Abstract
Background
The oxaliplatin-based regimen FOLFOX is widely used to treat patients with advanced colorectal cancer (CRC). However, dose-limiting toxicity after continuous oxaliplatin administration can lead to peripheral neuropathy. Several agents, including opioids, that have been employed to treat oxaliplatin-induced peripheral neuropathy (OIPN) have been examined in clinical settings regarding their protective and therapeutic effects. However, the pharmacotherapy of these agents has not yet been established. Therefore, we investigated the efficacy and tolerability of oxycodone for OIPN and subsequently with FOLFOX therapy in CRC patients.
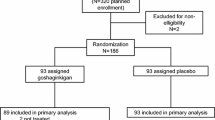
Methods
This was a single-center retrospective study of 64 CRC patients who underwent FOLFOX therapy at the Toho University Sakura Medical Center (Sakura, Japan). Controlled-release (CR) oxycodone was concomitantly administered to 29 patients (OXY group), whereas the additional 35 patients (non-OXY group) were not given oxycodone during the FOLFOX treatment course. The incidence and severity of OIPN and the number of FOLFOX cycles were measured and compared between the two groups. Neurological toxicities were assessed according to the Common Terminology Criteria for Advanced Events, version 3.0.
Results
All study patients had OIPN. Most patients experienced grade 1 or 2 sensory neuropathy. Grade 3 sensory neuropathy was observed in two patients in the non-OXY group. All patients in the OXY group completed the scheduled FOLFOX therapy, whereas FOLFOX therapy was discontinued in ten patients in the non-OXY group due to severe peripheral neuropathy. The median numbers of FOLFOX cycles in the OXY and non-OXY groups were 13 (range, 6–46) and 7 (range, 2–18), respectively (P < 0.05). The median cumulative oxaliplatin doses were 1072.3 mg/m2 (range, 408.7–3385.3 mg/m2) in the OXY group and 483.0 mg/m2 (range 76.2–1414.1 mg/m2) in the non-OXY group (P < 0.05).
Conclusions
Our findings indicate that CR oxycodone might attenuate the severity of OIPN and extend the use of FOLFOX therapy.
Similar content being viewed by others
Introduction
The occurrence of cancer therapy-related chronic pain has become more frequent over the past few decades. This is because cancer treatments such as surgery, chemotherapy, hormonal therapy, and radiotherapy, among others, when used individually and in combination, have potential side effects that can lead to severe and persistent pain [1]. Chemotherapy-induced peripheral neuropathy (CIPN), for example, has become more prevalent as increased numbers of neurotoxic agents have been introduced as treatment for different types of cancer [2]. Dose reduction or discontinuation of these chemotherapeutic agents might limit any potential curative effects and ultimately reduce the chance of survival. Therefore, CIPN is a common complication associated with several classes of chemotherapeutic agents. These agents include platinum-based compounds (cisplatin, carboplatin, and oxaliplatin), taxanes (paclitaxel and docetaxel), and vinca alkaloids (vincristine and vinblastine). The symptoms of CIPN mostly depend on the involved nerves. The most common symptoms are numbness, pain (shooting, stabbing, burning, tingling, or electric/shock-like pain), loss of feeling, impaired manual dexterity, balance problems, and decreased or absent reflexes [3–5]. These symptoms can seriously impair the patient’s quality of life (QoL) and are thus important to address.
Colorectal cancer (CRC) is among the leading causes of cancer-related mortality, and its prevalence has increased in Japan. Oxaliplatin is a third-generation platinum-based cytotoxic agent that is used in the oxaliplatin-based regimen FOLFOX, a standard chemotherapeutic protocol for the treatment of advanced CRC patients with metastasis and in adjuvant settings [6]. The safety profile of oxaliplatin, for which renal or hematologic toxicity is uncommon, is somewhat different from that of conventional platinum-based compounds [4, 7–9], as the principal and dose-limiting cumulative toxicity associated with oxaliplatin-based chemotherapy is neurotoxicity [10].
