Abstract
Objectives
The 9th International Forum for Liver Magnetic Resonance Imaging (MRI) was held in Singapore in September 2019, bringing together radiologists and allied specialists to discuss the latest developments in and formulate consensus statements for liver MRI, including the applications of gadoxetic acid–enhanced imaging.
Methods
As at previous Liver Forums, the meeting was held over 2 days. Presentations by the faculty on days 1 and 2 and breakout group discussions on day 1 were followed by delegate voting on consensus statements presented on day 2. Presentations and discussions centered on two main meeting themes relating to the use of gadoxetic acid–enhanced MRI in primary liver cancer and metastatic liver disease.
Results and conclusions
Gadoxetic acid–enhanced MRI offers the ability to monitor response to systemic therapy and to assist in pre-surgical/pre-interventional planning in liver metastases. In hepatocellular carcinoma, gadoxetic acid–enhanced MRI provides precise staging information for accurate treatment decision-making and follow-up post therapy. Gadoxetic acid–enhanced MRI also has potential, currently investigational, indications for the functional assessment of the liver and the biliary system. Additional voting sessions at the Liver Forum debated the role of multidisciplinary care in the management of patients with liver disease, evidence to support the use of abbreviated imaging protocols, and the importance of standardizing nomenclature in international guidelines in order to increase the sharing of scientific data and improve the communication between centers.
Key Points
• Gadoxetic acid–enhanced MRI is the preferred imaging method for pre-surgical or pre-interventional planning for liver metastases after systemic therapy.
• Gadoxetic acid–enhanced MRI provides accurate staging of HCC before and after treatment with locoregional/biologic therapies.
• Abbreviated protocols for gadoxetic acid–enhanced MRI offer potential time and cost savings, but more evidence is necessary. The use of gadoxetic acid–enhanced MRI for the assessment of liver and biliary function is under active investigation.
Similar content being viewed by others
Introduction
The 9th International Forum for Liver Magnetic Resonance Imaging (MRI) was held in September 2019 in Singapore and attended by 90 invited delegates from Asia (n = 53), Europe (n = 20), North America (n = 8), Central America (n = 4), South America (n = 2), and Australia/New Zealand (n = 3). The majority of delegates were radiologists with expertise in liver MRI, including the use of gadoxetic acid (Primovist, Eovist, Bayer AG); other delegates provided representation from surgery, pathology, and hepatology (see Supplement 1). Discussion and consensus voting at the Forum focused on six topics:
-
Referrer focus: how to build a well-functioning multidisciplinary team in patients with liver tumors
-
Abbreviated MRI protocols for evaluation of liver metastases and hepatocellular carcinoma (HCC)
-
Evaluation of treatment response of liver metastases and clinical impact
-
International diagnostic HCC guidelines and Liver Imaging Reporting and Data System (LI-RADS)
-
Gadoxetic acid–enhanced MRI for treatment decision-making and follow-up of HCC
-
Future possible indications of gadoxetic acid–enhanced MRI.
Consensus statements on these topics were generated at workshops, following peer review of the literature available at the time of the Forum. Delegate voting on each statement could be either “agree,” “disagree,” or “abstain.” A consensus on each statement was considered to be reached if at least 80% of voting delegates agreed.
In this article, we review the relevant literature published prior to and available for discussion at the Forum. Any literature published after the Forum, even if related to the topic, has not been included because it was not available contemporaneously to the delegates.
Referrer focus: how to build a well-functioning multidisciplinary team in patients with liver tumors
The multidisciplinary team approach utilizes regular, scheduled discussions among diverse specialists to review the diagnosis, treatment, and outcomes of individual patients [1]. The adoption of multidisciplinary teams represents best practice in current standards of cancer care [2,3,4]. In relation to liver disease, the American Association for the Study of Liver Diseases (AASLD) states: “Hepatocellular carcinoma patients should be seen in [multidisciplinary] clinics whenever it is feasible and, if not, a referral to a center with a true multidisciplinary clinic should be considered” [5], while the LI-RADS version 2018 states: “Since radiologists may not know all relevant factors, multidisciplinary discussion for consensus-based management may be helpful in difficult cases” [6].
The exact composition of liver multidisciplinary teams and their regularity and methodology for meeting (whether physical or online) vary between institutions, and there is no single definition for what constitutes multidisciplinary care. Typically, specialists attending liver multidisciplinary teams include diagnostic and interventional radiologists, medical oncologists, radiation oncologists, hepatologists, surgeons, pathologists, and support services, reflecting the complex needs and multiple treatment options available to these patients. Radiologists’ roles include interpretation of images for diagnosis, staging, and post-treatment monitoring; performing interventional radiologic procedures; standardizing and updating institutional imaging guidelines; and exchanging experiences with other specialists. The following review of multidisciplinary teams focuses on survival as a measure for improved outcome.
Chang et al [7] and Yopp et al [8] compared two patient cohorts with newly diagnosed HCC before and after the implementation of multidisciplinary care. Median patient survival improved after multidisciplinary care implementation, at 13.2 versus 4.8 months (p = 0.005) in the study by Yopp et al. Another investigational approach, adopted in two retrospective studies, compared survival of cohorts who did versus those who did not receive multidisciplinary care [9, 10]. Both studies reported that multidisciplinary team review was associated with significant improvements in survival (e.g., 5-year survival 71.4% vs. 58.7%; p < 0.001 [10]). Finally, Charriere et al compared patient survival when the multidisciplinary team’s treatment decision was or was not followed [11]. Factors associated with a negative prognosis were (a) not following the multidisciplinary team’s treatment decision (hazard ratio [HR]: 0.39; p < 0.001), together with (b) elevated serum alpha-fetoprotein level (HR: 0.63; p = 0.005), and (c) being outside the Milan criteria for liver transplant eligibility (HR: 0.45; p < 0.001). Hence, despite methodologic limitations associated with retrospective studies, non-identical patient populations, and variable definitions of multidisciplinary care, these studies indicate that the multidisciplinary team approach improves survival in patients with HCC, providing the greatest benefit in patients with advanced tumor stage or more complex risk factors.
Few studies have investigated the influence of multidisciplinary care in metastatic liver disease [12]. However, the role of multidisciplinary teams is supported by multidisciplinary consensus panels that emphasize the importance of specialized, individualized patient care [13].
-
Consensus statement #1
-
To optimize patient care and improve survival, patients with suspected or diagnosed HCC should be evaluated utilizing a multidisciplinary approach (72/75; 96% agreement).
-
Consensus statement #2
-
A multidisciplinary approach is suggested for the management of patients with metastatic disease to the liver (76/79; 96% agreement).
-
Consensus statement #3
-
A radiologist should be a core member of any multidisciplinary team for HCC or metastatic liver disease (70/78; 90% agreement).
Abbreviated MRI protocols for evaluation of liver metastases and HCC
Abbreviated MRI protocols that utilize shorter or fewer imaging sequences have been developed to reduce imaging time, patient discomfort, and potentially costs [14]. Studies of abbreviated MRI protocols cited here are classified into two categories: (a) abbreviated MRI, including hepatobiliary phase (HBP), and (b) non-contrast MRI.
