Summary
Aim
The aim of this study was to assess the occurrence of polypharmacy and excessive polypharmacy in very old hospitalized patients based on their comorbidities.
Methods
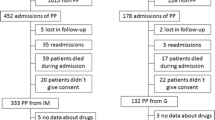
The documentation of patients aged 80 years or older admitted to our department in the year 2010 was analyzed. Based on the Charlson index of comorbidity, a multiple logistic regression model with stepwise backward elimination was performed. Patients were stratified by gender and four age-groups, and factors of a change in the number of medications during the hospital stay were assessed.
Results
Chronic pulmonary disease [odds ratio (OR): 2.40], diabetes mellitus with (OR: 4.65) or without (OR: 1.65) microvascular complications, congestive heart failure (OR: 2.37), connective tissue disease (OR: 3.02), and peripheral vascular disease (OR: 2.30) were statistically significantly associated with polypharmacy, while some of these diseases were also associated with excessive polypharmacy. The number of medications showed a gradual decrease with age, which was concordant with a decrease in total Charlson index score. “Admission for myocardial infarction” was associated with an increase in pharmaceuticals during hospital stay, whereas a known diagnosis of dementia or metastatic malignant disease was protective against a further increase in medications.
Conclusions
Several medical conditions seem to predispose to polypharmacy in very old patients. To attain old age seems to be associated with few comorbidities, which reduces the need for a high number of pharmaceuticals. Physicians should pay attention to the identified predictors in very old patients, as polypharmacy may lead to adverse events and unnecessary hospitalization.
Zusammenfassung
Ziel
Das Ziel dieser Studie war es, das Auftreten von Polypharmazie und exzessiver Polypharmazie in Abhängigkeit von Co-Morbiditäten bei hochbetagen hospitalisierten Patienten zu erfassen.
Methodik
Die Entlassungsdokumentationen von allen Patienten (80 Jahre oder älter), die 2010 im durchführenden Zentrum aufgenommen wurden, wurden analysiert. Basierend auf dem Charlson Co-Morbiditätsindex wurde ein multiples logistisches Regressionsmodell mit schrittweiser Rückwärtselimination durchgeführt. Die Patienten wurden des weiteren in 4 Altersgruppen und nach Geschlecht stratifiziert und die Änderung der Medikationen während des stationären Aufenthalts analysiert.
Ergebnisse
Chronische Lungenerkrankung (Odds ratio (OR) 2,40), Diabetes mellitus mit (OR 4,65) oder ohne (OR 1,65) mikrovaskulären Komplikationen, Herzinsuffizienz (OR 2,37), Kollagenose (OR 3,02) and periphere Gefäßerkrankung (OR 2,30) waren statistisch signifikant mit Polypharmazie assoziiert, während einige von diesen Erkrankungen auch mit exzessiver Polypharmazie zusammenhingen. Die Anzahl der eingenommenen Medikamente zeigte einen zunehmenden Abfall mit dem Alter, was mit einer gleichsinnigen Abnahme des Charlson Scores verbunden war. „Aufnahme wegen Myokardinfarkt“ war mit einer Zunahme an einzunehmenden Medikamenten verbunden, während Demenz oder ein metastasiertes Malignom einen protektiven Effekt auf eine Zunahme der Medikamente während des stationären Aufenthaltes hatte.
Schlussfolgerungen
Verschiedene Begleiterkrankungen begünstigen bei sehr betagten Patienten das Auftreten von Polypharmazie. Wenige Co-Morbitidäten scheinen eine Voraussetzung zu sein, um sehr hohes Alter zu erreichen, woraus reduzierter Medikamentenverbrauch resultiert.
Behandelnde Ärzte sollten besonders bei den identifizierten Risikopatienten auf Polypharmazie achten, da dies zu unerwünschtes Ereignissen und unnötiger Hospitalisierung führen kann.
Similar content being viewed by others
References
Linjakumpu T, Hartikainen S, Klaukka T, et al. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002 Aug;55(8):809–17.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51.
Tinetti ME, Bogardus ST, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351(27):2870–4.
Zulman DM, Sussman JB, Chen X, et al. Examining the evidence: a systematic review of the inclusion and analysis of older adults in randomized controlled trials. J Gen Intern Med. 2011 Jul;26(7):783–90.
