Abstract
Purpose
Inhaled drug delivery is an attractive route by which to deliver drugs to lungs of patients with idiopathic pulmonary fibrosis (IPF). GSK3008348 is a potent and selective small molecule being developed as the first inhaled inhibitor of the αvβ6 integrin for the treatment of IPF. The phase 1 first-time-in-human clinical trial (NCT02612051) presented here was designed to investigate the safety, tolerability and pharmacokinetic (PK) profile of single doses of GSK3008348 in healthy participants.
Methods
Single ascending doses of GSK3008348 were administered to three cohorts of eight healthy participants in a randomised, double-blind, placebo-controlled, 4-period crossover design. Safety, tolerability and PK were assessed after single doses of 1–3000 mcg given by nebulisation.
Results
A total of 29 participants were enrolled and received at least one dose of study treatment. There were no serious adverse events (AE) reported in any participant. No trends or clinically important differences were noted in the incidence or intensity of AEs or other safety assessments. Maximum plasma concentrations of GSK3008348 were generally attained within approximately 30 min after start of nebulisation, with geometric mean terminal elimination half-lives ranging from 7.95 to 10.2 h. Exposures, as measured by area under the plasma concentration-time curve (AUC), were dose proportional across all doses where estimates were possible (100–3000 mcg). Dose normalised geometric mean Cmax increased with dose up to 3000 mcg. This supra proportionality was relatively modest, with a less than 3-fold increase over the range from 30 to 3000 mcg. The reason(s) for this observation are currently not known but may be due to slower absorption at the lowest doses. All exposures were within the exposure margins set by the non-clinical toxicity studies and so this is not expected to have any impact on safety.
Conclusions
In summary, GSK3008348 was well tolerated at single doses up to 3000 mcg in healthy participants, and its PK profile was dose proportional at potentially clinically relevant doses (300–3000 mcg). These findings support further development of GSK3008348 as a novel inhaled treatment option for IPF.
Similar content being viewed by others
Introduction
Idiopathic pulmonary fibrosis (IPF) is a form of chronic, progressive fibrosing interstitial pneumonia with unknown aetiology, associated with a histological appearance of usual interstitial pneumonia. IPF progresses in a relentless and often insidious manner and is lethal, with median survival ranging from 2 to 4 years and a 5-year survival range of 20–30% [1, 2]. There are two disease-modifying treatments currently available to patients: pirfenidone and nintedanib. Both are oral anti-fibrotic therapies that demonstrate a reduction in the rate of decline in lung function (forced vital capacity, FVC) over 1 year [3, 4]. Pirfenidone is associated with phototoxicity, and both pirfenidone and nintedanib cause significant gastrointestinal effects, resulting in discontinuation due to adverse events (AEs) in approximately 30% of patients treated with pirfenidone and 20% of patients treated with nintedanib [5].
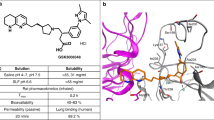
Development of new treatments for IPF has focussed on targets that drive fibrogenesis. It is likely that for maximal efficacy, a new medicine must reach the distal areas of the lung where fibrosis occurs. Aerosol-driven direct lung exposure combined with systemic drug availability may maximise the potential of a drug to reach all areas of the lung over a sustained period at lower doses than other routes of administration. GSK3008348 is a small molecule inhibitor of alpha-v beta-6 (αvβ6) integrin and represents the first inhaled compound in this class. The αvβ6 integrin plays a key role in the activation of transforming growth factor-β (TGFβ) [6] that is hypothesised to be central in the development of IPF [7, 8]. Expression of αvβ6 is significantly upregulated in IPF lung tissue [9] and localised to damaged epithelial sites [10]. Levels are also prognostic, with increased levels of αvβ6 observed in patients with rapidly progressing IPF [11]. Therefore, the αvβ6 integrin is an attractive therapeutic target for IPF with the advantage of inhibiting disease-specific activation of TGFβ via αvβ6, while limiting the potential for toxicological effects that may be associated with direct inhibition of TGFβ, that includes heart valve lesions and physeal dysplasia [12].