Two distinct forms of oxaliplatin-induced neuropathy have been described in the literature. The first is a unique acute, transient peripheral nerve hyperexcitability syndrome that occurs shortly after the infusion of oxaliplatin. This form of neuropathy usually occurs with low total cumulative doses and can be triggered or exacerbated by exposure to cold stimuli. Patients might experience paresthesia and dysesthesia of the hands and feet, as well as of the larynx and jaw. These symptoms tend to occur within hours of exposure and are reversible over time, especially over the next few hours and days. The symptoms do not generally lead to discontinuation of oxaliplatin-based chemotherapy [10]. Second, a chronic peripheral sensory neuropathy occurs mainly in distal extremities and presents with symptoms similar to those of cisplatin-induced neuropathy. The development of chronic neuropathy is reported to correlate with the cumulative oxaliplatin dose. Indeed, a loss of sensation, dysesthesia, and even functional impairment can develop progressively after several cycles of oxaliplatin-based therapy. These effects are reversible, but might last for several months and have had a significant impact on the continuation of oxaliplatin-based treatment [11], as these painful symptoms often disrupt the chemotherapy schedule. Furthermore, patients who are unable to complete a planned therapy program might suffer from chronic discomfort and a decreased QoL [12–15].
CIPN-related pain is predominantly neuropathic, and controlled-release (CR) oxycodone was found to be efficacious and tolerable for the treatment of neuropathic pain in several clinical settings. A meta-analysis of the role of opioids in the treatment of benign neuropathic pain showed that opioids, particularly oxycodone, were more effective than other agents [16, 17]. A randomized phase II trial showed that the combination of oxycodone and pregabalin was effective and safe for the treatment of neuropathic pain in cancer patients [18].
The objective of this study was to evaluate the efficacy and tolerability of oxycodone in oxaliplatin-induced peripheral neuropathy (OIPN) and its impact on FOLFOX therapy in cancer patients.
Patients and methods
Patients
We retrospectively reviewed the medical records of patients with histologically confirmed CRC between November 2006 and February 2012 at the Toho University Sakura Medical Center (Sakura, Japan). Among the reviewed patients, a total of 64 advanced CRC patients with stage III or IV disease were included in this study. All eligible patients underwent gross resection of the primary CRC (microscopic residual disease or residual marginal involvement was allowed) and subsequently received curative-intent oxaliplatin-based FOLFOX therapy. The key inclusion criteria were as follows: ≥18 years of age, a World Health Organization (WHO) performance status score of 0 or 1, and a life expectancy of ≥6 months. Patients with preexisting peripheral neuropathy or those who were previously exposed to other neurotoxic chemotherapeutic agents were excluded from the study.
All patients received modified FOLFOX6 (mFOLFOX6) therapy. mFOLFOX6 comprises a bolus of 85 mg/m2 oxaliplatin, 250 mg/m2 leucovorin, and 400 mg/m2 5-fluorouracil (5-FU), followed by a 48-h continuous infusion of 5-FU at 2500 mg/m2, given every 2 weeks. Bevacizumab, cetuximab, or panitumumab was administered prior to mFOLFOX6 in 27 cases. On a case-by-case basis, the physician in charge determined whether dose reduction or treatment interruption was appropriate in the instance of a severe toxicity response. Oxaliplatin-based FOLFOX chemotherapy was continued until disease progression (PD), the decision to use alternative therapies, unacceptable toxicities, or patient refusal of further treatment.
Study design
Patients were divided into two groups. Patients with cancer-related pain who had been administered CR oxycodone during the FOLFOX therapy period were defined as the OXY group. Patients who did not receive CR oxycodone treatment were defined as the non-OXY group. The OXY and non-OXY groups included 29 and 35 patients, respectively. No opioids besides CR oxycodone were administered to the study population before and during FOLFOX therapy. Regarding other analgesics, clonazepam was administered to six patients in the OXY group and two patients in the non-OXY group, and gabapentin was administered to one patient in the non-OXY group. Neurological toxicities were assessed according to the Common Terminology Criteria for Advanced Events (CTCAE) version 3.0 (U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute). The severity of neurological toxicity was evaluated as the worst score in each patient during FOLFOX therapy. A peripheral sensory neuropathy subscale was applied to grade the clinical severity as follows: grade 1, asymptomatic or with a loss of deep tendon reflex or paresthesia (including tingling) that did not interfere with function; grade 2, sensory alterations or paresthesia (including tingling) that interfered with function, but not with activities of daily living (ADL); and grade 3, sensory alterations or paresthesia that interfered with ADL [19]. Pain intensity was also measured on a numeric rating scale after each cycle of FOLFOX therapy. In this study, we focused on oxaliplatin-induced chronic cumulative neuropathy because this type of neuropathy might result in severe neurologic function disturbances and significantly impact the continuation of oxaliplatin treatment.
