Abstract
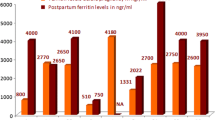
An improvement in quality of life and survival occurred among thalassemia major (TM) patients: pregnancy in such patients has become a reality. Safe pregnancy and delivery require efforts to ensure the best outcomes. Between 2007 and 2016, 30 TM patients had 37 pregnancies. We analyzed the hematological parameters before, during, and after pregnancies and in 19 patients a cardiovascular magnetic resonance (CMR) T2* was performed. The mean age at first pregnancy was 30 ± 4 years; the current mean age is 35 ± 5 years. Twenty-four patients (80%) had a single pregnancy, five patients (17%) had two pregnancies, and one patient (3%) became pregnant three times. Seventeen pregnancies (46%) were spontaneous, 20 (64%) needed gonadotrophin-induced ovulation and/or reproductive technologies. All pregnancies resulted in live births. Seven were twin pregnancies (19%). The mean gestational hemoglobin was 9.2 ± 0.5 g/dl, lower than pre- and postpregnancy (9.8 ± 1 g/dl, p = ns and 9.6 ± 1 g/dl, p = 0.02, respectively). Median ferritin levels increased progressively (1071, range 409–5724 ng/ml, before pregnancy vs 2231, range 836–6918 ng/ml, after pregnancy, p < 0.0001). CMR before pregnancy showed a normal cardiac T2* (mean 35.34 ± 8.90 ms) and a mean liver iron concentration (LIC) of 3.37 ± 2.11 mg/g dry weight (dw). After pregnancy, the mean cardiac T2* was 31.06 ± 13.26 ms and the mean LIC was significantly increased (9.06 ± 5.75 mg/g dw, p = 0.0001). Pregnancy is possible and safe in thalassemia major. During pregnancy, iron accumulates, especially in the liver; a prompt resumption of chelation after delivery is mandatory.


Similar content being viewed by others
References
Borgna-Pignatti C, Cappellini MD, De Stefano P et al (2005) Survival and complications in thalassemia. Ann N Y Acad Sci 1054:40–47
Telfer P, Coen PG, Christou S et al (2006) Survival of medically treated thalassemia patients in Cyprus. Trends and risk factors over the period 1980–2004. Haematologica 91(9):1187–1192
Origa R, Baldan A, Marsella M, Borgna Pignatti C (2015) A complicated disease: what can be done to manage thalassemia major more effectively? Expert Rev Hematol 8:851–862
Thalassemia RD (2016) Modern medicine battles an ancient disease. Am J Hematol 91:15–21
De Sanctis V (2002) Growth and puberty and its management in thalassaemia. Horm Res 58(Suppl 1):72–79
Mousa AA, Ghonem M, Elhadidy EH et al (2016) Iron overload detection using pituitary and hepatic MRI in thalassemic patients having short stature and hypogonadism. Endocr Res 4:1–6
Merchant RH, Shirodkar A, Ahmed J (2011) Evaluation of growth, puberty and endocrine dysfunctions in relation to iron overload in multi transfused Indian thalassemia patients. Indian J Pediatr 78:679–683
Delvecchio M, Cavallo L (2010) Growth and endocrine function in thalassemia major in childhood and adolescence. J Endocrinol Investig 33:61–68
Gulino FA, Vitale SG, Fauzia M, Cianci S, Pafumi C, Palumbo MA (2013) Beta-thalassemia major and pregnancy. Bratisl Lek Listy 114:523–525
Al-Riyami N, Al-Khaduri M, Daar S (2014) Pregnancy outcomes in women with homozygous beta thalassaemia: a single-centre experience from Oman. Sultan Qaboos Univ Med J 14:337–341
Thompson AA, Kim HY, Singer ST et al (2013) Pregnancy outcomes in women with thalassemia in North America and the United Kingdom. Am J Hematol 88:771–773
Carpenter JP, He T, Kirk P et al (2011) On T2* magnetic resonance and cardiac iron. Circulation 123:1519–1528
Wood JC, Enriquez C, Ghugre N et al (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle-cells disease patients. Blood 106:1460–1465
Armitage P, Berry G, Matthews (2002) Statistical methods in medical research, Fourth edn. Blackwell Science, Oxford
Hill CC, Pickinpaugh J (2008) Physiologic changes in pregnancy. Surg Clin North Am 88:391–401
Origa R, Piga A, Quarta G et al (2010) Pregnancy and beta-thalassemia: an Italian multicenter experience. Haematologica 95:376–381
Nassar AH, Naja M, Cesaretti C, Eprassi B, Cappellini MD, Taher A (2008) Pregnancy outcome in patients with beta-thalassemia intermedia at two tertiary care centers, in Beirut and Milan. Haematologica 93:1586–1587
Voskaridou E, Balassopoulou A, Boutou E et al (2014) Pregnancy in beta-thalassemia intermedia: 20-year experience of a Greek thalassemia center. Eur J Haematol 93:492–499
Thalassemia International Federation. Guidelines for the management of transfusion dependent thalassaemia (TDT). 3rd ed
Tuck SM (2005) Fertility and pregnancy in thalassemia major. Ann N Y Acad Sci 1054:300–307
Petrakos G, Andriopoulos P, Tsironi M (2016) Pregnancy in women with thalassemia: challenges and solutions. Int J Womens Health 8(8):441–451
Butwick A, Findley I, Wonke B (2005) Management of pregnancy in a patient with beta thalassaemia major. Int J Obstet Anesth 14:351–354
Messina G, Colombo E, Cassinerio E et al (2010) Pregnant women affected by thalassemia major: a controlled study of traits and personality. J Res Med Sci 15:100–106
Diamantidis MD, Neokleous N, Agapidou A et al (2016) Iron chelation therapy of transfusion-dependent β-thalassemia during pregnancy in the era of novel drugs: is deferasirox toxic? Int J Hematol 103:537–544
Harrison MS, Ali S, Pasha O et al (2015) A prospective population-based study of maternal, fetal, and neonatal outcomes in the setting of prolonged labor, obstructed labor and failure to progress in low- and middle-income countries. Reprod Health 12(Suppl 2):S9
Howard J, Tuck S, Eissa A, Porter J (2012) Hemoglobinpathies in pregnancy. In: Cohen H, O’Brien P (eds) Disorders of thrombosis and hemostasis in pregnancy. Springer, London
Hwang IR, Choi YK, Lee WK et al (2016) Association between prolonged breastfeeding and bone mineral density and osteoporosis in postmenopausal women: KNHANES 2010-2011. Osteoporos Int 27:257–265
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki declaration of 1975, as revised in 2008.
Informed consent was obtained from all patients for being included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cassinerio, E., Baldini, I., Alameddine, R. et al. Pregnancy in patients with thalassemia major: a cohort study and conclusions for an adequate care management approach. Ann Hematol 96, 1015–1021 (2017). https://doi.org/10.1007/s00277-017-2979-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-017-2979-9