Abstract
Background
The prognostic value of the International Society of Paediatric Oncology European Neuroblastoma Research Network (SIOPEN) skeletal score using 123iodine-metaiodobenzylguanidine (MIBG) has been confirmed for people with high-risk neuroblastoma. Whole-body MRI with diffusion-weighted imaging is used increasingly.
Objective
To compare the original SIOPEN score and its adaption by diffusion-weighted imaging in high-risk stage 4 neuroblastoma and to evaluate any consequences of score differences on overall survival.
Materials and methods
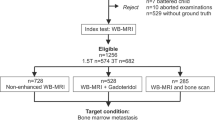
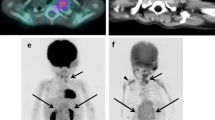
This retrospective observational study included pediatric patients who underwent MIBG scintigraphy and whole-body MRI, including diffusion-weighted imaging, between 2010 and 2015. Semi-quantitative skeletal scores for each exam were calculated independently. A difference of two or more points was defined as clinically relevant and counted as M+ (more in diffusion-weighted imaging) or S+ (more in MIBG). In cases of a negative result in one of the studies, residual disease of 1 point was also rated as relevant. We tested correlation and differences on an exam basis and also grouped by different therapeutic conditions. Overall survival was used to evaluate prognostic relevance.
Results
Seventeen children with 25 paired examinations were evaluated. Median MIBG scintigraphy score was 0 (interquartile range [IQR] 0–4, range 0–25) vs. a median whole-body MRI score of 1 (IQR 0–5.5, range 0–35) (P=0.018). A relevant difference between whole-body MRI and MIBG scintigraphy was noted in 14 of the 25 paired examinations (M+: n=9; S+: n=5). After treatment, the median survival of cases with M+ was 14 months (IQR 4–59, range 1–74 months), while S+ cases showed a median survival of 49 months (IQR 36–52, range 36–52 months) (P=0.413).
Conclusion
The SIOPEN scoring system is feasible for whole-body MRI but might result in slightly higher scores, probably because of MRI’s superior spatial resolution. Further studies are necessary to validate any impact on prognosis.




Similar content being viewed by others
References
Ries LAG, Smith MA, Gurney J et al (1999) Cancer incidence and survival among children and adolescents: United States SEER Program 1975–1995. Surveillance, epidemiology, and end results program. National Cancer Institute, Bethesda
Maris JM (2010) Recent advances in neuroblastoma. N Engl J Med 362:2202–2211
Bar-Sever Z, Biassoni L, Shulkin B et al (2018) Guidelines on nuclear medicine imaging in neuroblastoma. Eur J Nucl Med Mol Imaging 45:2009–2024
Brisse HJ, McCarville MB, Granata C et al (2011) Guidelines for imaging and staging of neuroblastic tumors: consensus report from the International Neuroblastoma Risk Group Project. Radiology 261:243–257
Avanzini S, Pio L, Erminio G, Granata C et al (2017) Image-defined risk factors in unresectable neuroblastoma: SIOPEN study on incidence, chemotherapy-induced variation, and impact on surgical outcomes. Pediatr Blood Cancer 64
Chen AM, Trout AT, Towbin AJ (2018) A review of neuroblastoma image-defined risk factors on magnetic resonance imaging. Pediatr Radiol 48:1337–1347
Irtan S, Brisse HJ, Minard-Colin V et al (2015) Image-defined risk factor assessment of neurogenic tumors after neoadjuvant chemotherapy is useful for predicting intra-operative risk factors and the completeness of resection. Pediatr Blood Cancer 62:1543–1549
Sharp SE, Shulkin BL, Gelfand MJ et al (2009) 123I-MIBG scintigraphy and 18F-FDG PET in neuroblastoma. J Nucl Med 50:1237–1243
Matthay KK, Shulkin B, Ladenstein R et al (2010) Criteria for evaluation of disease extent by (123)I-metaiodobenzylguanidine scans in neuroblastoma: a report for the International Neuroblastoma Risk Group (INRG) task force. Br J Cancer 102:1319–1326
Yanik GA, Parisi MT, Shulkin BL et al (2013) Semiquantitative mIBG scoring as a prognostic indicator in patients with stage 4 neuroblastoma: a report from the Children's Oncology Group. J Nucl Med 54:541–548