Abbreviated MRI protocols, including HBP
Three retrospective studies simulated the use of abbreviated gadoxetic acid–enhanced MRI protocols for HCC surveillance [15,16,17]. Marks et al reported that an abbreviated MRI protocol comprising T2-weighted (T2W) single-shot, fast spin-echo (SSFSE) and T1-weighted (T1W) HBP imaging 20-min post-gadoxetic acid administration had a negative predictive value (NPV) of 96–97% compared with the composite reference standard [15]. Inclusion of a diffusion-weighted imaging (DWI) sequence did not alter the performance of the abbreviated protocol. Tillman et al also compared T2W SSFSE and T1W HBP imaging 20-min post-gadoxetic acid injection versus a composite reference [16]. Per-lesion sensitivity and NPV of the abbreviated protocol were 85% and 95%, respectively. In the study by Besa et al, T1W HBP imaging 20-min post-gadoxetic acid injection provided per-patient sensitivity and NPV (at 90% and 94%, respectively, pooled data) equivalent to a full protocol (90% and 95%, respectively) [17]. Combining T1W HBP with DWI in the abbreviated protocol reduced sensitivity and NPV (81% and 90%, respectively).
Finally, Canellas et al assessed an abbreviated imaging protocol including ultrafast spin-echo T2W, T1W HBP 20-min post-gadoxetic acid injection, and DWI against a full protocol in patients with pathologically proven colorectal liver metastases (CRLMs) [18]. There were no statistically significant differences in sensitivity or lesion characterization (all > 90%) between the protocols.
Abbreviated protocols in three of the above studies provided cost savings of 31% [15], 31% [17], and 41% [18] versus full protocols by reducing the imaging time. Absolute Medicare reimbursement costs (2017–dated) for the abbreviated and full protocols, respectively, were $365.9 versus $527.8 [17] and $311.33 versus $528.70 [18].
Abbreviated protocols using non-contrast MRI
Two studies compared abbreviated MRI protocols without contrast versus full gadoxetic acid–enhanced MRI for HCC follow-up and for detection of CRLMs. In a retrospective study comparing non-contrast MRI (T1W, T2W, and DWI) versus gadoxetic acid–enhanced MRI in 483 patients with HCC undergoing follow-up post hepatectomy [19], full gadoxetic acid–enhanced MRI provided significantly superior sensitivity (99% vs. 95%; p = 0.025) and accuracy (99% vs. 98%; p = 0.021) compared with non-contrast abbreviated MRI. In this study, a low-risk patient cohort followed for ≥ 1 year without HCC recurrence, non-contrast MRI did not differ significantly in diagnostic performance to gadoxetic acid–enhanced MRI at 1–2 years (sensitivity: 89% vs. 100%, n = 94) and ≥ 2 years post surgery (100%, both techniques; n = 29), suggesting that non-contrast MRI could replace full MRI in a patient subgroup at low risk of recurrence [19]. Hwang et al retrospectively compared non-contrast MRI (T1W, T2W, and DWI), with or without contrast-enhanced computed tomography (CECT), versus gadoxetic acid–enhanced MRI in patients with colorectal cancer [20]. There were no significant differences between the techniques in sensitivity, specificity, NPV, and positive predictive value (PPV) for all lesions, lesions ≤ 1.0 cm, and lesions > 1.0 cm. The authors concluded that non-contrast abbreviated MRI could be an alternative to contrast-enhanced MRI, at least in patients with a relatively high risk of CRLMs.
In conclusion, this is a relatively nascent topic. The few publications available are retrospective and likely to over-estimate sensitivity and cost savings. Components of the abbreviated protocols also varied between these studies. During the discussion at the Liver Forum, some delegates recommended that an abbreviated gadoxetic acid–enhanced MRI protocol should include HBP plus DWI, while inclusion of T2W sequence(s) was optional.
-
Consensus statement #4
-
Abbreviated gadoxetic acid–enhanced MRI protocols can be considered a method of screening and surveillance for HCC in at-risk patients, with the caveat that there is appropriate expertise available (44/80; 55% agreement. Consensus was not reached).
-
Notes: Insufficient evidence is available for recommending the frequency of MRI surveillance (annual vs. biannual) or the method to assess diagnostic performance (per lesion/per patient). The cost-effectiveness of this approach may be possible to establish, but is dependent on reimbursement levels and the risk for developing HCC. Standardized criteria for imaging features in an abbreviated protocol should be developed.
-
Consensus statement #5
-
Abbreviated gadoxetic acid–enhanced MRI can be considered a method for follow-up in patients at risk of or with known colorectal liver metastases, with the caveat that a full staging method of imaging is required at baseline (45/76; 59% agreement. Consensus was not reached).
Evaluation of treatment response of liver metastases and clinical impact
Response prediction and assessing response to systemic therapy
Pre-operative chemotherapy is commonly used in patients with resectable liver metastatic disease to improve survival [21, 22], although the benefit of this intervention remains equivocal [23, 24]. Radiologic response to pre-operative chemotherapy is associated with better survival post-resection [25]. Thus, accurate predictors of response at baseline imaging are desired. Furthermore, the Response Evaluation Criteria in Solid Tumors (RECIST 1.1) is recognized to have shortcomings using size measurements only to assess response [26, 27]. In consequence, novel functional and morphologic imaging parameters are being investigated.
Prediction of therapy response in baseline MRI
Murata et al performed a retrospective study to assess whether gadoxetic acid–enhanced MRI could predict response to chemotherapy in patients with CRLMs [28]. Relative tumor enhancement compared with surrounding liver parenchyma, measured in the HBP, was higher in responders than non-responders (37.2% ± 10.9% vs. 17.9% ± 10.5%, respectively; p = < 0.001). Using a relative tumor enhancement cut-off value of 24.2%, the sensitivity and specificity for detection of responders were 93.3% and 72.7%, respectively. The authors hypothesized that OATP1B3 expression on tumors and gadoxetic acid uptake may be associated with chemotherapeutic response.
Another retrospective study assessed a scoring system based on three gadoxetic acid–enhanced MRI features—overall heterogeneity, tumor–liver interface, and peripheral rim enhancement—to predict response to chemotherapy in patients with CRLMs [29]. On multiple-regression analysis, residual vital tumor (the primary outcome) was statistically associated with the scoring system (p < 0.001), chemotherapy response group (p < 0.001), and apparent diffusion coefficient (ADC) (p < 0.021).
Response assessment beyond RECIST
Hosseini-Nik et al performed gadoxetic acid–enhanced MRI, including DWI after chemotherapy in patients scheduled for liver resection to derive ADC, normalized relative enhancement, and relative signal intensity difference (RSID) for liver parenchyma versus metastases [30]. Patients who showed a complete response at post-surgical histopathology had significantly higher ADC (p = 0.03) and lower RSID (p = 0.008) than patients with partial response. Combination of these indices (i.e., ADC = 1.25–1.9 × 10-3 mm2/s, normalized relative enhancement = 0–35%, and RSID < 120) had 60% sensitivity and 100% specificity for detection of complete pathologic response.