Statistical analysis
The study was designed to determine differences between patients in the OXY and non-OXY groups, undergoing oxaliplatin-based FOLFOX therapy. For both treatment groups, the medians and relative frequencies were compared using Welch’s t-test for two independent samples and the Wilcoxon signed-rank test and Fisher’s exact test, respectively. Statistical significance was determined as P < 0.05.
Results
Baseline characteristics of the eligible patients (Table 1)
The demographic and clinicopathological data collected from the medical records of 64 patients are shown in Table 1. The OXY group included 29 patients, and CR oxycodone was administered to five patients with cancer-related pain before starting FOLFOX therapy. The daily CR oxycodone doses at baseline ranged from 10 to 40 mg. Other patients in the OXY group received CR oxycodone after the occurrence of painful peripheral neuropathy. The OXY and non-OXY groups did not significantly differ in age (P = 0.2582; Welch’s t-test) or gender (P = 1.0000; Fisher’s exact test). The maximum daily CR oxycodone doses were as follows: 160 mg for one patient (3.4 %), 40 mg for two patients (6.9 %), 30 mg for three patients (10.3 %), 20 mg for three patients (10.3 %), 15 mg for two patients (6.9 %), and 10 mg for 18 patients (62.1 %).
CTCAE grading of sensory neuropathy during the study period (Table 2)
As shown in Table 2, all patients (100 %) in the OXY group and 33 patients (94.3 %) in the non-OXY group experienced grade 1 or 2 sensory neuropathy. Grade 3 neurotoxicity was not observed in the OXY group, whereas two patients (5.7 %) in the non-OXY group reported grade 3 sensory neuropathy. Although 14 patients (40 %) in the non-OXY group reported mild pain, these patients did not receive opioid therapy. In contrast, every patient in the OXY group who experienced more than mild pain received CR oxycodone. In the OXY group, pain was generally well controlled by adequate dose titration. Two months after the completion of FOLFOX therapy, the sensory neuropathy worsened from grade 1 to 2 in 1 non-OXY group patient, whereas the sensory neuropathy grades remained stable or improved in the other group patients. In the OXY group, the sensory neuropathy grades improved in every patient. CR oxycodone was discontinued in ten patients (34.5 %) in the OXY group after the completion of FOLFOX therapy.
Causes of FOLFOX therapy discontinuation (Table 3)
FOLFOX therapy was interrupted in some cases. The causes of interruption are listed in Table 3. There were no discontinuations due to peripheral neuropathy in the OXY group. However, for ten patients (28.6 %) in non-OXY group, FOLFOX therapy was terminated because of severe OIPN. Eighteen patients (62.1 %) in the OXY group discontinued FOLFOX therapy because of PD, compared with seven patients (20 %) in the non-OXY group. Other reasons for interrupting FOLFOX therapy were unacceptable toxicities besides peripheral sensory neuropathy, scheduled switching to alternative therapies, or patient refusal of further treatment.
Frequencies of FOLFOX cycles and total oxaliplatin doses (Table 4)
We also compared the number of FOLFOX cycles in the OXY and non-OXY groups. Patients in the OXY group received a median of 13 cycles of FOLFOX therapy (range, 6–46 cycles). Patients in the non-OXY group received a median of seven cycles (range, 2–18 cycles). The number of FOLFOX cycles in the OXY group significantly exceeded that in the non-OXY group (P < 0.05; Welch’s t-test). The median total oxaliplatin doses were 1072.3 mg/m2 (range, 408.7–3385.3 mg/m2) in the OXY group and 483.0 mg/m2 (range, 76.2–1414.1 mg/m2) in the non-OXY group. The total administered oxaliplatin dose was also significantly higher in the OXY group than in the non-OXY group (P < 0.05; Welch’s t-test; Table 4).
There were no statistically significant differences between the five patients who were administered CR oxycodone before FOLFOX therapy and the other 24 patients in the OXY group with regard to the number of FOLFOX cycles (P = 0.6094; Welch’s t-test) and the total oxaliplatin dose (P = 0.5424; Welch’s t-test; data not shown). There were also no statistically significant differences between the OXY group patients who did or did not receive other analgesics with regard to the number of FOLFOX cycles (P = 0.2503; Welch’s t-test) and the total oxaliplatin dose (P = 0.3186; Welch’s t-test; data not shown).
A total of 15 possible opioid-induced adverse events occurred in ten patients in the OXY group during the FOLFOX therapy period. Constipation was the most common event and occurred in eight patients (27.6 %). Other adverse events included drowsiness (6.7 %), nausea (6.7 %), hallucination (3.4 %), and anorexia (3.4 %). The severity of each adverse event was classified as grade 1, and CR oxycodone was not discontinued in any case because of adverse events.
