Abstract
Purpose
We examined whether multi-disciplinary stepped psycho-social care decreases financial problems and improves return-to-work in cancer patients.
Methods
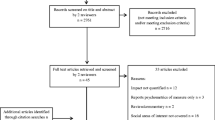
In a university hospital, wards were randomly allocated to either stepped or standard care. Stepped care comprised screening for financial problems, consultation between doctor and patient, and the provision of social service. Outcomes were financial problems at the time of discharge and return-to-work in patients < 65 years old half a year after baseline. The analysis employed mixed-effect multivariate regression modeling.
Results
Thirteen wards were randomized and 1012 patients participated (n = 570 in stepped care and n = 442 in standard care). Those who reported financial problems at baseline were less likely to have financial problems at discharge when they had received stepped care (odds ratio (OR) 0.2, 95% confidence interval (CI) 0.1, 0.7; p = 0.01). There was no evidence for an effect of stepped care on financial problems in patients without such problems at baseline (OR 1.1, CI 0.5, 2.6; p = 0.82). There were 399 patients < 65 years old who were not retired at baseline. In this group, there was no evidence for an effect of stepped care on being employed half a year after baseline (OR 0.7, CI 0.3, 2.0; p = 0.52).
Trial registration
NCT01859429
Conclusions
Financial problems can be avoided more effectively with multi-disciplinary stepped psycho-social care than with standard care in patients who have such problems.

Similar content being viewed by others
References
Ernst J, Mehnert A, Weis J, Faust T, Giesler JM, Roick J (2016) Social counseling in outpatient cancer counseling centers offers and usage by advice-seekers. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 59(11):1476–1483. https://doi.org/10.1007/s00103-016-2440-6
Miller JJ, Frost MH, Rurnmans TA, Huschka M, Atherton P, Brown P, Gamble G, Richardson J, Hanson J, Sloan JA, Clark MM (2007) Role of a medical social worker in improving quality of life for patients with advanced cancer with a structured multidisciplinary intervention. J Psychosoc Oncol 25(4):105–119. https://doi.org/10.1300/J077v25n04_07
Pockett R, Dzidowska M, Hobbs K (2015) Social work intervention research with adult cancer patients: a literature review and reflection on knowledge-building for practice. Soc Work Health Care 54(7):582–614. https://doi.org/10.1080/00981389.2015.1046577
De Boer AGEM, Taskila TK, Tamminga SJ, Feuerstein M, Frings-Dresen MHW, Verbeek JH (2015) Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007569.pub3
Cwikel JG, Behar LC (1999) Organizing social work services with adult cancer patients: integrating empirical research. Soc Work Health Care 28(3):55–76. https://doi.org/10.1300/J010v28n03_04
Singer S, Hohlfeld S, Müller-Briel D, Dietz A, Brähler E, Schröter K, Lehmann-Laue A (2011) Psychosoziale Versorgung von Krebspatienten - Versorgungsdichte und -bedarf. Psychotherapeut 56(5):386–393. https://doi.org/10.1007/s00278-011-0859-7
Rottenberg Y, Jacobs JM, Ratzon NZ, Grinshpun A, Cohen M, Uziely B, De Boer AGEM (2017) Unemployment risk 2 years and 4 years following gastric cancer diagnosis: a population-based study. J Cancer Surviv 11(1):119–125. https://doi.org/10.1007/s11764-016-0568-x
Paalman CH, van Leeuwen FE, Aaronson NK, De Boer AGEM, van de Poll-Franse L, Oldenburg HSA, Schaapveld M (2016) Employment and social benefits up to 10 years after breast cancer diagnosis: a population-based study. Br J Cancer 114(1):81–87. https://doi.org/10.1038/bjc.2015.431
Azzani M, Roslani AC, TT S (2015) The perceived cancer-related financial hardship among patients and their families: a systematic review. Support Care Cancer 23(3):889–898. https://doi.org/10.1007/s00520-014-2474-y
Arozullah AM, Calhoun EA, Wolf M, Finley DK, Fitzner KA, Heckinger EA, Gorby NS, Schumock GT, Bennett CL (2004) The financial burden of cancer: estimates from a study of insured women with breast cancer. J Support Oncol 2(3):271–278
Longo CJ, Fitch M, Deber RB, Williams AP (2006) Financial and family burden associated with cancer treatment in Ontario, Canada. Support Care Cancer 14(11):1077–1085. https://doi.org/10.1007/s00520-006-0088-8
Schiel RO, Brechtel A, Hartmann M, Taubert A, Walther J, Wiskemann J, Rötzer I, Becker N, Jäger D, Herzog W, Friederich H-C (2014) Multidisziplinärer Versorgungsbedarf psychisch belasteter Tumorpatienten an einem Comprehensive Cancer Center. Dtsch Med Wochenschr 139(12):587–591. https://doi.org/10.1055/s-0034-1369856