In conclusion, gadoxetic acid–enhanced MRI shows promise for predicting and assessing the response to systemic chemotherapy.
Pre-surgical or pre-interventional planning after systemic therapy
Imaging for pre-surgical/pre-interventional assessment should be highly sensitive for detecting metastatic burden [31]. Gadoxetic acid–enhanced MRI and CECT were prospectively compared for the pre-operative detection of 151 histologically confirmed CRLM in patients who underwent chemotherapy [31]. Gadoxetic acid–enhanced MRI had significantly higher sensitivity for detection of CRLM ≤ 1.0 cm (86% vs. 46%; p < 0.001), a lower rate of indeterminate diagnosis (7% vs. 33%; p < 0.001), and higher interobserver concordance in characterizing lesions ≤ 1.0 cm (72% vs. 51%; p = 0.041). The authors noted that the higher lesion yield of gadoxetic acid–enhanced MRI than CECT would have changed the surgical plan in 45% of patients.
“Disappearing” liver metastases (DLMs) disappear or become occult on imaging after pre-operative chemotherapy. In general, factors pre-disposing to DLMs are small baseline lesion size (< 2 cm), increased number of treatment cycles, oxaliplatin-based therapy, increased number of CRLMs (≥ 3), and synchronous CRLMs [32]. Despite a complete radiologic response, however, up to 80% DLMs on CECT show microscopic residual disease at the anatomic location and 60–74% DLMs re-appear in situ [33, 34]. Due to a higher lesion detection rate of MRI compared to CECT and a lower impairment of the sensitivity of MRI by therapy-induced changes, pre-operative contrast-enhanced MRI (and particularly gadoxetic acid–enhanced MRI) show a higher sensitivity for correct DLM assessment [32]. The outcomes of three retrospective studies reporting the role of gadoxetic acid–enhanced MRI to assess DLMs are summarized in Table 1.
Sinusoidal obstruction syndrome (SOS) is an adverse effect of pre-operative systemic chemotherapy in CRLM, with a reported incidence of 42–51%. SOS can lead to diffuse hepatopathy, focal hepatopathy, and focal nodular hyperplasia-like nodules [38], which is associated with higher post-operative morbidity and mortality. Gadoxetic acid–enhanced MRI typically identifies SOS as a diffuse hypointensity on HBP imaging, with a high specificity (96–100%) and good interobserver agreement [39]. This led the European Society of Gastrointestinal and Abdominal Radiology to recommend gadoxetic acid–enhanced MRI for the diagnosis of SOS in patients with chemotherapy-treated CRLM [40].
-
Consensus statement #6
-
Pre-surgical or pre-interventional planning of liver metastases after systemic therapy is best assessed with gadoxetic acid–enhanced MRI (65/77; 84% agreement).
-
Consensus statement #7
-
Gadoxetic acid–enhanced MRI (including DWI) is superior to computed tomography (CT) for the assessment of disappearing liver metastases from colorectal cancer after systemic therapy, although the disappearance of liver metastases on gadoxetic acid–enhanced MRI does not indicate a complete pathologic response (77/81; 95% agreement).
International diagnostic HCC guidelines and LI-RADS
Imaging-based diagnostic systems for HCC have been published by numerous specialist societies [41]. Notably, all recent guidelines included gadoxetic acid–enhanced MRI in their diagnostic algorithms [6, 42,43,44,45,46,47].
There is a lack of standardization across HCC guidelines on the target populations requiring surveillance, diagnosis, staging, or monitoring; the imaging modalities and imaging criteria adopted; and treatment practices [48]. These differences are illustrated in Table 2, which compares the imaging components used for the diagnosis of HCC by five international guidelines. Essentially, there is not complete agreement in the use of any imaging components between these guidelines.
There is a notable divergence in treatment approaches between the North American/European guidelines and those from Asia. In North America and Europe, the diagnostic criteria are designed to achieve high specificity for the diagnosis of definite HCC (“the liver transplant setting”). In Asia, by contrast, diagnostic criteria favor high sensitivity for the detection of early-stage HCC (“the local treatment setting”) [41].
Standardization of imaging criteria and treatment practices across HCC guidelines represents a long-term objective—although the recent integration of LI-RADS into AASLD practice guidelines represents an early step to achieving this goal [5]. Standardization of terminology across HCC guidelines is a more achievable objective. This would encourage the development of registries and sharing of scientific data between centers, while in the clinical practice setting, it would reduce ambiguities or inaccurate communication [49]. LI-RADS has been developing a lexicon for definitions and reporting since 2011 and will continue to refine this in future updates [50].
-
Consensus statement #8
-
To facilitate research, enable meta-analysis, and improve patient care, international guidelines should adopt the LI-RADS terminology and recommend the use of standardized reporting for the radiologic diagnosis of HCC (60/71; 85% agreement).
Caveat: This consensus statement relates to LI-RADS terms and definitions, not to LI-RADS diagnostic criteria and categories. Thus, radiologists and other specialists caring for patients with liver disease are encouraged to use the LI-RADS terms and definitions for clinical care and publications, even if a LI-RADS algorithm is not applied.
Gadoxetic acid–enhanced MRI for staging, treatment decision-making, and follow-up of HCC
Treatment options
The Barcelona Clinic Liver Cancer (BCLC) staging system is a widely used and validated algorithm that selects treatments based on tumor burden, liver function, and performance status [42]. Alternative treatment algorithms have also evolved [43, 51], primarily reflecting recent changes in the treatment strategies for intermediate HCC [52]. In all algorithms, imaging criteria underpin treatment decision-making, providing information on lesion location, number, size, and stage.
Staging
The staging performance of gadoxetic acid–enhanced dynamic MRI and CECT was retrospectively compared in 195 patients with HCC, relative to the final BCLC staging [53]. Gadoxetic acid–enhanced MRI provided significantly greater sensitivity (91% vs. 80%; p < 0.0001) and more accurate BCLC staging (93% vs. 81%; p < 0.0001) than CECT. BCLC stage was correctly changed by gadoxetic acid–enhanced MRI in 14% (27/195) of patients who showed a difference between the CECT-derived and the final BCLC stage.
Therapy planning (resection, transplantation, local ablation)
Lee et al assessed the ability of gadoxetic acid–enhanced MRI to predict HCC recurrence in a retrospective study of 122 patients before living donor liver transplantation [54]. Independent predictors of HCC recurrence were being “beyond the Milan criteria” (HR: 3.54; p = 0.030) and peritumoral hypointensity on HBP imaging (HR: 18.30; p < 0.001). HBP MRI had a 90% accuracy to categorize the Milan criteria when compared with pathology on the explanted liver. Peritumoral hypointensity on HBP was significantly associated with worse tumor grade (p = 0.01) and microvascular invasion (MVI) (p < 0.001).
Another retrospective study assessed whether HBP imaging, in addition to dynamic imaging, improved the diagnostic performance of gadoxetic acid–enhanced liver MRI in patients with HCC who underwent transplantation [55]. HBP imaging significantly improved sensitivity for lesion detection compared with dynamic imaging, particularly for 1–2-cm HCCs (21% vs. 45%, respectively, reader 1 [R1]; 28% vs. 41%, reader 2 [R2]). The accuracy of patient allocation based on Milan criteria also improved from 89% with gadoxetic acid–enhanced dynamic images to 92% when adding HBP images.
