Abstract
Background
Laparoscopic surgery for gastrointestinal reflux disease was introduced in 1991. Early safety, efficacy, and 5–10-year durability have been amply documented, but long-term patient outcomes have been criticized. This study presents 20-year outcomes after laparoscopic fundoplication (LF) in a consecutive patient cohort.
Methods
Patients who underwent primary LF procedures for gastroesophageal reflux disease (GERD) were identified from a prospectively collected IRB-approved database (1991–1995). A phone symptom questionnaire was administered using a 5-point validated GERD scoring system (heartburn, regurgitation, and dysphagia). Symptomatic success was defined by a lack of surgical re-intervention and a low symptom score.
Results
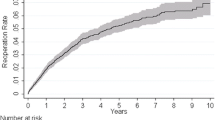
One-hundred and ninety-three patients were identified during the time period. Fifty-one patients completed the survey (100 lost to follow-up, 40 deceased, 2 declined to answer). Respondents had a median follow-up of 19.7 years. Overall, 38/51 (74.5 %) of patients reported complete control of heartburn and regurgitation. Ten patients reported only occasional heartburn. Eight of fifty-one (16 %) reported daily dysphagia, and 22/51 (43 %) of respondents were using proton pump inhibitors at the time of telephone interview. Nine of fifty-one (18 %) underwent revision of the original surgery which did not negatively impact the satisfaction rating, with 8/9 (89 %) of these patients reporting the highest satisfaction rating. Overall, 46/51 (90 %) were satisfied with their choice of surgery.
Conclusion
Long-term results from the early experience with LF are excellent with 94 % of patients reporting only occasional or fewer reflux symptoms at 20-year follow-up. However, 18 % required surgical revision surgery to maintain their results. There is a relatively high rate of daily dysphagia but 90 % of patients are happy to have had LF.





Similar content being viewed by others
References
Finks JF, Wei Y, Birkmeyer JD (2006) The rise and fall of antireflux surgery in the United States. Surg Endosc 20:1698–1701
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439
Richter JE, Dempsey DT (2008) Laparoscopic antireflux surgery: key to success in the community setting. Am J Gastroenterol 103:289–291
Richter JE (2003) Let the patient beware: the evolving truth about laparoscopic antireflux surgery. Am J Med 114:71–73
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg 204:9–20
Luostarinen M (1993) Nissen fundoplication for reflux esophagitis: long-term clinical and endoscopic results in 109 of 127 consecutive patients. Ann Surg 217:329–337
Dellemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, Jehaes C (2006) Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 20:159–165
Morgenthal CB, Shane MD, Stival A, Gletsu N, Milam G, Swafford V, Hunter JG, Smith CD (2007) The durability of laparoscopic Nissen fundoplication: 11-year outcomes. J Gastrointest Surg. doi:10.1007/s11605-007-0161-8
Hunter J, Swanstrom L, Waring JP (1996) Dysphagia after laparoscopic antireflux surgery. Ann Surg 224:51–57
Kelly JJ, Watson DI, Chin KF, Devitt PG, Game PA, Jamieson GG (2007) Laparoscopic Nissen fundoplication: clinical outcomes at 10 years. J Am Coll Surg 205:570–575
Khajanchee YS, O’Rourke R, Cassera MA, Gatta P, Hansen PD, Swanstrom LL (2007) Laparoscopic reintervention for failed antireflux surgery. Arch Surg 142:785–792
Khajanchee YS, O’Rourke RW, Lockhart BA, Patterson EJ, Hansen PD, Swanstrom LL (2002) Postoperative symptoms and failure following antireflux surgery. Arch Surg 137:1008–1014
Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R (1991) Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc 1:138–143
Patterson EJ, Herron DM, Hansen PD, Ramzi N, Standage BA, Swanstrom LL (2000) Effect of an esophageal bougie on the incidence of dysphagia following Nissen fundoplication: a prospective blinded randomized trial. Arch Surg 135:1055–1062
Disclosures
Ben Robinson, Christy M. Dunst, Maria A. Cassera, Kevin M. Reavis, Ahmed Sharata, and Lee L. Swanstrom have no conflicts of interest or financial relationships to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robinson, B., Dunst, C.M., Cassera, M.A. et al. 20 years later: laparoscopic fundoplication durability. Surg Endosc 29, 2520–2524 (2015). https://doi.org/10.1007/s00464-014-4012-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-4012-x