Cherubini A, Oristrell J, Pla X, et al. The persistent exclusion of older patients from ongoing clinical trials regarding heart failure. Arch Intern Med. 2011 Mar 28;171(6):550–6.
Grabowski DC, Ellis JE. High body mass index does not predict mortality in older people: analysis of the Longitudinal Study of Aging. J Am Geriatr Soc. 2001;49:968–79.
Oreopoulos A, Padwal R, Kalantar-Zadeh K, et al. Body mass index and mortality in heart failure: a meta-analysis. Am Heart J. 2008;156:1322.
Gussekloo J, van Exel E, de Craen AJ, et al. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004 Dec 1;292(21):2591–9.
Rosholm JU, Christensen K. Relationship between drug use and self-reported health in elderly Danes. Eur J Clin Pharmacol. 1997;53:179–83.
Haider SI, Johnell K, Thorslund M, et al. Analysis of the association between polypharmacy and socioeconomic position among elderly aged > or = 77 years in Sweden. Clin Ther. 2008;30:419–27.
Junius-Walker U, Theile G, Hummers-Pradier E. Prevalence and predictors of polypharmacy among older primary care patients in Germany. Fam Pract. 2007;24:14–9.
Bjerrum L, Søgaard J, Hallas J, et al. Polypharmacy: correlations with sex, age and drug regimen. A prescription database study. Eur J Clin Pharmacol. 1998;54:197–202.
Mansur N, Weiss A, Hoffman A, et al. Continuity and adherence to long-term drug treatment by geriatric patients after hospital discharge: a prospective cohort study. Drugs Aging. 2008;25:861–70.
Barat I, Andreasen F, Damsgaard EM. Drug therapy in the elderly: what doctors believe and patients actually do. Br J Clin Pharmacol. 2001;51:615–22.
Thiruchselvam T, Naglie G, Moineddin R, et al. Risk factors for medication nonadherence in older adults with cognitive impairment who live alone. Int J Geriatr Psychiatry. 2012 Dec;27(12):1275–82.
Marcum ZA, Amuan ME, Hanlon JT, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60;34–41.
Ziere G, Dieleman JP, Hofman A, et al. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006;61:218–23.
Kuijpers MA, van Marum RJ, Egberts AC, et al. OLDY (OLd people Drugs & dYsregulations) Study Group. Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008;65:130–3.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Jensen GL, Friedmann JM, Coleman CD, et al. Screening for hospitalization and nutritional risks among community-dwelling older persons. Am J Clin Nutr. 2001;74:201–5.
Veehof LJ, Stewart RE, Meyboom-de Jong B, et al. Adverse drug reactions and polypharmacy in the elderly in general practice. Eur J Clin Pharmacol. 1999;55:533–6.
Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507–19.
Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012 Sep;65(9):989–95.
Mizokami F, Koide Y, Noro T, et al. Polypharmacy with common diseases in hospitalized elderly patients. Am J Geriatr Pharmacother. 2012;10:123–8.
Jyrkkä J, Enlund H, Korhonen MJ, et al. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75 + study: a cross-sectional analysis. Drugs Aging. 2009;26:493–503.
Barat I, Andreasen F, Damsgaard EM. The consumption of drugs by 75-year-old individuals living in their own homes. Eur J Clin Pharmacol. 2000;56:501–9.
Onder G, Liperoti R, Fialova D, et al. Polypharmacy in nursing home in Europe: results from the SHELTER study. J Gerontol A Biol Sci Med Sci. 2012;67:698–704.
Eggen AE. Pattern of drug use in a general population—prevalence and predicting factors: the Tromsø study. Int J Epidemiol. 1994;23:1262–72.
Corsonello A, Antonelli Incalzi R, Pistelli R, et al. Comorbidities of chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2011;17 Suppl 1:21–8.
Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362(9386):777–81.
Massie BM, Carson PE, McMurray JJ, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456–67.
McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–847.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent was not applicable, as this was a retrospective analysis. The protocol for data acquisition and analysis was approved by the Viennese ethics committee (“Ethikkommission der Stadt Wien,” approval number: EK-12-219-VK).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strehblow, C., Smeikal, M. & Fasching, P. Polypharmacy and excessive polypharmacy in octogenarians and older acutely hospitalized patients. Wien Klin Wochenschr 126, 195–200 (2014). https://doi.org/10.1007/s00508-013-0485-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-013-0485-1