioavailability and bioequivalence studies for orally administered drug products—general considerations. US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Silver Spring, MD
Vieira-Coelho MA, Soares-da-Silva P (1996) Ontogenic aspects of liver and kidney catechol-O-methyltransferase sensitivity to tolcapone. Br J Pharmacol 117(3):516–520
Vieira-Coelho MA, Soares-da-Silva P (1999) Effects of tolcapone upon soluble and membrane-bound brain and liver catechol-O-methyltransferase. Brain Res 821(1):69–78
Tarantino G, Di Minno M, Capone D (2009) Drug-induced liver injury: is it somehow foreseeable? World J Gastroenterol 15(23):2817–2833
Verbeeck R (2008) Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol 64:1147–1161
Conflict of interest
This study was sponsored by Bial (Portela & Cª, S.A). All authors were involved in the design or conduction of the study, the collection, management or analysis of the data, and the preparation or review of the manuscript. Dr Amílcar Falcão received consultancy honoraria from Bial (Portela & Cª, S.A.). Drs José Francisco Rocha, Ana Santos, Nelson Lopes, Teresa Nunes, Roberto Pinto and Patrício Soares-da-Silva are or were employees of Bial at the time of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rocha, J.F., Santos, A., Falcão, A. et al. Effect of moderate liver impairment on the pharmacokinetics of opicapone. Eur J Clin Pharmacol 70, 279–286 (2014). https://doi.org/10.1007/s00228-013-1602-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-013-1602-9