The presence of HBP hypointense nodules without arterial phase hyperenhancement (APHE) on pre-operative gadoxetic acid–enhanced MRI was reported by Lee et al to be a significant predictor of recurrence-free survival (RFS) after hepatic resection and radiofrequency ablation (RFA) [56]. In patients with HBP hypointense nodules without APHE, 5-year RFS was 34% after hepatic resection and 28% after RFA (p = 0.618). In patients without HBP hypointense nodules and APHE, 5-year RFS was superior after hepatic resection compared to RFA (65% versus 51%; p = 0.042), due to a lower incidence of local tumor progression post resection. The absence of HBP hypointense nodules without APHE on gadoxetic acid–enhanced MR may help to select treatment, but further research on the optimal treatment of such lesions is required.
The prospective, randomized SORAMIC trial assessed the improvement in survival from selective internal radiation therapy combined with sorafenib versus sorafenib alone in patients with advanced HCC (palliative arm), as well as assessing the improvement in time to recurrence from adjuvant sorafenib after local ablation versus local ablation alone in patients with early HCC (curative arm). A SORAMIC substudy compared the accuracy of baseline gadoxetic acid–enhanced MRI, using criteria developed by Renzulli et al [57], relative to multi-slice CECT and dynamic MRI, using the European Association for the Study of the Liver (EASL) criteria, for stratifying patients to palliative or curative treatment [58]. Gadoxetic acid–enhanced MRI provided superior accuracy for treatment decision-making (83% and 81%, respectively, R1 and R2; intent-to-treat population n = 530; p < 0.001) compared with CECT (74% and 71%) and dynamic MRI (76% and 70%, respectively).
Follow-up criteria
The RECIST criteria have a number of limitations in assessing HCC response: RECIST-assessed expected tumor shrinkage can underestimate the response to therapy; the criteria demand strict requirements for patient selection and cannot be used in routine clinical practice [59]; furthermore, the RECIST criteria were designed for cytotoxic agents. With the increasing use of biologic and locoregional therapies (LRT), assessment of tumor size has a limited role for response assessment [60]. The modified RECIST (mRECIST), EASL, and LI-RADS use contrast-enhanced images that correlate more accurately with residual disease burden and survival in patients treated with ablation, transarterial chemoembolization, and radioembolization [6, 61,62,63,64,65].
Gordic et al compared RECIST, mRECIST, EASL, degree of tumor necrosis on subtraction MRI, and DWI for their ability to predict complete pathologic necrosis in patients with HCC undergoing liver transplantation after LRT for bridging [66]. EASL, mRECIST, dynamic phase subtraction images, and qualitative DWI were significant predictors of complete pathologic necrosis (p < 0.001), while RECIST and ADC were not. Subtraction showed the strongest correlation with pathologic degree of tumor necrosis (r = 0.71–0.72; p < 0.0001) and was recommended by the authors for assessing HCC response to LRT when using MRI.
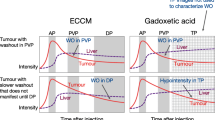
Follow-up post-ablation and resection
In patients at risk of early HCC recurrence, accurate early diagnosis may help to select patients for salvage therapy. Rimola et al prospectively followed 34 patients with HCC who had a complete response to resection and/or ablation, in whom 53 new focal lesions (enhancing in the arterial phase without washout) were detected with extracellular contrast-enhanced MRI (EC-MRI) during follow-up [67]. The combination of HBP hypointensity on gadoxetic acid–enhanced MRI and hyperintensity on DWI had high specificity (91%) and PPV (96%), but limited sensitivity (55%), for the detection of HCC recurrence prior to confident diagnosis by histopathology or EC-MRI.
Follow-up post-radioembolization
Radioembolization using β-emitting yttrium-90 microspheres is increasingly used to treat primary and metastatic liver cancers. For assessing tumor response to radioembolization, Joo et al suggest that imaging changes in size, enhancing tumor burden, and diffusion restriction together with serum tumor markers can be useful, particularly in combination [68]. Gadoxetic acid–enhanced MRI additionally provides functional information on hepatocyte uptake during treatment that may be useful for evaluating the extent of radiation effects on liver parenchyma [68].
Schelhorn et al compared gadobutrol (Gadovist/Gadavist®)-enhanced MRI against gadoxetic acid–enhanced MRI, with and without HBP imaging, for assessing response after radioembolization [69]. Patients with HCC underwent MRI on consecutive days before radioembolization and 30, 90, 180, and 270 days post-radioembolization. Tumor progression was confirmed in 14/82 study visits by CT combined with α-fetoprotein or γ-glutamyl transferase assessment. The sensitivity and specificity of gadoxetic acid–enhanced MRI with HBP imaging (0.929 and 0.971, respectively) were higher than gadoxetic acid–enhanced MRI without HBP imaging (0.786 and 0.941) or gadobutrol-enhanced MRI (0.643 and 0.956).
Follow-up post chemoembolization
HCC is 6.5-fold more likely to recur in the first year post chemoembolization than in the second [70]. Reflecting this, 3-monthly imaging is recommended in the first year post treatment, with increased imaging intervals subsequently [6, 42]. There is no evidence to demonstrate the superiority of one technique (i.e., gadoxetic acid–enhanced MRI, EC-MRI, or CT) over another for assessment of response post-chemoembolization.
Follow-up using radiogenomics and radiomics
The potential of radiomics-based approaches to predict response and survival in HCC is an area of active investigation [71, 72]. A preliminary study in 38 patients with HCC demonstrated a correlation between phenotypic MRI/CT imaging traits (including infiltrative pattern, mosaic appearance, presence of macrovascular invasion, size > 5 cm) and gene signatures for aggressive HCC [73].
Yang et al described the development of a nomogram incorporating clinic-radiologic risk factors and radiomics features derived from gadoxetic acid–enhanced MRI HBP images for the pre-operative prediction of individualized risk of MVI in patients with HCC [74].
-
Consensus statement #9
-
Evaluation of HCC response includes tumor size and degree of enhancement/necrosis based on dynamic MRI or CT, as well as assessment of new lesions (70/79; 89% agreement).
-
Consensus statement #10
-
Gadoxetic acid–enhanced MRI is accurate for the staging of HCC before and after treatment with locoregional/biologic therapies (63/71; 89% agreement).
Future possible indications of gadoxetic acid–enhanced MRI
Liver function
Chronic liver disease
Liver fibrosis is a key determinant in the natural history of chronic liver diseases. Estimating the degree of liver fibrosis is of clinical importance, because it influences the surveillance, treatment, and prognosis of disease. Gadoxetic acid uptake in the HBP is being investigated as a biomarker for liver function and staging of fibrosis and cirrhosis, as well as prediction of liver transplant graft survival and pre-operative risk assessment of liver failure after major resection [75]. Which MR-derived quantitative or semi-quantitative measures are most suitable for assessment is unresolved. The techniques summarized in Table 3 hold promise.
