Abstract
Purpose
Severe hypotension caused by anesthetic administration for anesthesia induction, which might cause ischemic stroke, myocardial injury, acute kidney injury and postoperative mortality, should be prevented. Anesthesiologists are familiar with ultrasound examination of the internal jugular vein (IJV). This study aimed to clarify whether ultrasonographic IJV evaluation just before induction could predict the occurrence of such hypotension.
Methods
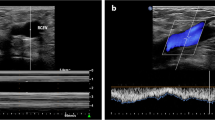
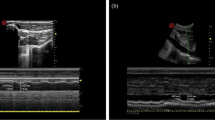
Adult patients undergoing surgery under general anesthesia were enrolled after excluding patients with cardiovascular disease or ASA-PS ≥ III. Ultrasonographic IJV images were recorded in both the supine and 10° Trendelenburg positions immediately before induction. Using these images, IJV area (IJV-A), diameter and change rate with posture were measured. Hypotension during induction was defined as mean BP < 60 mmHg or > 30% decrease from baseline.
Results
Hypotension during induction was observed in 37 of 82 patients. IJV-A in the Trendelenburg position was 2.02 ± 0.86 and 1.72 ± 0.68 in the hypotensive and non-hypotensive groups, respectively (P = 0.08). Logistic regression analysis performed using age, use of calcium antagonists, angiotensin converting enzyme inhibitors/angiotensin receptor blockers, baseline mean BP and IJV-A in the Trendelenburg position as variables showed that IJV-A in the Trendelenburg position was an independent predictor of hypotension, with an adjusted odds ratio of 3.11 (95% CI 1.07–9.03, P = 0.04). Area under the curve was 0.595 (95% CI 0.469–0.722) for IJV-A in the Trendelenburg position.
Conclusion
IJV-A in the Trendelenburg position was an independent predictor of hypotension during induction. Further study is required to examine the diagnostic accuracy of IJV-A as a predictor for hypotension during induction.

Similar content being viewed by others
References
Ebert TJ, Muzi M, Berens R, Goff D, Kampine JP. Sympathetic responses to induction of anesthesia in humans with propofol or etomidate. Anesthesiology. 1992;76:725–33.
Lonjaret L, Lairez O, Minville V, Geeraerts T. Optimal perioperative management of arterial blood pressure. Integr Blood Press Control. 2014;7:49–59.
Bijker JB, Persoon S, Peelen LM, Moons KG, Kalkman CJ, Kappelle LJ, van Klei WA. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case–control study. Anesthesiology. 2012;116:658–64.
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–15.
Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 2015;123:515–23.
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121:706–21.
Monk TG, Bronsert MR, Henderson WG, Mangione MP, Sum-Ping ST, Bentt DR, Nguyen JD, Richman JS, Meguid RA, Hammermeister KE. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology. 2015;123:307–19.
Zhang J, Critchley LA. Inferior vena cava ultrasonography before general anesthesia can predict hypotension after induction. Anesthesiology. 2016;124:580–9.
Juri T, Suehiro K, Tsujimoto S, Kuwata S, Mukai A, Tanaka K, Yamada T, Mori T, Nishikawa K. Pre-anesthetic stroke volume variation can predict cardiac output decrease and hypotension during induction of general anesthesia. J Clin Monit Comput. 2018;32:415–22.
Lin FQ, Li C, Zhang LJ, Fu SK, Chen GQ, Yang XH, Zhu CY, Li Q. Effect of rapid plasma volume expansion during anesthesia induction on haemodynamics and oxygen balance in patients undergoing gastrointestinal surgery. Int J Med Sci. 2013;10:355–61.
Kratz T, Steinfeldt T, Exner M, Dell Orto MC, Timmesfeld N, Kratz C, Skrodzki M, Wulf H, Zoremba M. Impact of focused intraoperative transthoracic echocardiography by anesthesiologists on management in hemodynamically unstable high-risk noncardiac surgery patients. J Cardiothorac Vasc Anesth. 2017;31:602–9.
Adler AC, Greeley WJ, Conlin F, Feldman JM. Perioperative anesthesiology ultrasonographic evaluation (PAUSE): a guided approach to perioperative bedside ultrasound. J Cardiothorac Vasc Anesth. 2016;30:521–9.