Singer S, Danker H, Roick J, Einenkel J, Briest S, Spieker H, Dietz A, Hoffmann I, Papsdorf K, Meixensberger J, Mössner J, Schiefke F, Dietel A, Wirtz H, Niederwieser D, Berg T, Kersting A (2017) Effects of stepped psycho-oncological care combining distress screening and doctor consultation on referral to psychosocial services and emotional well-being: a cluster-randomised controlled trial. Psychooncology 26(10):1675–1683. https://doi.org/10.1002/pon.4492
Singer S, Götze H, Möbius C, Witzigmann H, Kortmann R-D, Lehmann A, Höckel M, Schwarz R, Hauss J (2009) Quality of care and emotional support from the inpatient cancer patient’s perspective. Langenbeck's Arch Surg 394(4):723–731. https://doi.org/10.1007/s00423-009-0489-5
Zimmermann-Schlegel V, Hartmann M, Sklenarova H, Herzog W, Haun MW (2017) Accessibility, availability, and potential benefits of psycho-oncology services: the perspective of community-based physicians providing cancer survivorship care. Oncologist 22(6):719–727. https://doi.org/10.1634/theoncologist.2016-0245
Dibbelt S, Schaidhammer M, Fleischer C, Greitemann B (2009) Patient-doctor interaction in rehabilitation: the relationship between perceived interaction quality and long-term treatment results. Patient Educ Couns 76(3):328–335. https://doi.org/10.1016/j.pec.2009.07.031
Fan SY, Lin IM, Hsieh JG, Chang CJ (2017) Psychosocial care provided by physicians and nurses in palliative care: a mixed methods study. J Pain Symptom Manag 53(2):216–223. https://doi.org/10.1016/j.jpainsymman.2016.08.019
Schumacher A (2017) Psycho-oncological care of patients with acute leukemia. Onkologe 23(7):550–554. https://doi.org/10.1007/s00761-017-0224-8
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, Dehaes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F (1993) The European organization for research and treatment of cancer QLQ-C30—a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
Singer S, Kuhnt S, Zwerenz R, Eckert K, Hofmeister D, Dietz A, Giesinger J, Hauss J, Papsdorf K, Briest S, Brown A (2011) Age- and sex-standardised prevalence rates of fatigue in a large hospital-based sample of cancer patients. Br J Cancer 105(3):445–451. https://doi.org/10.1038/bjc.2011.251
Schwarz R, Hinz A (2001) Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer 37(11):1345–1351. https://doi.org/10.1016/S0959-8049(00)00447-0
Mehnert A (2011) Employment and work-related issues in cancer survivors. Critical reviews in oncology. Hematology 77:109–130
Mehnert A, Koch U (2013) Predictors of employment among cancer survivors after medical rehabilitation—a prospective study. Scand J Work Environ Health 39(1):76–87. https://doi.org/10.5271/sjweh.3291
Carlsen K, Dalton SO, Frederiksen K, Diderichsen F, Johansen C (2008) Cancer and the risk for taking early retirement pension: a Danish cohort study. Scand J Public Health 36(2):117–125. https://doi.org/10.1177/1403494807085192
Damkjaer LH, Deltour I, Suppli N, Christensen J, Kroman N, Johansen C, Dalton SO (2011) Breast cancer and early retirement: associations with disease characteristics, treatment, comorbidity, social position and participation in a six-day rehabilitation course in a register-based study in Denmark. Acta Oncol 50:281
First M, Spitzer R, Gibbon M, Williams J (1997) Structured clinical interview for DSM-IV axis I disorders (SCID-I), Clinician Version. American Psychiatric Press, Washington
Roick J, Danker H, Kersting A, Briest A, Dietrich A, Dietz A, Einenkel J, Papsdorf K, Lordick F, Meixensberger J, Mössner J, Niederwieser D, Prietzel T, Schiefke F, Stolzenburg J-U, Wirtz H, Singer S (2017) Factors associated with non-participation and attrition of cancer patients in a cluster-randomised controlled trial testing a health care model in psycho-oncology. Eur J Cancer Care. https://doi.org/10.1111/ecc.12645
McLachlan SA, Allenby A, Matthews J, Wirth A, Kissane D, Bishop M, Beresford J, Zalcberg J (2001) Randomized trial of coordinated psychosocial interventions based on patient self-assessments versus standard care to improve the psychosocial functioning of patients with cancer. J Clin Oncol 19(21):4117–4125. https://doi.org/10.1200/JCO.2001.19.21.4117
Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R (2013) Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol 31(6):782–793. https://doi.org/10.1200/JCO.2011.40.8922