Hepatectomy, liver transplantation
In a retrospective study with 62 patients, Asenbaum et al [81] looked at how well functional future liver remnant (functFLR), as calculated from the RLE on gadoxetic acid–enhanced MRI and volumetry on multidetector CT done within 10 weeks of a planned major resection, predicted post-hepatectomy liver failure (PHLF) following major liver resection compared to well-established clinical tests. In a multivariate analysis, the authors found that a decreased functFLR was independently associated with the probability of PHLF (0.561; p = 0.002). Comparing receiver operating characteristic curves, functFLR showed a significantly higher area under the curve (0.904; p < 0.001) than established variables. The authors concluded that functFLR seems to be superior to established variables in the prediction of PHLF after major liver resection.
Wibmer et al evaluated gadoxetic acid–enhanced MRI in liver transplant recipients with regard to graft function and mortality at 1 year from imaging [82]. Impaired HBP excretion, defined as absence of gadoxetic acid visualization in the common bile duct 20 min after injection, was identified in 20/51 patients after transplantation. The impaired excretion group had significantly higher serum bilirubin (p < 0.001), aspartate aminotransferase (p = 0.003), alkaline phosphatase (p = 0.007), and higher median MELD score (p < 0.001). Within 1 year of MRI, 55% of these 20 patients had died (n = 7) or underwent retransplantation (n = 4), while all patients with normal HBP excretion survived without retransplantation (p < 0.001). RLE 20 min after gadoxetic acid injection was directly related to serum cholinesterase (p < 0.001) and inversely related to serum bilirubin (p = 0.0098), aspartate aminotransferase (p = 0.007), and MELD score (p < 0.001). RLE was also directly related to the probability of 1-year retransplantation-free survival (p = 0.005).
Biliary system assessment
Bile leakage is a common complication of abdominal surgical procedures and its precise localization is important for selecting optimal management [83]. A retrospective analysis in 34 patients with suspected bile leak showed that gadoxetic acid–enhanced MRI had an overall 96% sensitivity and 97% accuracy for diagnosis and location of an active bile leak [84]. Sensitivity increased in delayed HBP: from 43% for 20–25-min HBP to 93% for combined 20–25 and 60–90-min HBP, and 96% for combined 20–25, 60–90, and 150–180-min HBP.
Expanding bile leaks after blunt liver trauma require more aggressive treatment than contained leaks. The presence of expanding bile leaks was assessed by T1W MR cholangiopancreatography (MRCP) gadoxetic acid–enhanced MRC in 22 patients with recent major blunt trauma [85]. T1W MRC 30 and 90 min after gadoxetic acid administration had higher scores for biliary tree visualization and leak detection compared with 10- and 20-min acquisitions and showed an excellent interrater reliability.
T1W MRC can be useful for visualization of non-dilated duct. Biliary visualization was assessed in 29 right-liver donors using four techniques: 3D T2W MRCP, 2D T2W MRCP, breath-hold T1W hepatobiliary MRC (BH T1W MRC), and high-resolution 3D T1W hepatobiliary MR (Nav T1 MRC) using gadoxetic acid [86]. Both BH T1 MRC and Nav T1 MRC improved the accuracy of visualization and specificity of biliary diagnosis when added to 3D/2D T2W MRCP in 29 living liver donors. The Nav T1 MRC set using gadoxetic acid showed the highest diagnostic confidence and visualization scores for branching and overall ducts. In another study on living liver donors, gadoxetic acid–enhanced isotropic high-resolution (IHR) 3D T1W MRC was compared to 3D multi-slice T2W MRCP for evaluation of biliary anatomy [87]. IHR-T1W-MRC provided significantly improved visibility and sharpness of all evaluated intrahepatic bile ducts compared with 3D T2W MRCP (all p < 0.05), as well as higher overall image quality (p < 0.01). IHR-T1W-MRC also demonstrated significantly higher agreement with the reference standard than 3D T2W MRCP in bile duct variation (88% vs. 81%; p = 0.03) and expected bile duct openings (77% vs. 70%; p = 0.006).
Gadoxetic acid–enhanced MRI features were investigated for their ability to diagnose cystic fibrosis (CF)–associated liver disease (CFLD) in 50 CF patients and 40 controls [88]. Three imaging descriptors distinguished CFLD from controls: altered gallbladder morphology, periportal tracking, and periportal fat deposition. Prospective validation of this classification algorithm showed 94% sensitivity and 85% specificity for discriminating CFLD from controls. Disease severity correlated well with the imaging features.
-
Consensus statement #11
-
Gadoxetic acid uptake in the HBP may serve as a biomarker for liver function globally and segmentally, as well as assessment of liver fibrosis (64/67; 96% agreement).
-
Consensus statement #12
-
Gadoxetic acid T1W MRC can provide a functional and structural assessment of the biliary system (68/73; 93% agreement).
Summary
Delegates at the 9th International Forum debated the benefits from multidisciplinary treatment and approaches to standardizing the terminology in liver MRI, the important roles of gadoxetic acid–enhanced MRI in evaluating treatment response of liver metastases and in treatment decision-making for HCC, and the potential new indications for this imaging technique in quantifying liver and biliary system function.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- ADC:
-
Apparent diffusion coefficient
- aHR:
-
Adjusted hazard ratio
- APHE:
-
Arterial phase hyperenhancement
- BCLC:
-
Barcelona Clinic Liver Cancer
- BH:
-
Breath-hold
- cACLD:
-
Compensated advanced chronic liver disease
- CECT:
-
Contrast-enhanced computed tomography
- CES:
-
Contrast enhancement spleen index
- CES20:
-
Contrast enhancement spleen index at 20 min
- CEUS:
-
Contrast-enhanced ultrasound
- CF:
-
Cystic fibrosis
- CFLD:
-
Cystic fibrosis-associated liver disease
- CRLM:
-
Colorectal liver metastasis
- CT:
-
Computed tomography
- DLM:
-
“Disappearing” liver metastasis
- DWI:
-
Diffusion-weighted imaging
- EASL:
-
European Association for the Study of the Liver
- EC-MRI:
-
Extracellular contrast-enhanced magnetic resonance imaging
- ER:
-
Enhancement ratio
- ER15:
-
Enhancement ratio at 15 min
- FLIS:
-
Functional liver imaging score
- FLR:
-
Future liver remnant
- functFLR:
-
Functional future liver remnant
- HBP:
-
Hepatobiliary phase
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- HVPG:
-
Hepatic venous pressure gradient
- IHR:
-
Isotropic high-resolution
- LI-RADS:
-
Liver Imaging Reporting and Data System
- LRT:
-
Locoregional interventional therapies