GSK3008348 demonstrates selectivity for αvβ6 and binds to the integrin with high affinity [13]. It has been shown to inhibit the activation of TGFβ with a prolonged duration of action in non-clinical in vitro and in vivo studies [14]. On delivery by nebulisation directly to the lungs, GSK3008348 is anticipated to bind to αvβ6 on the damaged epithelium and reduce TGFβ activation, thereby limiting the ability of TGFβ to promote collagen production and halting or slowing the progression of fibrosis. The study presented here was designed to investigate the safety, tolerability and pharmacokinetic (PK) profile of single doses of GSK3008348 in healthy participants.
Methods
Study design
This was a first-time-in-human, randomised, double-blind, single ascending-dose study of nebulised GSK3008348 (NCT02612051). GSK3008348 was formulated as a solution, administered via nebulisation over approximately 10 min using a Philips Respironics Inno Spire Delux Nebuliser with a Philips side stream mouthpiece. Informed consent was obtained from all individual participants in the study.
Two cohorts of eight healthy participants each were randomised 3:1 to receive GSK3008348 (n = 6) or placebo (n = 2) in each period of a 4-period crossover. Within each cohort, participants were randomised to receive up to three ascending doses of GSK3008348 and one of placebo. In case it was necessary to repeat any doses to obtain more PK or safety data, a third cohort with the same design was also included in the study. Sentinel dosing was used throughout: on day 1, two subjects were dosed one active and one placebo, the remaining subjects in the dosing group were dosed the following day. Once each dose group had been completed, there was a blinded review of the safety and PK before proceeding to the next dose (Fig. 1).
In each period, participants were admitted to the clinical unit before dosing and were discharged 48 h after their dose. There was a washout period of at least 6 days between doses. This was based on non-clinical PK observations predicting an effective half-life of less than 12 h and human in vitro studies indicating a modestly extended pharmacodynamic effect. GSK3008348 demonstrates a receptor dissociation half-life of ~ 9 h and induces rapid internalisation of αvβ6 (minutes) followed by a slow return of the integrin to the cell surface (hours) due to integrin degradation [13, 14]. Non-clinical PK studies demonstrated rapid absorption of the drug from the lung into the systemic circulation with no evidence of significant lung retention. After the final dose, there was a follow-up period for 7–14 days.
Cohort 1 received 1, 3, 10, and 30 mcg GSK3008348, and cohort 2 received 100, 300, 1000, and 3000 mcg GSK3008348. Cohort 3 received a repeat of the highest dose levels, 1000 and 3000 mcg GSK3008348, to obtain additional information on safety and PK. The 1 mcg starting dose of GSK3008348 was predicted to engage approximately 15% of the αvβ6 in healthy lungs at lung peak concentrations, and the free systemic concentrations were predicted to be below the KD at maximum plasma concentration (Cmax). This was a deliberately conservative approach given the novel mechanism. Dose escalation was continued, using half log steps, to a maximum of 3000 mcg in order to explore sustained higher occupancies (predicted > 90%) where downstream biomarker modulation and efficacy may be expected based on pre-clinical evidence [14]. In addition, 3000 mcg was the maximum dose supported by non-clinical toxicological studies. No systemic toxicity was identified at all doses tested in the 4-week inhalation toxicity studies. The human systemic exposures achieved across the dose range were within the systemic nonclinical safety margins.
The objectives of the study were achieved after the first two dosing periods in cohort 3; therefore, the study was terminated and the final two dosing periods in cohort 3 were not required.
Study participants
Healthy male or female participants aged ≥ 18 years, with body weight ≥ 50 kg and body mass index ≥ 19.0–≤ 35.0 kg/m2, were eligible to participate in the study. Female participants were eligible if they were of non-childbearing potential. Participants were determined as healthy based on medical history, physical examination, clinical laboratory tests (haematology, clinical chemistry, urinalysis, HIV and hepatitis B and C screen, and drug, alcohol and smoking screening tests), 12-lead electrocardiogram (ECG), continuous cardiac telemetry, vital signs and pulmonary function tests.
Current smokers and participants with current or history of liver disease, known hepatic or biliary abnormalities, current or history of photosensitivity, current respiratory tract infection or history of excessive alcohol consumption were excluded.
Safety assessments
Participants were under continuous medical supervision during each admission period (up to 48 h post-dose), and safety assessments were made at regular intervals throughout each period and until the end of follow-up. Assessment of safety was conducted by monitoring AEs, clinical laboratory tests (haematology, clinical chemistry and urinalysis), vital signs (including pulse oximetry), 12-lead ECGs, telemetry, physical examinations and pulmonary function tests (forced expiratory volume in 1 s [FEV1], FVC, diffusing capacity of the lung for carbon monoxide).