Rana S, Verma V, Bhandari S, Sharma S, Koundal V, Chaudhary SK. Point-of-care ultrasound in the airway assessment: a correlation of ultrasonography-guided parameters to the Cormack–Lehane Classification. Saudi J Anaesth. 2018;12:292–6.
Unluer EE, Kara PH. Ultrasonography of jugular vein as marker of hypovolemia in healthy volunteers. Am J Emerg Med. 2013;31:173–7.
Au AK, Steinberg D, Thom C, Shirazi M, Papanagnou D, Ku BS, Fields JM. Ultrasound measurement of inferior vena cava collapse predicts propofol-induced hypotension. Am J Emerg Med. 2016;34:1125–8.
Avcil M, Kapci M, Dagli B, Omurlu IK, Ozluer E, Karaman K, Yilmaz A, Zencir C. Comparision of ultrasound-based methods of jugular vein and inferior vena cava for estimating central venous pressure. Int J Clin Exp Med. 2015;8:10586–94.
Prekker ME, Scott NL, Hart D, Sprenkle MD, Leatherman JW. Point-of-care ultrasound to estimate central venous pressure: a comparison of three techniques. Crit Care Med. 2013;41:833–41.
Simon MA, Kliner DE, Girod JP, Moguillansky D, Villanueva FS, Pacella JJ. Detection of elevated right atrial pressure using a simple bedside ultrasound measure. Am Heart J. 2010;159:421–7.
Broilo F, Meregalli A, Friedman G. Right internal jugular vein distensibility appears to be a surrogate marker for inferior vena cava vein distensibility for evaluating fluid responsiveness. Rev Bras Ter Intensiva. 2015;27:205–11.
Cherpanath TG, Hirsch A, Geerts BF, Lagrand WK, Leeflang MM, Schultz MJ, Groeneveld AB. Predicting fluid responsiveness by passive leg raising: a systematic review and meta-analysis of 23 clinical trials. Crit Care Med. 2016;44:981–91.
Gok F, Sarkilar G, Kilicaslan A, Yosunkaya A, Uzun ST. Comparison of the effect of the Trendelenburg and passive leg raising positions on internal jugular vein size in critically ill patients. Int J Clin Exp Med. 2015;8:19037–43.
Sear JW, Jewkes C, Tellez JC, Foëx P. Does the choice of antihypertensive therapy influence haemodynamic responses to induction, laryngoscopy and intubation? Br J Anaesth. 1994;73:303–8.
Mets B. Management of hypotension associated with angiotensin–axis blockade and general anesthesia administration. J Cardiothorac Vasc Anesth. 2013;27:156–67.
Vaquero Roncero LM, Sánchez Poveda D, Valdunciel García JJ, Sánchez Barrado ME, Calvo Vecino JM. Perioperative use of angiotensin-converting-enzyme inhibitors and angiotensin receptor antagonists. J Clin Anesth. 2017;40:91–8.
Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A, Bodian CA. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005;101:622–8.
Coste J, Pouchot J. A grey zone for quantitative diagnostic and screening tests. Int J Epidemiol. 2003;32:304–13.
Monnet X, Jabot J, Maizel J, Richard C, Teboul JL. Norepinephrine increases cardiac preload and reduces preload dependency assessed by passive leg raising in septic shock patients. Crit Care Med. 2011;39:689–94.
Kalmar AF, Allaert S, Pletinckx P, Maes JW, Heerman J, Vos JJ, Struys MMRF, Scheeren TWL. Phenylephrine increases cardiac output by raising cardiac preload in patients with anesthesia induced hypotension. J Clin Monit Comput. 2018;32:969–76.
Nassar B, Deol GRS, Ashby A, Collett N, Schmidt GA. Trendelenburg position does not increase cross-sectional area of the internal jugular vein predictably. Chest. 2013;144:177–82.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Okamura, K., Nomura, T., Mizuno, Y. et al. Pre-anesthetic ultrasonographic assessment of the internal jugular vein for prediction of hypotension during the induction of general anesthesia. J Anesth 33, 612–619 (2019). https://doi.org/10.1007/s00540-019-02675-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02675-9