Abstract
Purpose
Prolongation of the QTc interval may result in Torsade de Pointes, a ventricular arrhythmia. Numerous risk factors for QTc interval prolongation have been described, including the use of certain drugs. In clinical practice, there is much debate about the management of the risks involved. In this study, we quantified the effect of these risk factors on the length of the QTc interval.
Methods
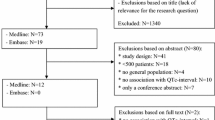
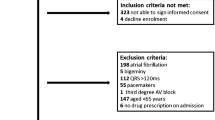
We analyzed all ECGs that were taken during routine practice between January 2013 and October 2016 in the Spaarne Gasthuis, a general teaching hospital in the Netherlands. We collected laboratory values in the week before the ECG recording and the drugs prescribed. For the identification of risk factors, we used multilevel linear regression analysis to correct for multiple ECG recordings per patient.
Results
We included 133,359 ECGs in our study, taken in 40,037 patients. Patients using one QT-prolonging drug had a 11.08 ms (95% CI 10.63–11.52; p < 0.001) longer QTc interval. Patients using two QT-prolonging drugs had a 3.04 ms (95% CI 2.06–4.02; p < 0.001) increase in the QTc interval compared to patients using one QT-prolonging drug. Women had a longer QTc interval compared to men (16.30 ms 95% CI 14.59–18.01; p < 0.001). The QTc interval increased with increasing age, but the difference between men and women diminished. Other independent risk factors that significantly prolonged the QTc interval with at least 10 ms were hypokalemia, hypocalcemia, and the use of loop diuretics.
Conclusion
We identified and quantified various risk factors for QTc interval prolongation.





Similar content being viewed by others
References
Straus SM, Kors JA, De Bruin ML, van der Hooft CS, Hofman A, Heeringa J, Deckers JW, Kingma JH, Sturkenboom MC, Stricker BH, Witteman JC (2006) Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol 47(2):362–367. https://doi.org/10.1016/j.jacc.2005.08.067
Tisdale J, Jaynes H, Kingery J, Mourad N, Trujillo T, Overholser B, Kovacs RJ (2013) Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes 6(4):479–487. https://doi.org/10.1161/CIRCOUTCOMES.113.000152
Mangoni A, Kinirons M, Swift C, Jackson SHD (2003) Impact of age on QT interval and QT dispersion in healthy subjects: a regression analysis. Age Ageing 32(3):326–331. https://doi.org/10.1093/ageing/32.3.326
Benoit S, Mendelsohn A, Nourjah P, Staffa J, Graham D (2005) Risk factors for prolonged QTc among US adults: Third National Health and Nutrition Examination Survey. Eur J Cardiovasc Prev Rehabil 12(4):363–368. https://doi.org/10.1097/01.hjr.0000173110.21851.a9
Sohaib SMA, Papacosta O, Morris R, Macfarlane P, Whincup P (2008) Length of the QT interval: determinants and prognostic implications in a population-based prospective study of older men. J Electrocardiol 41(6):704–710. https://doi.org/10.1016/j.jelectrocard.2008.01.010
Trojak B, Astruc K, Pinoit J, Chauvet Gelinier J, Ponavoy E, Bonin B, Gisselmann A (2009) Hypokalemia is associated with lengthening of QT interval in psychiatric patients on admission. Psychiatry Res 169(3):257–260. https://doi.org/10.1016/j.psychres.2008.06.031
Jardin CGM, Putney D, Michaud S (2014) Assessment of drug-induced torsade de pointes risk for hospitalized high-risk patients receiving QT-prolonging agents. Ann Pharmacother 48(2):196–202. https://doi.org/10.1177/1060028013512614
Niemeijer MN, van den Berg ME, Eijgelsheim M, Rijnbeek PR, Stricker BH (2015) Pharmacogenetics of drug-induced QT interval prolongation: an update. Drug Saf 38(10):855–867. https://doi.org/10.1007/s40264-015-0316-6
Roden D (2004) Drug-induced prolongation of the QT interval. N Engl J Med 350(10):1013–1022. https://doi.org/10.1056/NEJMra032426
Yap Y, Camm AJ (2003) Drug induced QT prolongation and torsades de pointes. Heart 89(11):1363–1372. https://doi.org/10.1136/heart.89.11.1363