PK assessments
Blood samples for the measurement of plasma GSK3008348 concentrations were taken up to 24 h after each dose administration and up to 30 h after dose administration in cohort 3. Analysis was conducted using a validated analytical method based on protein precipitation, followed by high-performance liquid chromatography (Waters Acquity Chromatograpy System) and mass spectrometry detection via an electrospray interface with multiple reaction monitoring (Waters Xevo TQ-S). The lower limit of quantification for GSK3008348 was 50 pg/mL using a 50-μL aliquot of human plasma with a higher limit of quantification of 50,000 pg/mL. The overall assay accuracy (% deviation from nominal) was ± 3.5% and precision (% coefficient of variation) was ≤ 8.4%.
Statistical methods
Safety data was summarised descriptively and presented in tabular format. PK parameters were determined by non-compartmental analysis of GSK3008348 plasma concentration-time data. The following parameters were generated where data permitted: Cmax, time of maximum concentration (Tmax), terminal half-life (T½), area under the plasma concentration-time curve from zero hours to time (AUC0-t) and area under the plasma concentration-time curve from 0 h to infinity (AUC0-inf).
An assessment of dose proportionality was made for Cmax and AUC0-inf using the power model [15]. Both parameters were loge-transformed, and a mixed-effect model was fitted for each parameter with loge (dose) as a fixed effect and subject specific intercepts as a random effect. For each parameter, the exponent of the power model and corresponding 90% confidence intervals (CIs) were estimated. Further dose proportionality analyses were performed using the analysis of variance method. Dose-normalised, loge-transformed AUC0-inf and Cmax were analysed separately using a mixed-effect model as described above but with dose as a categorical variable. Pairwise comparisons were made with respect to each dose versus the chosen reference dose of 300 mcg.
Results
Participant demographics and disposition
A total of 64 participants were screened, and 29 participants were enrolled and received at least one dose of GSK3008348 or placebo. Six participants were withdrawn: two due to AEs, three due to abnormal clinical laboratory safety tests and one due to a positive drug/alcohol screen on readmission. None of the AEs or abnormal clinical laboratory safety tests that led to withdrawal were attributed to GSK3008348. The demographics of the participants are summarised in Table 1.
Safety results
GSK3008348 was well tolerated at all dose levels, and there were no noted trends or clinically important differences in the incidence of AEs with escalating doses of GSK3008348 that would be suggestive of toxicity in humans. In fact, no treatment-related AEs were reported at the highest doses of 1000 or 3000 mcg GSK3008348. No serious AEs were reported in the study, and no participant was withdrawn due to a treatment-related AE.
Overall, 11 out of 29 participants experienced at least one AE in the study, all of which were considered mild in intensity. The two AEs that led to withdrawal of participants were a common cold, reported after a 3-mcg dose, and papular rash over the body, reported after a 100-mcg dose. Neither AE were considered to be related to study treatment. All AEs were resolved by follow-up, with the exception of the papular rash, which was ongoing at follow-up but was considered mild and unrelated to study treatment.
Five participants reported AEs that were considered related to study treatment, as summarised in Table 2; note that relatedness was assessed before unblinding of study treatment; therefore, some AEs were considered related to treatment with placebo. The most common treatment-related AEs were cough and dizziness, reported in two participants each.
There were no clinically significant abnormal clinical laboratory values. All 12-lead ECG, telemetry and vital sign measurements outside normal ranges were deemed not clinically significant. Analysis of individual change from baseline in FEV1 and FVC over time did not show clinically significant differences between the treatment groups (Supplementary Table 1). No notable trends were observed in clinical laboratory parameters, ECGs, vital signs and pulmonary function test values during the course of the study or between treatment groups.