Lewington V, Lambert B, Poetschger U et al (2017) (123)I-mIBG scintigraphy in neuroblastoma: development of a SIOPEN semi-quantitative reporting method by an international panel. Eur J Nucl Med Mol Imaging 44:234–241
Pfluger T, Schmied C, Porn U et al (2003) Integrated imaging using MRI and 123I metaiodobenzylguanidine scintigraphy to improve sensitivity and specificity in the diagnosis of pediatric neuroblastoma. AJR Am J Roentgenol 181:1115–1124
Kembhavi SA, Rangarajan V, Shah S et al (2014) Prospective observational study on diagnostic accuracy of whole-body MRI in solid small round cell tumours. Clin Radiol 69:900–908
Piccardo A, Lopci E, Conte M et al (2012) Comparison of 18F-dopa PET/CT and 123I-MIBG scintigraphy in stage 3 and 4 neuroblastoma: a pilot study. Eur J Nucl Med Mol Imaging 39:57–71
Piccardo A, Puntoni M, Lopci E et al (2014) Prognostic value of (1)(8)F-DOPA PET/CT at the time of recurrence in patients affected by neuroblastoma. Eur J Nucl Med Mol Imaging 41:1046–1056
Neubauer H, Li M, Muller VR et al (2017) Diagnostic value of diffusion-weighted MRI for tumor characterization, differentiation and monitoring in pediatric patients with neuroblastic tumors. Rofo 189:640–650
Uhl M, Altehoefer C, Kontny U et al (2002) MRI-diffusion imaging of neuroblastomas: first results and correlation to histology. Eur Radiol 12:2335–2338
Voss SD (2018) Staging and following common pediatric malignancies: MRI versus CT versus functional imaging. Pediatr Radiol 48:1324–1336
Owens C, Li BK, Thomas KE, Irwin MS (2016) Surveillance imaging and radiation exposure in the detection of relapsed neuroblastoma. Pediatr Blood Cancer 63:1786–1793
Applebaum MA, Henderson TO, Lee SM et al (2015) Second malignancies in patients with neuroblastoma: the effects of risk-based therapy. Pediatr Blood Cancer 62:128–133
Lassmann M, Biassoni L, Monsieurs M et al (2007) The new EANM paediatric dosage card. Eur J Nucl Med Mol Imaging 34:796–798
Li C, Zhang J, Chen S et al (2018) Prognostic value of metabolic indices and bone marrow uptake pattern on preoperative 18F-FDG PET/CT in pediatric patients with neuroblastoma. Eur J Nucl Med Mol Imaging 45:306–315
Pai Panandiker AS, Coleman J, Shulkin B (2015) Whole-body pediatric neuroblastoma imaging: 123I-mIBG and beyond. Clin Nucl Med 40:737–739
Goo HW (2010) Whole-body MRI of neuroblastoma. Eur J Radiol 75:306–314
Aslan M, Aslan A, Arioz Habibi H et al (2017) Diffusion-weighted MRI for differentiating Wilms tumor from neuroblastoma. Diagn Interv Radiol 23:403–406
Peschmann AL, Beer M, Ammann B et al (2019) Quantitative DWI predicts event-free survival in children with neuroblastic tumours: preliminary findings from a retrospective cohort study. Eur Radiol Exp 3:6
Meeus EM, Zarinabad N, Manias KA et al (2018) Diffusion-weighted MRI and intravoxel incoherent motion model for diagnosis of pediatric solid abdominal tumors. J Magn Reson Imaging 47:1475–1486
Vik TA, Pfluger T, Kadota R et al (2009) (123)I-mIBG scintigraphy in patients with known or suspected neuroblastoma: results from a prospective multicenter trial. Pediatr Blood Cancer 52:784–790
Callahan MJ, MacDougall RD, Bixby SD et al (2018) Ionizing radiation from computed tomography versus anesthesia for magnetic resonance imaging in infants and children: patient safety considerations. Pediatr Radiol 48:21–30
Schaefer JF, Berthold LD, Hahn G et al (2019) Whole-body MRI in children and adolescents — S1 guideline. Rofo 191:618–625
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gassenmaier, S., Bares, R., Barreuther, M. et al. 123Iodine-metaiodobenzylguanidine scintigraphy versus whole-body magnetic resonance imaging with diffusion-weighted imaging in children with high-risk neuroblastoma — pilot study. Pediatr Radiol 51, 1223–1230 (2021). https://doi.org/10.1007/s00247-020-04960-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04960-2