- MELD:
-
Model of end-stage liver disease
- MRCP:
-
Magnetic resonance cholangiopancreatography
- mRECIST:
-
Modified Response Evaluation Criteria in Solid Tumors
- MRI:
-
Magnetic resonance imaging
- MVI:
-
Microvascular invasion
- Nav T1 MRC:
-
High-resolution 3D T1W hepatobiliary MR
- NPV:
-
Negative predictive value
- PHLF:
-
Post-hepatectomy liver failure
- PPV:
-
Positive predictive value
- PVHS:
-
Portal vein hyperintensity sign
- PVP:
-
Portovenous phase
- R1:
-
Reader 1
- R2:
-
Reader 2
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- RFA:
-
Radiofrequency ablation
- RFS:
-
Recurrence-free survival
- RLE:
-
Relative liver enhancement
- ROC:
-
Receiver operating characteristic
- RSID:
-
Relative signal intensity difference
- RT-CRLM:
-
Residual tiny colorectal liver metastases
- SOS:
-
Sinusoidal obstruction syndrome
- SSFSE:
-
Single-shot, fast spin-echo
- SWI:
-
Susceptibility-weighted imaging
- T1W:
-
T1-weighted
- T2W:
-
T2-weighted
- TP:
-
Transitional phase
References
Pillay B, Wootten AC, Crowe H et al (2016) The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: a systematic review of the literature. Cancer Treat Rev 42:56–72
Cancer Australia. Principles of multidisciplinary care. https://canceraustralia.gov.au/clinical-best-practice/multidisciplinary-care/all-about-multidisciplinary-care/principles-multidisciplinary-care. Accessed 28 July 2020
Commission on Cancer. A quality program of the American College of Surgeons. Draft revised standards. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/draft_coc_revised_standards_may2019.ashx. Accessed 28 July 2020
NICE Guideline 94. Multidisciplinary team meetings. https://www.nice.org.uk/guidance/ng94/evidence/29.multidisciplinary-team-meetings-pdf-172397464668. Accessed 28 July 2020
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723–750
CT/MRI LI-RADS ®v2018 CORE. https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-2018-Core.pdf?la=en. Accessed 28 July 2020
Chang TT, Sawhney R, Monto A et al (2008) Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. HPB (Oxford) 10:405–411
Yopp AC, Mansour JC, Beg MS et al (2014) Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol 21:1287–1295
Serper M, Taddei TH, Mehta R et al (2017) Association of provider specialty and multidisciplinary care with hepatocellular carcinoma treatment and mortality. Gastroenterology 152:1954–1964
Sinn DH, Choi GS, Park HC et al (2019) Multidisciplinary approach is associated with improved survival of hepatocellular carcinoma patients. PLoS One 14:e0210730
Charriere B, Muscari F, Maulat C et al (2017) Outcomes of patients with hepatocellular carcinoma are determined in multidisciplinary team meetings. J Surg Oncol 115:330–336
Engstrand J, Kartalis N, Stromberg C et al (2017) The impact of a hepatobiliary multidisciplinary team assessment in patients with colorectal cancer liver metastases: a population-based study. Oncologist 22:1067–1074
Adam R, de Gramont A, Figueras J et al (2015) Managing synchronous liver metastases from colorectal cancer: a multidisciplinary international consensus. Cancer Treat Rev 41:729–741
Zech CJ, Ba-Ssalamah A, Berg T et al (2020) Consensus report from the 8th International Forum for Liver Magnetic Resonance Imaging. Eur Radiol 30:370–382
Marks RM, Ryan A, Heba ER et al (2015) Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR Am J Roentgenol 204:527–535
Tillman BG, Gorman JD, Hru JM et al (2018) Diagnostic per-lesion performance of a simulated gadoxetate disodium-enhanced abbreviated MRI protocol for hepatocellular carcinoma screening. Clin Radiol 73:485–493
Besa C, Lewis S, Pandharipande PV et al (2017) Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdom Radiol (NY) 42:179–190
Canellas R, Patel MJ, Agarwal S, Sahani DV (2019) Lesion detection performance of an abbreviated gadoxetic acid-enhanced MRI protocol for colorectal liver metastasis surveillance. Eur Radiol 29:5852–5860
Min JH, Kim YK, Choi SY et al (2018) Detection of recurrent hepatocellular carcinoma after surgical resection: non-contrast liver MR imaging with diffusion-weighted imaging versus gadoxetic acid-enhanced MR imaging. Br J Radiol 91:20180177
Hwang JA, Kim YK, Min JH, Song KD, Sohn I, Ahn HS (2019) Non-contrast liver MRI as an alternative to gadoxetic acid-enhanced MRI for liver metastasis from colorectal cancer. Acta Radiol 60:441–450
Khoo E, O'Neill S, Brown E, Wigmore SJ, Harrison EM (2016) Systematic review of systemic adjuvant, neoadjuvant and perioperative chemotherapy for resectable colorectal-liver metastases. HPB (Oxford) 18:485–493
Mitchell D, Puckett Y, Nguyen QN (2019) Literature review of current management of colorectal liver metastasis. Cureus 11:e3940
Nordlinger B, Sorbye H, Glimelius B et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14:1208–1215
Bridgewater JA, Pugh SA, Maishman T et al (2020) Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis (New EPOC): long-term results of a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 21:398–411
Shindoh J, Loyer EM, Kopetz S et al (2012) Optimal morphologic response to preoperative chemotherapy: an alternate outcome end point before resection of hepatic colorectal metastases. J Clin Oncol 30:4566–4572
Kuhl CK, Alparslan Y, Schmoee J et al (2019) Validity of RECIST Version 1.1 for response assessment in metastatic cancer: a prospective, multireader study. Radiology 290:349–356
Van Cutsem E, Verheul HM, Flamen P et al (2016) Imaging in colorectal cancer: progress and challenges for the clinicians. Cancers (Basel) 8:E81. https://doi.org/10.3390/cancers8090081
Murata S, Matsushima S, Sato Y et al (2018) Predicting chemotherapeutic response for colorectal liver metastases using relative tumor enhancement of gadoxetic acid disodium-enhanced magnetic resonance imaging. Abdom Radiol (NY) 43:3301–3306
Costa NVVP, Bastati N, Pötter-Lang S, Guengoern Z, Bican Y, Ba-Ssalamah A. Predicting the response of colorectal cancer liver metastases to preoperative chemotherapy using gadoxetic acid-enhanced MRI. Abstract presented at European College of Radiology: B-1077. Available at https://link.springer.com/content/pdf/10.1007/s13244-018-0603-8.pdf. Presented at: European College of Radiology. Accessed 28 July 2020
Hosseini-Nik H, Fischer SE, Moulton CA et al (2016) Diffusion-weighted and hepatobiliary phase gadoxetic acid-enhanced quantitative MR imaging for identification of complete pathologic response in colorectal liver metastases after preoperative chemotherapy. Abdom Radiol (NY) 41:231–238
