Abstract
Background and Purpose
Dysphagia is estimated to occur in up to 50% of the stroke neurorehabilitation population. Those patients with severe neurogenic oropharyngeal dysphagia (NOD) may receive feeding gastrostomy tubes (FGT) if noninvasive therapies prove ineffective in eliminating aspiration or sustaining adequate nutritional intake. Our aim was to quantify the recovery of swallowing function, and to identify variables predictive of survival after dysphagic stroke requiring FGT placement.
Methods
We identified consecutive stroke patients with severe dysphagic stroke requiring FGT placement admitted to a rehabilitation hospital between May 1998 and October 2001. The medical records were reviewed, and demographic, clinical, videofluoroscopic (VSS) and neuroimaging information were abstracted. A follow–up telephone interview was performed to determine whether the FGT was still in use, had been removed,or if the patient had died. State death certificate records were reviewed to ascertain date of death for subjects who had expired by the time of follow–up. Univariate and multivariate analyses were performed.
Results
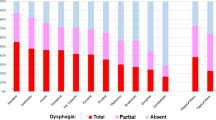
11.6 % (77/664) of stroke patients admitted during the study period had severe dysphagic stroke with FGT insertion. Follow–up was available for 66 (85.7 %) of these individuals at a mean of two years after acute stroke. On follow–up 64% (42/66) of the patients were alive and 45 % had had the FGT removed and resumed oral diets. On univariate analysis patients who were alive at the time of follow–up had received FGT feeding for a shorter period of time (p < 0.0003), showed no signs of aspiration on the Clinical Assessment of Feeding & Swallowing (CAFS,p < 0.020) and on the Videofluoroscopic Swallowing Study (VSS, 0.001), had a better discharge FIM–Score (Functional Independence Measure) for eating (p < 0.0002) and cognitive function (p < 0.002) as well as better discharge FCM–Score (Functional Communication Measure) for swallowing (p < 0.0001). On multivariate analysis we developed a model consisting of FGT removal at discharge from the rehabilitation hospital (p < 0.011) and non–aspiration during VSS (p < 0.040) that was significantly associated with longer survival time during follow–up.
Conclusions
Severe dysphagia requiring FGT is common in patients with stroke referred for neurorehabilitation. Patients who had a FGT in place at the time of discharge from the stroke rehabilitation unit or aspirated during VSS were substantially more likely to have died by the time of follow–up compared to those who had had the FGT removed and had no signs of aspiration on VSS. However functional outcome measurements (FIM, FCM) including the cognitive function (attention, concentration etc.) could play an important role for prediction of swallowing regeneration and survival in neurorehabilitation. These findings may have practical utility in guiding physicians and speech language pathologists when advising patients and families about prognosis in stroke survivors with severe dysphagia.
Similar content being viewed by others
References
ASHA (1998) The National Outcomes Measurement System (NOMS). Rockville, Maryland
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifiying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Daniels SK, Foundas AL (1999) Lesion Localization in acute stroke patients with risk of aspiration. J Neuroimag 9:91–98
Gordon C, Hewer RL, Wade DT (1987) Dysphagia in acute stroke. BMJ 293:411–414
Hamdy S, Aziz Q, Rothwell JC, Crone R, Hughes D, Tallis RC, Thompson DG (1997) Explaining oropharyngeal dysphagia after unilateral hemispheric stroke. Lancet 350:686–692
Hamdy S, Rothwell JC, Aziz Q, Thompson DG (2000) Organization and reorganization of human swallowing motor cortex: implications for recovery after stroke. Clin Sci 99:151–157
Holas MA, DiPippo KL, Reding MJ (1994) Aspiration and relative risk of medical complications following stroke. Arch Neurol 51:1051–1053
Horner J, Massey EW, Riski JE, et al. (1988) Aspiration following stroke: clinical correlates and outcome. Neurology 38:1359–1362
Ickenstein GW, Kelly PJ, Furie KL, Ambrosi D, Rallis N, Goldstein R, Horick N, Stein J (2003) Predictors of feeding gastrostomy tube (FGT) removal in stroke patients with dysphagia. J Stroke Cerebrovasc Dis 12:169–174
Jean A, Car A (1979) Inputs to swallowing medullary neuron’s from the peripheral afferent fibers and swallowing cortical area. Brain Res 178:567–572
Keith RA, Granger CV, Hamilton BB, Sherwin FS (1987) The Functional Independence Measure: a new tool for rehabilitation. In: Eisenberg MG, Grzesiak RC (eds) Advances in clinical rehabilitation. Springer Publishing, New York, pp 6–18
Kennedy JG, Kent RD (1988) Physiological substrates of normal deglutition. Dysphagia 3:24–37
Kirby DF, Craig RM, Tsang TK, Plotnick BH (1986) Percutaneous endoscopic gastrostomies: a prospective evaluation and review of the literature. J Parenter Enteral Nutr 10:155–159
Mann G, Hankey G, Cameron D (1999) Swallowing function after stroke: Prognosis and prospectic factors at 6 months. Stroke 30:744–748
Mann G, Hankey G Cameron D (2000) Swallowing disorder following acute stroke: Prevalence and diagnostic accurancy. Cerebrovasc Dis 10:380–386
Martin RE, Sessle BJ (1993) The role of the cerebral cortex in swallowing. Dysphagia 8:195–202
Miller A, Bieger D, Conklin JL (1997) Functional controls of deglutition. In: Perlman AL, Schulze-Delrieu K (eds) Deglutition and its disorders. Singular, San Diego, pp 43–97
Pallicino P, Snyder W, Granger C (1992) The NIH Stroke Scale and the FIM in stroke rehabilitation. Stroke 23:919–920
Park RHR, Allison MC, Lang J, et al. (1992) Randomized comparison of percutanous endoscopic gastrostomy and nasopharyngeal tube feeding in patients with persisting neurological dysphagia. BMJ 304:1406–1409
Sekizawa K (2002) Nasogastric tubes in patients with dysphagia. Lancet 359:80–81
Smith PM, Illig SB, Fiedler RC, Hamilton BB, Ottenbacher KJ, Fiedler RC (1996) Intermodel agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke. Arch Phys Med Rehabil 77:431–435
Smithard D, O’Neill P, Park C, Morreis J, Wyatt R, England R, Martin D (1996) Complications and outcome after acute stroke: Does dysphagia matter? Stroke 27:1200–1204
Stiegmann GV, Goff JS, Silas D, Pearlman N, Sun J, Norton L (1990) Endoscopic versus operative gastrostomy: final results of a prospective randomized trial. Gastrointest Endosc 36:1–5
Streiner DL, Norman GR (1996) A practical guide to the development and use of health measurement scales. In: Health measurement scales. Oxford University Press, New York, pp 5–24
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1996) Arterial territories of human brain: brainstem and cerebellum. Neurology 47:1125–1135
Teasell R, Foley N, McRae M, Finestone H (2001) Use of percutaneous gastrojejunostomy feeding tubes in the rehabilitation of stroke patients. Arch Phys Med Rehabil 82:1412–1415
Wiles CM (1991) Neurogenic dysphagia. J Neurol Neurosurg Psychiatry 54:1037–1039
Broadley S, Croser D, Cottrell J, Creevy M, Teo E, Yiu D, Pathi R, Taylor J, Thompson PD (2003) Predictors of prolonged dysphagia following acute stroke. J Clin Neurosci 10(3):300–305
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ickenstein, G.W., Stein, J., Ambrosi, D. et al. Predictors of survival after severe dysphagic stroke. J Neurol 252, 1510–1516 (2005). https://doi.org/10.1007/s00415-005-0906-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-005-0906-9