Abstract
Background
The functional lumen imaging probe (FLIP) is a novel diagnostic tool that can be used to measure esophagogastric junction (EGJ) distensibility. In this study, we performed intraoperative FLIP measurements during laparoscopic Heller myotomy (LHM) and peroral esophageal myotomy (POEM) for treatment of achalasia and evaluated the relationship between EGJ distensibility and postoperative symptoms.
Methods
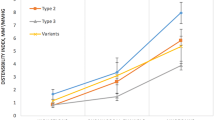
Distensibility index (DI) (defined as the minimum cross-sectional area at the EGJ divided by distensive pressure) was measured with FLIP at two time points during LHM and POEM: (1) at baseline after induction of anesthesia, and (2) after operation completion.
Results
Measurements were performed in 20 patients undergoing LHM and 36 undergoing POEM. Both operations resulted in an increase in DI, although this increase was larger with POEM (7 ± 3.1 vs. 5.1 ± 3.4 mm2/mmHg, p < .05). The two patients (both LHM) with the smallest increases in DI (1 and 1.6 mm2/mmHg) both had persistent symptoms postoperatively and, overall, LHM patients with larger increases in DI had lower postoperative Eckardt scores. In the POEM group, there was no correlation between change in DI and symptoms; however, all POEM patients experienced an increase in DI of >3 mm2/mmHg. When all patients were divided into thirds based on final DI, none in the lowest DI group (<6 mm2/mmHg) had symptoms suggestive of reflux (i.e., GerdQ score >7), as compared with 20 % in the middle third (6–9 mm2/mmHg) and 36 % in the highest third (>9 mm2/mmHg). Patients within an “ideal” final DI range (4.5–8.5 mm2/mmHg) had optimal symptomatic outcomes (i.e., Eckardt ≤ 1 and GerdQ ≤ 7) in 88 % of cases, compared with 47 % in those with a final DI above or below that range (p < .05).
Conclusions
Intraoperative EGJ distensibility measurements with FLIP were predictive of postoperative symptomatic outcomes. These results provide initial evidence that FLIP has the potential to act as a useful calibration tool during operations for achalasia.


Similar content being viewed by others
References
Triadafilopoulos G, Boeckxstaens GE, Gullo R, Patti MG, Pandolfino JE, Kahrilas PJ, Duranceau A, Jamieson G, Zaninotto G (2012) The Kagoshima consensus on esophageal achalasia. Dis Esophagus 25:337–348
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR, European Achalasia Trial I (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstatter M, Lin F, Ciovica R (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–57
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Novais PA, Lemme EM (2010) 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther 32:1257–1265
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17:228–235
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2013) A comparative study on comprehensive, objective outcomes of laparoscopic heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259(6):1098–1103
Pandolfino JE, de Ruigh A, Nicodeme F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil 25:496–501
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143:328–335
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin ZY, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Clouse RE, Staiano A, Alrakawi A, Haroian L (2000) Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol 95:2720–2730
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, International High Resolution Manometry Working G (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 24(Suppl 1):57–65
Vaziri K, Soper NJ (2008) Laparoscopic Heller myotomy: technical aspects and operative pitfalls. J Gastrointest Surg 12:1586–1591
McMahon BP, Frokjaer JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H (2007) The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol 292:G377–G384
Perretta S, McAnena O, Botha A, Nathanson L, Swanstrom L, Soper NJ, Inoue H, Ponsky J, Jobe B, Marescaux J, Dallemagne B (2013) Acta from the EndoFLIP(R) Symposium. Surg Innov
Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, Lind T (2009) Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 30:1030–1038
Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ (2010) Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 72:272–278
Mattioli S, Ruffato A, Lugaresi M, Pilotti V, Aramini B, D’Ovidio F (2010) Long-term results of the Heller-Dor operation with intraoperative manometry for the treatment of esophageal achalasia. J Thorac Cardiovasc Surg 140:962–969
Endo S, Nakajima K, Nishikawa K, Takahashi T, Souma Y, Taniguchi E, Ito T, Nishida T (2009) Laparoscopic Heller-Dor surgery for esophageal achalasia: impact of intraoperative real-time manometric feedback on postoperative outcomes. Dig Surg 26:342–348
Chapman JR, Joehl RJ, Murayama KM, Tatum RP, Shi G, Hirano I, Jones MP, Pandolfino JE, Kahrilas PJ (2004) Achalasia treatment: improved outcome of laparoscopic myotomy with operative manometry. Arch Surg 139:508–513 discussion 13
Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, Luketich JD (2009) Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery 146:826–831 discussion 31-3
Acknowledgments
The authors would like to acknowledge Rowena Martinez, RN, and Colleen Krantz, RN, for their help coordinating the clinical aspects of this study. This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases Grant R01 DK-079902 (J.E. Pandolfino).
Disclosures
Nathaniel Soper is on the scientific advisory boards of TransEnterix and Miret Surgical, which are unrelated to this study. Ezra Teitelbaum, John Pandolfino, Peter Kahrilas, Lubomyr Boris, Frederic Nicodeme, Zhiyue Lin, and Eric Hungness have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teitelbaum, E.N., Soper, N.J., Pandolfino, J.E. et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29, 522–528 (2015). https://doi.org/10.1007/s00464-014-3733-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3733-1