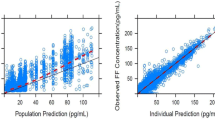
PK results
Median plasma concentrations at each nominal time point for each treatment are summarised in Fig. 2. At the lowest dose levels of 1, 3 and 10 mcg GSK3008348, plasma concentrations were not quantifiable. Plasma concentrations of GSK3008348 were measurable between 0.25 and 4 h post-dose in all but one participant following 30-mcg doses, and up to 24 h post-dose following doses of 100 mcg and higher. Plasma concentrations were also measurable up to 30 h post-dose following 1000- and 3000-mcg doses. The plasma concentration-time profiles showed rapid absorption of GSK3008348 up to 1–3 h post-dose, followed by rapid decline 4–12 h post-dose, followed by a slower decline with geometric mean T½ ranging from 7.95 to 10.2 h, suggesting multi-phasic elimination of GSK3008348. A summary of derived GSK3008348 PK parameters following single nebulised doses of 1–3000 mcg GSK3008348 are presented in Table 3 and selected dose normalised parameters in Table 4. Lower variability in the GSK3008348 plasma concentration profiles was observed between participants at doses of 300, 1000 and 3000 mcg compared with the lower doses (Table 3).
Systemic exposure of GSK3008348, as measured by geometric mean AUC0-inf, AUC0-t and Cmax, increased with escalating dose. There appeared to be no trend in the dose normalised geometric mean AUC0-inf estimates, with the lowest dose normalised geometric mean observed at 300 mcg (26.8 pg*h/mL) and the highest adjusted geometric mean observed at 100 mcg (35.3 pg*h/mL). In contrast, dose normalised geometric means for Cmax increased with escalating doses of GSK3008348, although they appeared to plateau above 1000 mcg (Table 4). This effect may have been due to moderately slower absorption from the lung at lower doses, as the Tmax was latest at the 30-mcg dose and a later upper range was observed at doses lower than 3000 mcg (Table 3).
Inter-individual variability in the extent of systemic exposure to GSK3008348 ranged from low to high, with geometric coefficient of variance (CV) for Cmax, AUC0-t and AUC0-inf ranging from 16.6 to 106%, 20.1 to 99.0% and 19.8 to 52.5%, respectively, across all dose groups where quantifiable plasma concentrations were observed.
Dose proportionality assessment
Dose normalised AUC(0-inf) and Cmax are summarised in Table 4 and show that AUC(0-inf) generally increased in a dose proportional manner. Consistent with that observation, a preliminary assessment of dose proportionality between subjects was made using the power model with the exponent of the power model fitted to AUC(0-inf) estimated at 0.98 (90% CI: 0.90, 1.05) (Supplementary Table 2).
There was a clear trend for the dose normalised geometric mean Cmax to increase with dose up to 3000 mcg. The increase was relatively modest, with a less than 3-fold increase over the range from 30 to 3000 mcg. The exponent of the power model fitted to Cmax was estimated at 1.21 (90% CI: 1.13, 1.29) (Supplementary Table 2). At the 1000- and 3000-mcg doses, dose normalised geometric means remained constant, suggesting that dose proportionality for Cmax was achieved at higher doses (Supplementary Table 3; Supplementary Fig. 1).
Discussion
Treatment of IPF remains a significant unmet need, despite the recent availability of two licenced medicines: pirfenidone and nintedanib. Current treatments reduce the rate of decline in lung function, but do not stop progression of IPF altogether. Blockade of αvβ6 integrin represents an attractive anti-fibrotic drug mechanism, with a body of evidence to suggest that it plays a central role in the activation of TGFβ and the pathogenesis of lung fibrosis [16]. By virtue of its restricted expression, αvβ6 represents a more targeted approach to modulating the process of fibrogenesis that results in the laying down of fibrotic tissue in the lung. This has the potential to confer advantages compared with approaches that seek to achieve a more generalised blockade of TGFβ, which has been shown to have negative side effects given TGFβ’s role in a variety of normal physiological processes [17]. Furthermore, in vitro experiments suggest that pirfenidone and nintedanib have limited effects on αvβ6 integrin-mediated TGFβ activation, indicating that targeting this pathway has the potential to provide mechanistic differentiation [18]. These observations also suggest that this approach could be attractive as an add-on therapy to either pirfenidone or nintedanib, as part of a multi-faceted approach to arrest fibrosis, the importance of which has been extensively discussed [19].
GSK3008348 is the first compound in the αvβ6 integrin class to be administered via the inhaled route. In addition to αvβ6 integrin being an attractive mechanism to target localised TGFβ activation in areas of fibrotic lung, delivery of GSK3008348 via inhalation may confer additional advantages compared with oral and intravenous routes of administration. Aerosol-driven direct lung exposure combined with systemic drug availability may maximise the potential of a drug to reach all areas of the lung over a sustained period at lower doses than other routes of administration.
