Abstract
The association between retinopathy in type 2 diabetes [diabetic retinopathy (DR)] and the C677T polymorphism in the methylenetetrahydrofolate reductase (MTHFR) gene has been investigated in several case-control studies. These studies rendered contradictory results, some indicating that the polymorphism is associated with the risk of developing DR whereas others concluded there is no association. To shed light on these inconclusive findings, a meta-analysis of all available studies relating the C677T polymorphism to the risk of developing DR was conducted. Four out of five identified studies included populations of East Asian descent, and only one involved samples from European descent (Caucasians). Overall, the meta-analysis suggested large heterogeneity between studies (p = 0.08, I2 = 52%) and marginal association between C677T transition and the risk of developing DR: random effects odds ratio (OR) = 1.39 [95% CI (1.05, 1.83)]. The sensitivity analysis [exclusion of one East Asian study with the controls not in Hardy–Weinberg equilibrium (HWE)] showed no heterogeneity (p = 0.25, I2 = 27%) and no significant association: fixed effects OR = 1.22 [95% CI (0.99, 1.51)] and random effects OR = 1.24 [95% CI (0.96, 1.60)]. The sub-group analysis for the East Asian population produced a significant association: fixed effects OR = 1.48 [95% CI (1.20, 1.83)] and random effects OR = 1.52 [95% CI (1.14, 2.03)]. However, sensitivity analysis in East Asians revealed that the association is marginal: fixed effects OR = 1.33 [95% CI (1.04, 1.70)] and random effects OR = 1.36 [95% CI (1.01, 1.83)]. There is a source of bias in the selected studies: the largest studies failed to show association while the smallest study claimed an association. The above findings reinforce the need for larger and more rigourous studies in this area.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is a serious chronic micro-angiopathic complication of types 1 and 2 diabetes and represents one of the leading causes of adult-acquired blindness in industrialised countries (Munier et al. 1998; Congdon et al. 2004). Various predisposing factors (Walker et al. 1985; van Leiden et al. 2003; Best and Chakravarthy 1997) have been identified already, but the pathogenesis of DR is not yet fully elucidated. The main risk factors are proven to be poor glycemic control and the duration of diabetes (Yanko et al. 1983; Klein et al. 1992). However, in large surveys, there were sub-groups of patients with type 2 diabetes who did not develop retinopathy despite poor glycemic control while others with fairly good control did develop retinopathy [UK Prospective Diabetes Study (UKPDS) Group 1998; The Diabetes Control and Complications Trial Research Group 1997]. Furthermore, sub-group analysis in the Diabetes Control and Complications Trial showed strong familial transmission for DR, especially in patients with severe proliferative retinopathy (The Diabetes Control and Complications Trial Research Group 1997). These facts represent convincing evidence that genetic factors contribute to the development of DR, but the genes conferring susceptibility remain to be identified (Simonelli et al. 2001; Warpeha and Chakravarthy 2003).
The methylenetetrahydrofolate reductase (MTHFR) gene is located on chromosome 1p36.3 (Goyette et al. 1994). Human MTHFR catalyses the conversion of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, a co-substrate for re-methylation of homocysteine to methionine. The C677T transition is a common ubiquitous missense mutation in the coding region of the MTHFR gene, which creates a HinfI recognition sequence and is detectable as a restriction fragment length polymorphism (RFLP). It causes an alanine to valine (Al222Val) amino acid substitution located in the anticipated catalytic domain of the enzyme (Frosst et al. 1995) and results in a thermo-labile MTHFR variant with reduced catalytic activity.
Homozygosity for the mutation (TT genotype) predisposes to significantly elevated plasma homocysteine levels (Frosst et al. 1995; Kang et al. 1991). Hyperhomocysteinemia is recognised as an independent risk factor for macroangiopathy (cerebrovascular or coronary artery disease) and for arterial or venous thrombosis (Bostom et al. 2001; Boushey et al. 1995; McCully 1996). The DR is a micro-angiopathic lesion primarily affecting the retinal capillaries and, therefore, its development might be related to MTHFR gene polymorphisms.