Straus SM, Sturkenboom MC, Bleumink GS, Dieleman JP, van der Lei J, de Graeff PA, Kingma JH, Stricker BH (2005) Non-cardiac QTc-prolonging drugs and the risk of sudden cardiac death. Eur Heart J 26(19):2007–2012. https://doi.org/10.1093/eurheartj/ehi312
De Bruin ML, Langendijk PN, Koopmans RP, Wilde AA, Leufkens HG, Hoes AW (2007) In-hospital cardiac arrest is associated with use of non-antiarrhythmic QTc-prolonging drugs. Br J Clin Pharmacol 63(2):216–223. https://doi.org/10.1111/j.1365-2125.2006.02722.x
Woosley, RL and Romero, KA (2015) QT drug list. http://wwwCrediblemedsorg Accessed Oct 2015
Bazett HC (1920) An analysis of the time-relations of the electrocardiograms. Heart 7:353–370
EMEA (1997) The assessment of the potential for QT interval prolongation by non-cardiovascular medicinal products. http://www.fda.gov/ohrms/dockets/ac/03/briefing/pubs/cpmp.pdf, http://www.fda.gov/ohrms/dockets/ac/03/briefing/pubs/cpmp.pdf
Fridericia LS (1920) Die systolendauer im elektrokardiogramm bei normalen menschen und bei herzkranken. Acta Med Scand 53:469–486
Vandenberk B, Vandael E, Robyns T, Vandenberghe J, Garweg C, Foulon V, Ector J, Willems R (2016) Which QT correction formulae to use for QT monitoring? J Am Heart Assoc 5. https://doi.org/10.1161/JAHA.116.003264
Zeltser D, Justo D, Halkin A, Prokhorov V, Heller K, Viskin S (2003) Torsade de pointes due to noncardiac drugs: most patients have easily identifiable risk factors. Medicine (Baltimore) 82(4):282–290. https://doi.org/10.1097/01.md.0000085057.63483.9b
Meid AD, von Medem A, Heider D, Adler JB, Günster C, Seidling HM, Quinzler R, König HH, Haefeli WE (2017) Investigating the additive interaction of QT-prolonging drugs in older people using claims data. Drug Saf 40(2):133–144. https://doi.org/10.1007/s40264-016-0477-y
Nachimuthu S, Assar MD, Schussler JM (2012) Drug-induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf 3(5):241–253. https://doi.org/10.1177/2042098612454283
Pham TV, Rosen MR (2002) Sex, hormones, and repolarization. Cardiovasc Res 53(3):740–751. https://doi.org/10.1016/S0008-6363(01)00429-1
Kurokawa J, Kodama M, Clancy CE, Furukawa T (2016) Sex hormonal regulation of cardiac ion channels in drug-induced QT syndromes. Pharmacol Ther . https://doi.org/10.1016/j.pharmthera.2016.09.004
Rautaharju PM, Zhou SH, Wong S, Calhoun HP, Berenson GS, Prineas R, Davignon A (1992) Sex differences in the evolution of the electrocardiographic QT interval with age. Can J Cardiol 8(7):690–695
Tisdale JE (2016) Drug-induced QT interval prolongation and torsades de pointes: role of the pharmacist in risk assessment, prevention and management. Can Pharm J (Ott) 149(3):139–152. https://doi.org/10.1177/1715163516641136
Estes NA 3rd (2013) Computerized interpretation of ECGs: supplement not a substitute. Circ Arrhythm Electrophysiol 6(1):2–4. https://doi.org/10.1161/CIRCEP.111.000097
Postema PG, De Jong JS, Van der Bilt IA, Wilde AA (2008) Accurate electrocardiographic assessment of the QT interval: teach the tangent. Heart Rhythm 5(7):1015–1018. https://doi.org/10.1016/j.hrthm.2008.03.037
Poon K, Okin PM, Kligfield P (2005) Diagnostic performance of a computer-based ECG rhythm algorithm. J Electrocardiol 38(3):235–238. https://doi.org/10.1016/j.jelectrocard.2005.01.008
Acknowledgements
We would like to thank Pieter G. Postema for his useful comments in preparing this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Electronic supplementary material
ESM 1
(DOCX 78 kb)
Rights and permissions
About this article
Cite this article
Heemskerk, C.P.M., Pereboom, M., van Stralen, K. et al. Risk factors for QTc interval prolongation. Eur J Clin Pharmacol 74, 183–191 (2018). https://doi.org/10.1007/s00228-017-2381-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2381-5