Jhaveri KS, Fischer SE, Hosseini-Nik H et al (2017) Prospective comparison of gadoxetic acid-enhanced liver MRI and contrast-enhanced CT with histopathological correlation for preoperative detection of colorectal liver metastases following chemotherapy and potential impact on surgical plan. HPB (Oxford) 19:992–1000
Tsilimigras DI, Ntanasis-Stathopoulos I, Paredes AZ et al (2019) Disappearing liver metastases: a systematic review of the current evidence. Surg Oncol 29:7–13
van Vledder MG, de Jong MC, Pawlik TM, Schulick RD, Diaz LA, Choti MA (2010) Disappearing colorectal liver metastases after chemotherapy: should we be concerned? J Gastrointest Surg 14:1691–1700
Benoist S, Brouquet A, Penna C et al (2006) Complete response of colorectal liver metastases after chemotherapy: does it mean cure? J Clin Oncol 24:3939–3945
Park MJ, Hong N, Han K et al (2017) Use of imaging to predict complete response of colorectal liver metastases after chemotherapy: MR imaging versus CT imaging. Radiology 284:423–431
Owen JW, Fowler KJ, Doyle MB, Saad NE, Linehan DC, Chapman WC (2016) Colorectal liver metastases: disappearing lesions in the era of Eovist hepatobiliary magnetic resonance imaging. HPB (Oxford) 18:296–303
Kim SS, Song KD, Kim YK et al (2017) Disappearing or residual tiny (</=5 mm) colorectal liver metastases after chemotherapy on gadoxetic acid-enhanced liver MRI and diffusion-weighted imaging: is local treatment required? Eur Radiol 27:3088–3096
Nakano H, Oussoultzoglou E, Rosso E et al (2008) Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg 247:118–124
Shin NY, Kim MJ, Lim JS et al (2012) Accuracy of gadoxetic acid-enhanced magnetic resonance imaging for the diagnosis of sinusoidal obstruction syndrome in patients with chemotherapy-treated colorectal liver metastases. Eur Radiol 22:864–871
Neri E, Bali MA, Ba-Ssalamah A et al (2016) ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol 26:921–931
Kim TH, Kim SY, Tang A, Lee JM (2019) Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma: 2018 update. Clin Mol Hepatol 25:245–263
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Kokudo N, Takemura N, Hasegawa K et al (2019) Clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatol Res 49:1109–1113
Korean Liver Cancer Association (2019) 2018 Korean Liver Cancer Association-National Cancer Center Korea Practice guidelines for the management of hepatocellular carcinoma. Gut Liver 13:227–299
Omata M, Cheng AL, Kokudo N et al (2017) Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 11:317–370
Rao SX, Wang J, Wang J et al (2019) Chinese consensus on the clinical application of hepatobiliary magnetic resonance imaging contrast agent: gadoxetic acid disodium. J Dig Dis 20:54–61
Zhou J, Sun HC, Wang Z et al (2018) Guidelines for diagnosis and treatment of primary liver cancer in China (2017 edition). Liver Cancer 7:235–260
Tang A, Cruite I, Mitchell DG, Sirlin CB (2018) Hepatocellular carcinoma imaging systems: why they exist, how they have evolved, and how they differ. Abdom Radiol (NY) 43:3–12
Corwin MT, Lee AY, Fananapazir G, Loehfelm TW, Sarkar S, Sirlin CB (2018) Nonstandardized terminology to describe focal liver lesions in patients at risk for hepatocellular carcinoma: implications regarding clinical communication. AJR Am J Roentgenol 210:85–90
Elsayes KM, Kielar AZ, Chernyak V et al (2019) LI-RADS: a conceptual and historical review from its beginning to its recent integration into AASLD clinical practice guidance. J Hepatocell Carcinoma 6:49–69
Kudo M, Trevisani F, Abou-Alfa GK, Rimassa L (2016) Hepatocellular carcinoma: therapeutic guidelines and medical treatment. Liver Cancer 6:16–26
Ikeda M, Han K-W, Miyayama S et al (2019) Changing paradigm of treatment strategy for intermediate stage HCC: APPLE Expert Consensus. Liver Cancer 8(Suppl 1):13
Choi SH, Byun JH, Kwon HJ et al (2015) The usefulness of gadoxetic acid-enhanced dynamic magnetic resonance imaging in hepatocellular carcinoma: toward improved staging. Ann Surg Oncol 22:819–825
Lee S, Kim KW, Jeong WK et al (2019) Gadoxetic acid-enhanced MRI as a predictor of recurrence of HCC after liver transplantation. Eur Radiol. https://doi.org/10.1007/s00330-019-06424-0
Lee DH, Lee JM, Baek JH, Shin CI, Han JK, Choi BI (2015) Diagnostic performance of gadoxetic acid-enhanced liver MR imaging in the detection of HCCs and allocation of transplant recipients on the basis of the Milan criteria and UNOS guidelines: correlation with histopathologic findings. Radiology 274:149–160
Lee DH, Lee JM, Yu MH et al (2019) Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MR can help determine the treatment method for HCC. Eur Radiol 29:3122–3131
Renzulli M, Biselli M, Brocchi S et al (2018) New hallmark of hepatocellular carcinoma, early hepatocellular carcinoma and high-grade dysplastic nodules on Gd-EOB-DTPA MRI in patients with cirrhosis: a new diagnostic algorithm. Gut 67:1674–1682
Ricke J, Bartolozzi C, Berg T, et al The impact of gadoxetic acid enhanced hepato-biliary MRI on treatment decisions in hepatocellular carcinoma: the SORAMIC trial diagnostic cohort. Presented at: Radiological Society of North America, Chicago, IL
Liu Q, Li A, Sun S, Luo R, Chen F (2014) The true role of mRECIST guideline: does it really estimate viable tumor or merely improve accuracy in hepatocellular carcinoma response evaluation? J BUON 19:398–405
Dimitroulis D, Damaskos C, Valsami S et al (2017) From diagnosis to treatment of hepatocellular carcinoma: an epidemic problem for both developed and developing world. World J Gastroenterol 23:5282–5294
Bargellini I, Bozzi E, Campani D et al (2013) Modified RECIST to assess tumor response after transarterial chemoembolization of hepatocellular carcinoma: CT-pathologic correlation in 178 liver explants. Eur J Radiol 82:e212–e218
Forner A, Ayuso C, Varela M et al (2009) Evaluation of tumor response after locoregional therapies in hepatocellular carcinoma: are response evaluation criteria in solid tumors reliable? Cancer 115:616–623
Gillmore R, Stuart S, Kirkwood A et al (2011) EASL and mRECIST responses are independent prognostic factors for survival in hepatocellular cancer patients treated with transarterial embolization. J Hepatol 55:1309–1316
Riaz A, Memon K, Miller FH et al (2011) Role of the EASL, RECIST, and WHO response guidelines alone or in combination for hepatocellular carcinoma: radiologic-pathologic correlation. J Hepatol 54:695–704
Yeo DM, Choi JI, Lee YJ, Park MY, Chun HJ, Lee HG (2014) Comparison of RECIST, mRECIST, and Choi criteria for early response evaluation of hepatocellular carcinoma after transarterial chemoembolization using drug-eluting beads. J Comput Assist Tomogr 38:391–397
Gordic S, Corcuera-Solano I, Stueck A et al (2017) Evaluation of HCC response to locoregional therapy: validation of MRI-based response criteria versus explant pathology. J Hepatol 67:1213–1221