There are a number of recent case-control studies that investigated the association between the C677T polymorphism in the MTHFR gene and the diabetes-related micro-angiopathic complications, i.e. diabetic nephropathy and DR (Fujita et al. 1999; Yoshioka et al. 2003; Moczulski et al. 2003; Shpichinetsky et al. 2000). Results concerning the relationship between the risk of developing DR and the C677T mutation are inconclusive. Concretely, some of the studies indicate that the T allele of the MTHFR gene relative to the C allele is a risk factor for developing DR (Neugebauer et al. 1997; Sun et al. 2003; Maeda et al. 2003c) whereas other investigators report no genetic association (Yoshioka et al. 2003; Santos et al. 2003). However, the significant associations described in single studies between the T allele and DR are rather marginal and have, therefore, become subject to controversy (Yoshioka et al. 2003; Maeda et al. 2003b).
To provide an answer to these contradictory results, a meta-analysis (Lau et al. 1997) of all available studies relating the C677T polymorphism of the MTHFR gene to the risk of developing DR in patients with type 2 diabetes was conducted. In this meta-analysis, the estimates of the genetic association of each individual study and a pooled estimate of this association were obtained. In addition, the heterogeneity between studies and the existence of bias were investigated.
Materials and methods
Selection of studies
All studies that investigate the association of the C677T polymorphism in the MTHFR gene with the development of DR published before November 2004 were considered in the meta-analysis. The studies were identified by extensive computer-based searches of the PubMed and EBSCO databases. As a search criterion, we used the following: (MTHFR or “homocysteine metabolism”) and “DR” and “polymorphism”.
The retrieved publications were then read in their entirety in order to assess their appropriateness for inclusion in this meta-analysis. All references cited in the studies were also reviewed to identify additional published work not indexed by PubMed and EBSCO databases. Abstracts, case reports, editorials, and review articles were excluded. The search was restricted to articles in English. Case-control studies that determine the distribution of the C677T genotypes in cases with DR (proliferative and non-proliferative) and in controls free of DR were eligible for inclusion. Both cases and controls were patients with type 2 diabetes.
The distribution of genotypes in the control group was tested whether it is in Hardy–Weinberg equilibrium (HWE) using an exact test (Weir 1996) implemented by GDA software (Lewis and Zaykin 2001). Studies with controls not in HWE were subjected to a sensitivity analysis. Studies based on pedigree data were excluded since they investigated linkage (Zintzaras and Ioannidis 2005) and not association.
Data extraction
From each study, the following information was extracted: first author, journal, year of publication, racial descent of study population, demographics, matching, validity of the genotyping method, and the number of cases and controls for each C677T genotype. Frequencies of alleles were calculated, for the cases and the controls, from the corresponding genotype distributions. In addition, it was recorded whether the genotyping in each study was blinded to clinical status.
Meta-analysis
The meta-analysis examined the overall association of T allele with the risk of diabetic nephropathy relative to the C allele; and the contrast of homozygotes TT versus CC, the contrast TT versus (TC+CC), and the contrast (TT+TC) versus CC. All associations were indicated as odds ratios (ORs) with the corresponding 95% confidence interval (CI). Then, based on the individual ORs, a pooled OR was estimated.
Heterogeneity between studies was tested using the Q-statistic, which is a weighted sum of squares of the deviations of individual study OR estimates from the overall estimate (Cochran 1954). When the ORs were homogeneous, Q follows a chi-squared distribution with r-1 (r is the number of studies) degrees of freedom (d.f.). If p <0.10, then the heterogeneity was considered statistically significant. Heterogeneity was quantified with the I2 metric (I2 = (Q–d.f.)/Q), which is independent of the number of studies in the meta-analysis (Higgins et al. 2003). The I2 takes values between 0% and 100%, with higher values denoting greater degree of heterogeneity (I2 = 0–25%, no heterogeneity; I2 = 25–50%, moderate heterogeneity; I2 = 50–75%, large heterogeneity; I2 = 75–100%, extreme heterogeneity).