Discussion
CIPN treatment remains a challenge for clinicians. A number of protective and treatment approaches that focused on CIPN were investigated in clinical trials. However, evidence for pharmacological therapeutic strategies has not been fully established, and further investigation is required.
Regarding the management of OIPN, current recommendations include patient education, dose modification, the “stop and go” approach, and the use of neuromodulatory agents, particularly intravenous calcium and magnesium (Ca/Mg) infusion. Ca/Mg infusion was widely examined, and a meta-analysis that included four prospective randomized clinical trials and three retrospective clinical trials suggested that Ca/Mg infusion might decrease the incidence of OIPN without reducing chemotherapeutic efficacy [20]. However, Loprinzi et al. revealed that Ca/Mg infusion did not reduce cumulative OIPN in a recent randomized, placebo-controlled, double-blind trial [21]. A recent randomized pilot clinical trial also failed to demonstrate a protective effect of vitamin E on acute OIPN [22]. Several antiepileptic and antidepressant agents, including amitriptyline, gabapentin, and lamotrigine, did not show significant efficacy in this setting [23–25]. Among the serotonin and norepinephrine reuptake inhibitors, venlafaxine exhibited a therapeutic effect on painful OIPN [26]. In addition, duloxetine significantly reduced CIPN-associated pain intensity in a recent randomized placebo-controlled crossover trial, suggesting the clinical efficacy of duloxetine for OIPN [27].
The efficacy and tolerability of opioids for CIPN has rarely been investigated. However, despite their differing etiologies, agents used to treat peripheral neuropathic pain might have the potential to exhibit demonstrable efficacies for CIPN [28]. Given their proven clinical efficacies in treating peripheral neuropathic pain, opioids might be effective for the treatment of painful CIPN. In particular, oxycodone provided significant pain relief from peripheral neuropathic pain caused by post-herpetic neuralgia or diabetic neuropathy [29–32]. CR oxycodone was also shown to be effective for bortezomib-induced peripheral neuropathic pain in multiple myeloma patients [33]. Furthermore, recent basic studies have demonstrated that the antinociceptive effect of oxycodone was superior to that of morphine in a neuropathic pain mouse model [34] and that the analgesic profile of oxycodone in a bone cancer pain mouse model with a neuropathic pain-like state was different from those of morphine and fentanyl [35]. Although the pharmacological mechanism of oxycodone against peripheral neuropathic pain remains unclear, the results of those clinical trials and basic studies suggest that oxycodone could be considered a therapeutic option for CIPN.
We retrospectively investigated the efficacy and tolerability of CR oxycodone for OIPN during FOLFOX therapy in CRC patients. A total of 62.1 % of patients in the OXY group continued FOLFOX therapy until PD. Conversely, only 20 % of patients in the non-OXY group continued FOLFOX therapy until PD. The cumulative oxaliplatin dose was significantly higher in the OXY group than in the non-OXY group. Because patients in the OXY group received a higher cumulative dose of oxaliplatin, they would be expected to present with substantially more severe OIPN than patients in the non-OXY group; however, grade 3 sensory neuropathy only occurred in the non-OXY group. These results suggest that CR oxycodone might prevent or improve the symptoms of OIPN in CRC patients.
This study has several limitations. First, the sample size was small and the study design was observational and retrospective. Second, the severity of OIPN was measured according to the CTCAE grading system. The reliability of the CTCAE scale is controversial, and a recent study revealed that CTCAE scale overestimated the occurrence of motor neuropathy [36]. Finally, the pain intensity in 23 patients (79.3 %) in the OXY group remained mild during the study period, and thus, it was difficult to evaluate the analgesic effects of CR oxycodone on OIPN. Therefore, the continuation of oxaliplatin administration was worth evaluating to confirm the therapeutic efficacy and tolerability of CR oxycodone in patients with OIPN.
Conclusion
In conclusion, we demonstrated that patients who were administered CR oxycodone received significantly more cycles of FOLFOX therapy and a higher cumulative oxaliplatin dose than did patients who were not administered CR oxycodone. Although this study had several limitations, the results suggest that CR oxycodone can attenuate OIPN and extend FOLFOX therapy in CRC patients.