The results from this first-time-in-human, single ascending-dose study provide support for the continued development of GSK3008348 as an inhaled therapy for the treatment of IPF. Safety data collected in the study suggest that GSK3008348 was well tolerated in healthy participants at doses up to 3000 mcg. Importantly, inhalation of GSK3008348 was not associated with local or systemic adverse effects, demonstrating that the inhaled route is a viable one that can be used in future patient studies.
The PK profile for single doses of GSK3008348 was successfully characterised, indicating maximal concentrations at approximately 30 min post-start of nebulisation and geometric mean terminal T½ ranging from 7.95 to 10.2 h. Increases in systemic exposure, defined by the area under the concentration curve, were dose proportional. There was a clear trend for the dose normalised geometric mean Cmax to increase with doses up to 3000 mcg. The increase was relatively modest, with a less than 3-fold increase over the range from 30 to 3000 mcg and may have been due to a slower absorption from the lung at the lowest doses. The implication of the observed PK profile suggests that a twice daily dosing regimen may be efficacious (assuming that lung exposures parallel those in the systemic circulation). An investigational study to determine levels of target engagement in the lung is ongoing and will be utilised to further refine potential dosing regimens (NCT03069989).
It is expected, based on recent comparative observations of the PK of nebulised salbutamol in healthy participants and patients with IPF (unpublished data), that nebulised GSK3008348 would have a similar PK profile in patients with IPF to that observed in the healthy participants in the current study.
Results from this study therefore support the progression of GSK3008348 to the next stage of clinical development. Establishing the safety profile of repeated doses is a key next step, as is investigating the effects of single doses of GSK3008348 on target engagement in patients with IPF (NCT03069989).
Conclusion
This study has demonstrated that GSK3008348, an αvβ6 integrin inhibitor administered as an inhaled solution, was well tolerated, and systemic exposure was linear at doses of 300–3000 mcg. Taken together with results from preclinical studies, these findings support further development of inhaled GSK3008348 for the treatment of IPF.
References
American Thoracic Society (2000) Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med 161(2 Pt 1):646–664
Ley B, Collard HR, King TE Jr (2011) Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 183(4):431–440
King T, Bradford W, Castro-Bernardini S, Fagan E, Glaspole I, Glassberg M et al (2014) Effect of design modifications on trial outcomes in idiopathic pulmonary fibrosis (IPF): analysis of data from ASCEND and CAPACITY (CAP). Eur Respir J 44(Suppl 58)
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, Cottin V, Flaherty KR, Hansell DM, Inoue Y, Kim DS, Kolb M, Nicholson AG, Noble PW, Selman M, Taniguchi H, Brun M, le Maulf F, Girard M, Stowasser S, Schlenker-Herceg R, Disse B, Collard HR, INPULSIS Trial Investigators (2014) Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 370(22):2071–2082
Hughes G, Toellner H, Morris H, Leonard C, Chaudhuri N (2016) Real world experiences: Pirfenidone and Nintedanib are effective and well tolerated treatments for idiopathic pulmonary fibrosis. Journal of clinical medicine 5(9):78
Munger JS, Huang X, Kawakatsu H, Griffiths MJ, Dalton SL, Wu J et al (1999) The integrin alpha v beta 6 binds and activates latent TGF beta 1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 96(3):319–328
Khalil N, O'Connor RN, Flanders KC, Unruh H (1996) TGF-beta 1, but not TGF-beta 2 or TGF-beta 3, is differentially present in epithelial cells of advanced pulmonary fibrosis: an immunohistochemical study. Am J Respir Cell Mol Biol 14(2):131–138
Koli K, Myllarniemi M, Keski-Oja J, Kinnula VL (2008) Transforming growth factor-beta activation in the lung: focus on fibrosis and reactive oxygen species. Antioxid Redox Signal 10(2):333–342
Slack RJ, Fisher AJ, Denyer JC, Flint DJ, Pyne S. (2015) Quantification of αvβ6 integrin expression in normal and fibrotic human lung tissue proceedings of the British pharmacological society. 13(1):P022
