Abstract
Purpose
We aim to evaluate the role of biofilm-producing bacteria in the clinical response to antibiotic therapy among patients affected by chronic bacterial prostatitis (CBP).
Methods
All patients attending our centre from January to December 2008 due to prostatitis-like symptoms with a positive Meares–Stamey test were enroled. The clinical symptoms were assessed according to the NIH-CPSI, and the bacterial strains isolated from the patients enroled were identified and tested for antibiotic sensitivity using cards of the Vitek II semi-automated System for Microbiology (BioMerieux). Quantitative bacterial slime production was assessed by the Christensen microwell assay. All patients were treated with fluoroquinolones for 4 weeks and reevaluated clinically and microbiologically after 3 months.
Results
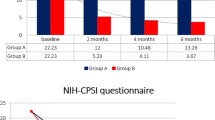
One hundred and sixteen patients were enroled, and 150 bacterial strains were isolated from all patients. About 85 % of these strains were strong or moderate biofilm producers. Patients with strong or moderate biofilm-producing bacteria had a higher NIH-CPSI symptom score than those without biofilm-producing bacteria (mean 17.6 ± 5.6 vs. 14.1 ± 3.3; p = 0.0009). At the follow-up, 68 patients (58.6 %) had negative microbiological tests, but only 11 (9.48 %) reported a reduction in NIH-CPSI score. Improvement of symptoms was found statistically significantly less frequent in patients with biofilm-producing bacteria than in those without (p = 0.03). Ultrastructural analysis showed cellular forms in active replication with aberrant morphology of unknown cause and confirmed strong slime production with consistent bacterial stratification.
Conclusion
In our CBP population, biofilm-producing bacteria were commonly found and had a significant negative impact on the clinical response to antibiotic therapy.
Similar content being viewed by others
References
Bartoletti R, Cai T, Mondaini N et al (2007) Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multi center case–control observational study. J Urol 178(6):2411–2415
Krieger JN, Nyberg L Jr, Nickel JC (1999) NIH consensus definition and classification of prostatitis. JAMA 282(3):236–237
Drach GW, Fair WR, Meares EM, Stamey TA (1978) Classification of benign diseases associated with prostatic pain: prostatitis or prostatodynia? J Urol 120(2):266
Grabe M, Bjerklund-Johansen TE, Botto H et al (2012) Guidelines on urological infections. In: Grabe M, Bjerklund-Johansen TE, Botto H, Wullt B, Çek M, Naber KG, Pickard RS, Tenke P, Wagenlehner F (eds) European Association of Urology Guidelines, ch 10.4.1, p 69
Wagenlehner FM, Naber KG (2003) Antimicrobial treatment of prostatitis. Expert Rev Anti Infect Ther 1(2):275–282
Fulmer BR, Turner TT (2000) A blood-prostate barrier restricts cell and molecular movement across the rat ventral prostate epithelium. J Urol 163(5):1591–1594
Bartoletti R, Cai T (2009) Chronic prostatitis and biofilm. Infez Med 17(1):10–16
Kanamaru S, Kurazono H, Terai A, Monden K, Kumon H, Mizunoe Y, Ogawa O, Yamamoto S (2006) Increased biofilm formation in Escherichia coli isolated from acute prostatitis. Int J Antimicrob Agents 28(1):S21–S25
Mazzoli S (2010) Biofilms in chronic bacterial prostatitis (NIH-II) and in prostatic calcifications. FEMS Immunol Med Microbiol 59(3):337–344
Porta M (ed) (2008) A dictionary of epidemiology, 5th edn. Oxford University Press, New York
Giubilei G, Mondaini N, Crisci A et al (2005) The Italian version of the National Institutes of Health Chronic Prostatitis Symptom Index. Eur Urol 47(6):805–811
Badia X, Garcia-Losa M, Dal-Re R (1997) Ten-language translation and harmonization of the International Prostate Symtom Score: developing a methodology for multinational clinical trials. Eur Urol 31(2):129–140
Christensen GD, Simpson WA, Younger JJ et al (1985) Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol 22(6):996–1006
Rubin RH, Shapiro ED, Andriole VT, Davis RJ, Stamm WE (1992) Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Infectious Diseases Society of America and the Food and Drug Administration. Clin Infect Dis 15(1):S216–S227
Trinchieri A (2001) Role of levofloxacin in the treatment of urinary tract infections. Arch Ital Urol Androl 73(2):105–113
Litwin MS, McNaughton-Collins M, Fowler FJ, Nickel JC, Calhoun EA, Pontari MA et al (1999) The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol 162:369
Mazzoli S, Cai T, Rupealta V et al (2007) Interleukin 8 and anti-chlamydia trachomatis mucosal IgA as urogenital immunologic markers in patients with C. trachomatis prostatic infection. Eur Urol 51(5):1385–1393
Cai T, Wagenlehner FM, Mazzoli S et al (2012) Semen quality in patients with Chlamydia trachomatis genital infection treated concurrently with prulifloxacin and a phytotherapeutic agent. J Androl 33(4):615–623
Nickel JC, Alexander RB, Schaeffer AJ, Landis JR, Knauss JS, Propert KJ (2003) Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol 170:818–822
Soto SM, Smithson A, Martinez JA et al (2007) Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J Urol 177(1):365–368
Donlan RM, Costerton JW (2002) Biofilm: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15:167–193
Choong S, Whitfield H (2000) Biofilms and their role in infections in urology. BJU Int 86(8):935–941
Verstraelen H, Verhelst R, Vaneechoutte M, Temmerman M (2010) The epidemiology of bacterial vaginosis in relation to sexual behaviour. BMC Infect Dis 10:81
Cai T, Mazzoli S, Meacci F, Boddi V, Mondaini N, Malossini G, Bartoletti R (2011) Epidemiological features and resistance pattern in uropathogens isolated from chronic bacterial prostatitis. J Microbiol 49(3):448–454
Bergman B, Wedren H, Holm SE (1989) Staphylococcus saprophyticus in males with symptoms of chronic prostatitis. Urology 34(5):241–245
Murphy AB, Mecejko A, Taylor A, Nadler RB (2009) Chronic prostatitis: management strategies. Drugs 69:71–84
Nickel JC, Olson ME, Barabas A, Benediktsson H, Dasgupta MK, Costerton JW (1990) Pathogenesis of chronic bacterial prostatitis in an animal model. Br J Urol 66(1):47–54
Acknowledgments
We are grateful to all participating centre’s members for their assistance and to Professor John Denton (Department of Modern Philology, University of Florence) for manuscript language revision.
Conflict of interest
Sanofi-Aventis Italia has provided technical support and funding. No author, however, has financial or commercial conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bartoletti, R., Cai, T., Nesi, G. et al. The impact of biofilm-producing bacteria on chronic bacterial prostatitis treatment: results from a longitudinal cohort study. World J Urol 32, 737–742 (2014). https://doi.org/10.1007/s00345-013-1145-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1145-9