References
Paice JA (2010) Chronic treatment-related pain in cancer survivors. Pain 152(3 suppl):S84–S89
Malik B, Stillman M (2008) Chemotherapy-induced peripheral neuropathy. Curr Pain Headache Rep 12:165–174
Loprinzi CL, Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, Kamal A, Le-Lindqwister NA, Soori GS, Jaslowski AJ, Novotny PJ, Lachance DH (2011) Natural history of paclitaxel-associated acute pain syndrome: prospective cohort study NCCTG N08C1. J Clin Oncol 29:1472–1478
McWhinney SR, Goldberg RM, McLeod HL (2009) Platinum neurotoxicity pharmacogenetics. Mol Cancer Ther 8:10–16
Quasthoff S, Hartung HP (2002) Chemotherapy-induced peripheral neuropathy. J Neurol 249:9–17
André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan P, Bridgewater J, Tabah-Fisch I, de Gramont A (2004) Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350:2343–2351
Kottschade LA, Sloan JA, Mazurczak MA, Johnson DB, Murphy BP, Rowland KM, Smith DA, Berg AR, Stella PJ, Loprinzi CL (2011) The use of vitamin E for the prevention of chemotherapy-induced peripheral neuropathy: results of a randomized phase III clinical trial. Support Care Cancer 19:1769–1777
Meyer L, Patte-Mensah C, Taleb O, Mensah-Nyagan AG (2011) Allopregnanolone prevents and suppresses oxaliplatin-evoked painful neuropathy: multi-parametric assessment and direct evidence. Pain 152:170–181
Garg MB, Ackland SP (2011) Pyridoxine to protect from oxaliplatin-induced neurotoxicity without compromising antitumor effect. Cancer Chemother Pharmacol 67:963–966
Wilson RH, Lehky T, Thomas RR (2002) Acute oxaliplatin-induced peripheral nerve hyperexcitability. J Clin Oncol 20:1767–1774
Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC (2011) Dose effects of oxaliplatin on persistent and transient Na+ conductances and the development of neurotoxicity. PLoS One 6:e18469
Mols F, Beijers T, Lemmens V, van den Hurk CJ, Vreugdenhil G, van de Poll-Franse LV, Saif MW, Reardon J (2013) Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 31:2699–2707
Tofthagen C, Donovan KA, Morgan MA, Shibata D, Yeh Y (2013) Oxaliplatin-induced peripheral neuropathy’s effects on health-related quality of life of colorectal cancer survivors. Support Care Cancer 21:3307–3313
Shimozuma K, Ohashi Y, Takeuchi A, Aranishi T, Morita S, Kuroi K, Ohsumi S, Makino H, Katsumata N, Kuranami M, Suemasu K, Watanabe T, Hausheer FH (2012) Taxane-induced peripheral neuropathy and health-related quality of life in postoperative breast cancer patients undergoing adjuvant chemotherapy: N-SAS BC02 A randomized clinical trial. Support Care Cancer 20:3355–3364
Tofthagen C (2010) Surviving chemotherapy for colon cancer and living with the consequences. J Palliat Med 13:1389–1391
Eisenberg E, McNicol ED, Carr DB (2005) Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin: systematic review and meta-analysis of randomized controlled trials. JAMA 293:3043–3052
Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E (2006) Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ 174:1589–1594
Garassino MC, Piva S, La Verde N, Spagnoletti I, Iorno V, Carbone C, Febbraro A, Bianchi A, Bramati A, Moretti A, Ganzinelli M, Marabese M, Gentili M, Torri V, Farina G (2013) Randomised phase II trial (NCT00637975) evaluating activity and toxicity of two different escalating strategies for pregabalin and oxycodone combination therapy for neuropathic pain in cancer patients. PLoS One 8:e59981
U.S. Department of Health and Human Services (2009) Common terminology criteria of adverse events (CTCAE) version 3.0
Wen F, Zhou Y, Wang W, Hu QC, Liu YT, Zhang PF, Du ZD, Dai J, Li Q (2013) Ca/Mg infusions for the prevention of oxaliplatin-related neurotoxicity in patients with colorectal cancer : a meta-analysis. Ann Oncol 24:171–178
Loprinzi L, Qin R, Dakhil SR, Fehrenbacher K, Stella PJ, Atherton PJ, Seisler DK, Qamar R, Lewis GC, Grothey A (2013) Phase III randomized, placebo (PL)-controlled, double-blind study of intravenous calcium/magnesium (CaMg) to prevent oxaliplatin-induced sensory neurotoxicity (sNT), N08CB : an alliance for clinical trials in oncology study. J Clin Oncol 31(15 suppl):3501