The pooled OR was estimated using fixed effects (Mantel–Haenszel) and random effects (DerSimonian and Laird) models. Random effects modelling assumes a genuine diversity in the results of various studies, and it incorporates into the calculations a between-study variance. Therefore, when there is heterogeneity between studies, then the pooled OR is estimated using the random effects model (Whitehead 2002). Adjusted estimates of OR were considered whenever possible in a separate analysis. A cumulative meta-analysis (Lau et al. 1992; Whitehead 1997) and recursive meta-analysis were carried out in order to evaluate the trend of pooled OR for the allele contrast (T versus C) in time. A differential magnitude of effect in large versus small studies, for the allele contrast, was checked using the Egger regression test for funnel plot asymmetry (Egger et al. 1997; Whitehead 2002). The test is based on the linear regression model: yi = α+βxi, where the dependent variable yi is the standardised estimate of θi = ln(ORi): \(y_i = \theta _i \sqrt {w_i } ,\) wi = 1/variance(θi), and the independent variable xi is the precision: \( x_i = \sqrt {w_i } , \) i.e. the study magnitude. A test of a differential magnitude of effect in large versus small studies would be a test of the null hypothesis that α is equal to zero (Ioannidis et al. 2003).
Whether the OR in the first study versus the pooled OR of the subsequent studies was different beyond chance (p <0.05) was assessed using the z-statistic, i.e. the difference of the natural logarithm of the ORs divided by the standard error of this difference (Ioannidis et al. 2003). In addition, the association between the C677T MTHFR gene polymorphism and DR was assessed with or without the first study.
The meta-analysis consisted of the main analysis, which includes all available data; the sub-group analysis of each population race; and sensitivity analyses, which examines the effect of excluding specific studies. Analyses were performed using Meta-Analyst (Joseph Lau, Boston, MA, USA), SAS software, and CVF90 with IMLS library (Zintzaras and Hadjigeorgiou 2004; Zintzaras and Stefanidis 2005; Whitehead 2002).
Results
Eligible studies
The literature review identified ten titles in PubMed and five titles in EBSCO that met the search criteria. After review, seven titles were judged to be potentially relevant. The abstracts of these articles were further reviewed, and full articles of selected studies were read to assess their appropriateness for meta-analysis. Five studies investigating the association between the MTHFR gene C677T polymorphism and DR met the inclusion criteria (Table 1).
Four studies were published in 2003 and one study in 1997. In four studies, the subjects were of East Asian descent (Neugebauer et al. 1997; Yoshioka et al. 2003; Sun et al. 2003; Maeda et al. 2003c), and in one study, the subjects were of European descent (Caucasians) (Santos et al. 2003). In four studies (Neugebauer et al. 1997; Sun et al. 2003; Santos et al. 2003; Yoshioka et al. 2003), the subjects’ ages (cases and controls) ranged from an average of 50.5 to 60 years, and gender was not evenly distributed; the fifth study does not report any demographic details (Maeda et al. 2003c).
In all studies, the cases, namely patients with type 2 diabetes showing DR, were well defined following similar inclusion criteria. In two studies (Sun et al. 2003; Santos et al. 2003) the existence of DR was assessed by means of ophthalmoscopy and/or biomicroscopy and/or fluorescein angiography while in the remaining studies the assessment method was not reported. In two studies, it was specified that cases and controls had no evidence of nephropathy (Maeda et al. 2003c; Yoshioka et al. 2003).
The controls were patients with type 2 diabetes without evidence for DR (Table 1). The duration of type 2 diabetes reported ranged in from 10 (Santos et al. 2003) to 12 years (Yoshioka et al. 2004). In one study (Sun et al. 2003), a duration of type 2 diabetes in controls longer than 10 years was reported.
In all studies genotypes were analysed using a validated genotyping method: PCR and digestion of the 198 bp PCR amplification product by HinflI, a restriction enzyme (Frosst et al. 1995).
Statistics summary
In total, the studies included 435 cases with type 2 diabetes and DR, and 620 controls with type 2 diabetes without DR.
The prevalence of allele T was 43% and 37% for the DR and control groups, respectively. The prevalence of homozygotes ΤΤ among patients with DR and controls was 19% and 14%, respectively. The prevalence of CC among patients with DR and controls was 33% and 40%, respectively. The prevalence of heterozygotes TC among patients with DR and controls was 48% and 46%, respectively (Table 2).
In one study (Sun et al. 2003), the distribution of the genotypes in the control group was not in HWE (p < 0.01), indicating genotyping errors and population stratification (Silverman and Palmer 2000; Xu et al. 2002). Therefore, a sensitivity analysis was carried out for this study; however, the produced results should be interpreted with caution.