Rimola J, Forner A, Sapena V et al (2020) Performance of gadoxetic acid MRI and diffusion-weighted imaging for the diagnosis of early recurrence of hepatocellular carcinoma. Eur Radiol 30:186–194
Joo I, Kim HC, Kim GM, Paeng JC (2018) Imaging evaluation following (90) Y radioembolization of liver tumors: what radiologists should know. Korean J Radiol 19:209–222
Schelhorn J, Best J, Reinboldt MP et al (2015) Therapy response assessment after radioembolization of patients with hepatocellular carcinoma--comparison of MR imaging with gadolinium ethoxybenzyl diethylenetriamine penta-acetic acid and gadobutrol. J Vasc Interv Radiol 26:972–979
Boas FE, Do B, Louie JD et al (2015) Optimal imaging surveillance schedules after liver-directed therapy for hepatocellular carcinoma. J Vasc Interv Radiol 26:69–73
Cozzi L, Dinapoli N, Fogliata A et al (2017) Radiomics based analysis to predict local control and survival in hepatocellular carcinoma patients treated with volumetric modulated arc therapy. BMC Cancer 17:829
Saini A, Breen I, Pershad Y et al (2018) Radiogenomics and radiomics in liver cancers. Diagnostics (Basel) 9:4
Taouli B, Hoshida Y, Kakite S et al (2017) Imaging-based surrogate markers of transcriptome subclasses and signatures in hepatocellular carcinoma: preliminary results. Eur Radiol 27:4472–4481
Yang L, Gu D, Wei J et al (2018) Radiomics nomogram for preoperative prediction of microvascular invasion in hepatocellular carcinoma. Liver Cancer 8:373–386
Ba-Ssalamah A, Bastati N, Wibmer A et al (2017) Hepatic gadoxetic acid uptake as a measure of diffuse liver disease: Where are we? J Magn Reson Imaging 45:646–659
Feier D, Balassy C, Bastati N, Fragner R, Wrba F, Ba-Ssalamah A (2016) The diagnostic efficacy of quantitative liver MR imaging with diffusion-weighted, SWI, and hepato-specific contrast-enhanced sequences in staging liver fibrosis--a multiparametric approach. Eur Radiol 26:539–546
Bastati N, Beer L, Mandorfer M et al (2020) Does the functional liver imaging score derived from gadoxetic acid-enhanced MRI predict outcomes in chronic liver disease? Radiology 294:98–107
Beer L, Mandorfer M, Bastati N et al (2019) Inter- and intra-reader agreement for gadoxetic acid-enhanced MRI parameter readings in patients with chronic liver diseases. Eur Radiol 29:6600–6610
Asenbaum U, Ba-Ssalamah A, Mandorfer M et al (2017) Effects of portal hypertension on gadoxetic acid-enhanced liver magnetic resonance: diagnostic and prognostic implications. Invest Radiol 52:462–469
Sandrasegaran K, Cui E, Elkady R et al (2018) Can functional parameters from hepatobiliary phase of gadoxetate MRI predict clinical outcomes in patients with cirrhosis? Eur Radiol 28:4215–4224
Asenbaum U, Kaczirek K, Ba-Ssalamah A et al (2018) Post-hepatectomy liver failure after major hepatic surgery: not only size matters. Eur Radiol 28:4748–4756
Wibmer A, Aliya Q, Steininger R et al (2012) Liver transplantation: impaired biliary excretion of gadoxate is associated with an inferior 1-year retransplantation-free survival. Invest Radiol 47:353–358
Petrillo M, Ierardi AM, Tofanelli L et al (2019) Gd-EOB-DTP-enhanced MRC in the preoperative percutaneous management of intra and extrahepatic biliary leakages: does it matter? Gland Surg 8:174–183
Cieszanowski A, Stadnik A, Lezak A et al (2013) Detection of active bile leak with Gd-EOB-DTPA enhanced MR cholangiography: comparison of 20-25 min delayed and 60-180 min delayed images. Eur J Radiol 82:2176–2182
Wong YC, Wang LJ, Wu CH et al (2018) Detection and characterization of traumatic bile leaks using Gd-EOB-DTPA enhanced magnetic resonance cholangiography. Sci Rep 8:14612
Lee JH, Kim B, Kim HJ, Kim BW, Wang HJ, Kim JK (2018) High spatial resolution navigated 3D T1-weighted hepatobiliary MR cholangiography using Gd-EOB-DTPA for evaluation of biliary anatomy in living liver donors. Abdom Radiol (NY) 43:1703–1712
Kang HJ, Lee JM, Ahn SJ et al (2019) Clinical feasibility of gadoxetic acid-enhanced isotropic high-resolution 3-dimensional magnetic resonance cholangiography using an iterative denoising algorithm for evaluation of the biliary anatomy of living liver donors. Invest Radiol 54:103–109
Poetter-Lang S, Staufer K, Baltzer P et al (2019) The efficacy of MRI in the diagnostic workup of cystic fibrosis-associated liver disease: a clinical observational cohort study. Eur Radiol 29:1048–1058
Acknowledgments
Medical writing assistance provided by Bill Wolvey at Parexel was funded by Bayer.
Funding
This study received funding from Bayer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dow-Mu Koh, MD.
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
Dow-Mu Koh: None
Ahmed Ba-Ssalamah: Consultant: Bayer AG
Giuseppe Brancatelli Consultant: Bayer AG
Ghaneh Fananapazir: None
M. Isabel Fiel: Consultant Alexion Biopharma, Progenity; Author royalties: Wolters Kluwer
Satoshi Goshima: None
Sheng-Hong Ju: None
Nikolaos Kartalis: None
Masatoshi Kudo: None
Jeong Min Lee: None
Takamichi Murakami: None
Max Seidensticker: Research grants: Bayer, Boston Scientific, SIRTEX Medical; Lecture fees: Bayer, Boston Scientific, Cook, Falk Foundation, Siemens, SIRTEX
Claude B. Sirlin: Financial disclosures: educational materials royalties: Wolters Kluwer; Research grants: Bayer, Foundation of NIH, GE, Gilead, Philips, Siemens; Consulting: Blade, Boehringer Ingelheim, Epigenomics; Consulting under auspices of university: AMRA, BMS, Exact Sciences, GE Digital, IBM-Watson; Core lab services: Enanta, Gilead, ICON, Intercept, Nusirt, Shire, Synageva, Takeda. Non-financial disclosures: Co-Chair, LI-RADS Steering Committee; Co-Chair, LI-RADS Lexicon & Writing Group
Cher Heng Tan: None
Jin Wang: None
Jeong Hee Yoon: Consultant: Samsung Electronics; Research grants: Bayer; honoraria for lectures including speakers bureaus from Bayer and Philips Healthcare
Mengsu Zeng: None
Jian Zhou: None
Bachir Taouli: Research grants: Bayer AG, Regeneron, Takeda; Consultant: Alexion, Bayer AG
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because this is a review paper.
Ethical approval
Institutional Review Board approval was not required because this is a review paper.
Methodology
• Not applicable because this is a review paper
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 186 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koh, DM., Ba-Ssalamah, A., Brancatelli, G. et al. Consensus report from the 9th International Forum for Liver Magnetic Resonance Imaging: applications of gadoxetic acid-enhanced imaging. Eur Radiol 31, 5615–5628 (2021). https://doi.org/10.1007/s00330-020-07637-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07637-4