Horan GS, Wood S, Ona V, Li DJ, Lukashev ME, Weinreb PH, Simon KJ, Hahm K, Allaire NE, Rinaldi NJ, Goyal J, Feghali-Bostwick CA, Matteson EL, O'Hara C, Lafyatis R, Davis GS, Huang X, Sheppard D, Violette SM (2008) Partial inhibition of integrin alpha(v)beta6 prevents pulmonary fibrosis without exacerbating inflammation. Am J Respir Crit Care Med 177(1):56–65
Saini G, Porte J, Weinreb PH, Violette SM, Wallace WA, McKeever TM et al (2015) alphavbeta6 integrin may be a potential prognostic biomarker in interstitial lung disease. Eur Respir J 46(2):486–494
Anderton MJ, Mellor HR, Bell A, Sadler C, Pass M, Powell S, Steele SJ, Roberts RRA, Heier A (2011) Induction of heart valve lesions by small-molecule ALK5 inhibitors. Toxicol Pathol 39(6):916–924
Hall ER, Bibby LI, Slack RJ (2016) Characterisation of a novel, high affinity and selective alphavbeta6 integrin RGD-mimetic radioligand. Biochem Pharmacol 117:88–96
Slack R, John A, Forty E, Mercer P, Graves R, Pun T, et al. (2016) P112 discovery of a novel, high affinity, small molecule αvβ6 inhibitor for the treatment of idiopathic pulmonary fibrosis. QJM: an international journal of medicine. 109(suppl_1):S60-S60
Gough K, Hutchison M, Keene O, Byrom B, Ellis S, Lacey L et al (1995) Assessment of dose proportionality: report from the statisticians in the pharmaceutical industry/pharmacokinetics UK joint working party. Therapeutic Innovation & Regulatory Science 29:1039–1048
Tatler AL, Jenkins G (2012) TGF-beta activation and lung fibrosis. Proc Am Thorac Soc 9(3):130–136
Ayyaz A, Attisano L, Wrana JL (2017) Recent advances in understanding contextual TGFbeta signaling. F1000Research 6:749
Porte J, Jenkins G (2014) Assessment of the effect of potential antifibrotic compounds on total and alphaVbeta6 integrin-mediated TGF-beta activation. Pharmacol Res Perspect 2(4):e00030
Rangarajan S, Locy ML, Luckhardt TR, Thannickal VJ (2016) Targeted therapy for idiopathic pulmonary fibrosis: where to now? Drugs 76(3):291–300
Acknowledgements
Editorial support, in the form of data checking and copy-editing the final draft of the manuscript in consultation with the authors, was provided by Katy Tucker, PhD CMPP, of Fishawack Indicia Ltd., UK, and was funded by GSK. Julia Kenny provided the non-clinical toxicology supporting information and contributed to the design and revision of the work.
Funding
This study is sponsored by GlaxoSmithKline (GSK; study numbers 200262/NCT02612051). GSK reviewed the manuscript for factual accuracy.
Author information
Authors and Affiliations
Contributions
David Fairman and Maria J Costa made substantial contributions to the conception and design of the work and the analysis and interpretation of the data as well as drafting and revising the work. Charlotte H Maden, Michelle Chalker, William A Fahy, Nadia Garman, Pauline T Lukey, Juliet K Simpson, Robert J Slack, Stuart Kendrick and Richard P Marshall made substantial contributions to the conception and design of the work as well as drafting and revising the work. Tim Mant study PI and Simon Parry made substantial contributions to the acquisition of data as well as drafting and revising the work. All authors have revised the work critically for important intellectual content and have provided final approval of the version to be published. Authors give their agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the South Central-Oxford A Research Ethics Committee, Bristol Research Ethics Committee Centre, Whitefriars, Level 3 Block B, Lewins Mead, Bristol, BS1 2NT. The study took place at Quintiles Drug Research Unit, 6 Newcomen Street, London SE1 1YR.
All animal studies were ethically reviewed and carried out in accordance with the Animals (Scientific Procedures) Act 1986 and the GSK Policy on the Care, Welfare and Treatment of Laboratory Animals.
Competing interests
The authors declare the following interests: Tim Mant is an employee of and holds shares in QuintilesIMS and is also supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. All other authors are employees of, and hold shares/stock options in, GSK.
Electronic supplementary material
ESM 1
(DOCX 171 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Maden, C.H., Fairman, D., Chalker, M. et al. Safety, tolerability and pharmacokinetics of GSK3008348, a novel integrin αvβ6 inhibitor, in healthy participants. Eur J Clin Pharmacol 74, 701–709 (2018). https://doi.org/10.1007/s00228-018-2435-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-2435-3