de Afonseca SO, Cruz FM, de Iracema Gomes Cubero D, Lera AT, Schindler F, Okawara M, de Souza LF, Rogrigues NP, del Giglio A (2013) Vitamin E for prevention of oxaliplatin-induced peripheral neuropathy : a pilot randomized clinical trial. Sao Paulo Med J 131:35–38
Kautio A-L, Haanpaa M, Leminen A, Kalso E, Kautiainen H, Saarto T (2009) Amitriptyline in the prevention of chemotherapy-induced neuropathic symptoms. Anticancer Res 29:2601–2606
Rao RD, Michalak JC, Sloan JA, Loprinzi CL, Soori GS, Nickcevich DA, Warner DO, Novotny P, Kutteh LA, Wong GY, the North Central Cancer Treatment Group (2007) Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy : A phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer 110:2110–2118
Rao RD, Flynn PJ, Sloan JA, Wong GY, Novotny P, Johnson DB, Gross HM, Nashawaty M, Loprinzi CL (2008) Efficacy of lamotrigine in the management of chemotherapy-induced peripheral neuropathy : A phase 3 randomized, double-blind, placebo-controlled trial, N01C3. Cancer 112:2802–2808
Durand JP, Deplanque G, Montheil V, Gornet JM, Scotte F, Mir O, Cessot A, Coriat R, Raymond E, Mitry E, Herait P, Yataghene Y, Goldwasser F (2012) Efficacy of venlafaxine for the prevention and relief of oxaliplatin-induced acute neurotoxicity : results of EFFOX, a randomized, double-blind, placebo-controlled phase III trial. Ann Oncol 23:200–205
Smith EM, Pang H, Cirrincione C, Fleishman S, Paskett ED, Ahles T, Bressler LR, Fadul CE, Knox C, Le-Lindqwister N, Gilman PB, Shapiro CL (2013) Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA 309:1359–1367
Urch CE, Dickenson AH (2008) Neuropathic pain in cancer. Eur J Pain 44:1091–1096
Watson CPN, Babul N (1998) Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia. Neurology 50:1837–1841
Watson CP, Moulin D, Watt-Watson J, Gordon A, Eisenhoffer J (2003) Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain 105:71–78
Gimbel JS, Rochards P, Portenoy RK (2003) Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology 60:927–934
Hanna M, O’Brien C, Wilson MC (2008) Prolonged-release oxycodone enhances the effects of existing gabapentin therapy in painful diabetic neuropathy patients. Eur J Pain 12:804–813
Cartoni C, Brunetti GA, Federico V, Efficace F, Grammatico S, Tendas A, Scaramucci L, Cupelli L, D’Elia GM, Truini A, Niscola P, Petrucci MT (2012) Controlled-release oxycodone for the treatment of bortezomib-induced neuropathic pain in patients with multiple myeloma? Support Care Cancer 20:2621–2626
Narita M, Nakamura A, Ozaki M, Imai S, Miyoshi K, Suzuki M, Suzuki T (2008) Comparative pharmacological profiles of morphine and oxycodone under a neuropathic pain-like state in mice: evidence for less sensitivity to morphine. Neuropsychopharmacology 33:1097–1112
Minami K, Hasegawa M, Ito H, Nakamura A, Tomii T, Matsumoto M, Orita S, Matsushima S, Miyoshi T, Masuno K, Torii M, Koike K, Shimada S, Kanemasa T, Kihara T, Narita M, Suzuki T, Kato A (2009) Morphine, oxycodone, and fentanyl exhibit different analgesic profiles in mouse pain models. J Pharmacol Sci 111:60–72
Frigeni B, Piatti M, Lanzani F, Alberti P, Villa P, Zanna C, Ceracchi M, Ildebrando M, Cavaaletti G (2011) Chemotherapy-induced peripheral neurotoxicity can be misdiagnosed by the National Cancer Institute Common Toxicity scale. J Peripher Nerv Syst 16:228–236
Acknowledgments
This work was supported by Grants-in-Aid from the Smoking Research Foundation.
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Nagashima, M., Ooshiro, M., Moriyama, A. et al. Efficacy and tolerability of controlled-release oxycodone for oxaliplatin-induced peripheral neuropathy and the extension of FOLFOX therapy in advanced colorectal cancer patients. Support Care Cancer 22, 1579–1584 (2014). https://doi.org/10.1007/s00520-014-2132-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2132-4