Zebrack B, Burg MA, Vaitones V (2012) Distress screening: an opportunity for enhancing quality cancer care and promoting the oncology social work profession. J Psychosoc Oncol 30(6):615–624. https://doi.org/10.1080/07347332.2012.721485
Kowalski C, Ferencz J, Singer S, Weis I, Wesselmann S (2017) Frequency of psycho-oncologic and social service counseling in cancer centers relative to center site and hospital characteristics: findings from 879 center sites in Germany, Austria, Switzerland, and Italy. Cancer 122:3538–3545
Cwikel JG, Behar LC (1999) Social work with adult cancer patients: a vote-count review of intervention research. Soc Work Health Care 29(2):39–67. https://doi.org/10.1300/J010v29n02_03
Velikova G, Coens C, Efficace F, Greimel E, Groenvold M, Johnson C, Singer S, van de Poll-Franse L, Young T, Bottomley A, on behalf of the EORTC Quality of Life Group (2012) Health-related quality of life in EORTC clinical trials—30 years of progress from methodological developments to making a real impact on oncology practice. Eur J Cancer Suppl 10(1):141–149. https://doi.org/10.1016/S1359-6349(12)70023-X
Torp S, Gudbergsson SB, Dahl AA, Fossa SD, Flotten T (2011) Social support at work and work changes among cancer survivors in Norway. Scand J Public Health 39(6_suppl):33–42. https://doi.org/10.1177/1403494810395827
Bottcher HM, Steimann M, Koch U, Bergelt C (2012) Return to work—experiences and expectations of cancer patients during inpatient rehabilitation. Rehabilitation 51:31–38
Singer S, Meyer A, Wienholz S, Briest S, Brown A, Dietz A, Binder H, Jonas S, Kortmann R-D, Stolzenburg J-U, Köhler U, Raßler J, Zwerenz R, Schröter K, Mehnert A, Löbner M, König HH, Riedel-Heller SG (2014) Early retirement in cancer patients with or without co-morbid mental health conditions: a prospective cohort study. Cancer 120(14):2199–2206. https://doi.org/10.1002/cncr.28716
Stigt JA, Uil SM, van Riesen SJH, Simons FJNA, Denekamp M, Shahin GM, Groen HJM (2013) A randomized controlled trial of postthoracotomy pulmonary rehabilitation in patients with resectable lung cancer. J Thorac Oncol 8(2):214–221. https://doi.org/10.1097/JTO.0b013e318279d52a
Schiel RO, Herzog W, Hof H, Debus J, Friederich HC, Brechtel A, Rummel J, Freytag P, Hartmann M (2013) Effect of systematic information about psychosocial support services during outpatient radiotherapy. A controlled trial. Strahlenther Onkol 189(7):579–585. https://doi.org/10.1007/s00066-013-0366-6
Braeken APBM, Lechner L, Eekers DBP, Houben RMA, van Gils FCJM, Ambergen T, Kempen GIJM (2013) Does routine psychosocial screening improve referral to psychosocial care providers and patient-radiotherapist communication? A cluster randomized controlled trial. Patient Educ Couns 93(2):289–297. https://doi.org/10.1016/j.pec.2013.06.015
Acknowledgements
We would like to acknowledge the time and effort of all doctors and nurses who helped in implementing this trial into daily routine in a large university hospital. We are also very grateful to all patients who participated in this trial.
Access to data
Susanne Singer had full access to all the data in the study and takes responsibility for the integrity of the data, the accuracy of the data analysis, and the decision to submit for publication. She also planned and conducted the data analysis.
Funding
This trial was funded by the German Federal Ministry of Health within the framework “Research within the German National Cancer Plan” (no. NKP-332-026). The grant provided salary support for Helge Danker and Julia Roick.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was granted by the University Medical Center Leipzig (no. 210-12-02072012).
Conflict of interest
We declare that there are no conflicts of interest.
Disclaimer
The German Federal Ministry of Health did not influence the trial design and procedures or the writing of this manuscript or the decision to submit it for publication.
Additional information
The manuscript was prepared in accordance with the CONSORT 2010 checklist (extension cluster-randomized trials).
Rights and permissions
About this article
Cite this article
Singer, S., Roick, J., Meixensberger, J. et al. The effects of multi-disciplinary psycho-social care on socio-economic problems in cancer patients: a cluster-randomized trial. Support Care Cancer 26, 1851–1859 (2018). https://doi.org/10.1007/s00520-017-4024-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-4024-x