Main results, sub-group and sensitivity analyses
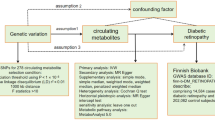
The main analysis for investigating the association of the allele T and the risk of developing DR relative to the allele C showed that there was large heterogeneity (p = 0.08, I2 = 52%) between the five studies, then the random effects pooled OR was marginally significant OR = 1.39 [95% CI (1.05, 1.83)] (Table 3 and Fig. 1).
C677T methylenetetrahydrofolate reductase (MTHFR) polymorphism and the risk of diabetic retinopathy (DR): contrast of allele T against C. Each study is shown by an odds ratio (OR) estimate with the corresponding 95% confidence interval (CI). The random effects pooled ORs are shown. The horizontal axis is plotted on a log scale
In sub-group analysis, there was moderate heterogeneity (p = 0.16, I2 = 42%) between the studies performed in the East Asian population. The random effects and fixed effects pooled ORs were significant, i.e. OR = 1.52 [95% CI (1.14, 2.03)] and OR = 1.48 [95% CI (1.20, 1.83)], respectively (Table 3).
In sensitivity analysis (exclusion of the study with the controls not in HWE), there was no between-study heterogeneity either for all studies in HWE (p = 0.25, I2 = 27%) or for the sub-group analysis (East Asians in HWE) (p = 0.28, I2 = 22%) (Table 3). Then, in the analysis for all studies in HWE, the fixed and random effects ORs were not significant: OR = 1.22 [95% CI (0.99, 1.51)] and OR = 1.24 [95% CI (0.96, 1.60)], respectively, and in East Asians, they were marginally significant: OR = 1.33 [95% CI (1.04, 1.70)] and OR = 1.31 [95% CI (1.01, 1.83)], respectively.
The genotype contrast of the homozygotes produced the same pattern of association with the allele contrast and no heterogeneity. The dominant model for the effect of T allele in the main analysis showed lack of association and for the East Asians significant association. However, sensitivity analyses for both dominant and recessive models showed no significant associations (Table 3).
Potential bias
None of the studies reported that genotyping was blinded to clinical status.
Cumulative meta-analysis and recursive meta-analysis for the allelic contrast showed that random effects pooled OR declined from 1.92 in 1997 (first study) to 1.35 in 2003 (five studies). The four studies published in 2003 produced a random effects OR of 1.32. There was also a suggestion that the two largest studies (Yoshioka et al. 2003; Santos et al. 2003) produced no significant associations and, in contrast, the smallest study produced significant association. The Egger test indicated that there is a differential magnitude of effect in large versus small studies. However, this result might not be so reliable since the number of studies is small (Ioannidis et al. 2003). There is no statistical difference between the OR of the first study versus the pooled OR of the subsequent studies (z = 1.10, p ≥ 0.05). The random effects pooled OR without the first study was OR = 0.76 [95% CI (0.56, 1.02)], and the between-study heterogeneity was moderate (p = 0.07, I2 = 56%).
Discussion
The MTHFR is involved in the re-methylation of homocysteine to methionine, and its C677T polymorphism yields a thermo-labile MTHFR variant with reduced enzymatic activity. This mutation is a genetic determinant of hyperhomocysteinemia in healthy subjects (Kang et al. 1991; Frosst et al. 1995) and also in patients with diabetes (Buysschaert et al. 2004). Hyperhomocysteinemia induces endothelial dysfunction (Constans et al. 1999) and has been implicated as a risk factor for atherosclerosis and atherothrombosis (McCully 1969; Frosst et al. 1995) but also for retinopathy in type 1 and in type 2 diabetes patients (Hoogeveen et al. 2000; Goldstein et al. 2004). Recent in vitro studies indicate that homocysteine and other thiol-containing reductive compounds (i.e. thiolactone) increase the expression of the vascular endothelial growth factor (VEGF) in cell cultures via activation of its transcription (Maeda et al. 2003a; Roybal et al. 2004). The VEGF is a pro-angiogenic factor known to play a key role in the development and progression of DR (Roybal et al. 2004; Ray et al. 2004). For these reasons, it may be readily postulated that the C677T MTHFR gene polymorphism might be involved in the development of DR.
The meta-analysis presented here included data from five case-control association studies that investigated the relation between the MTHFR polymorphism and DR in type 2 diabetes. Overall, 435 subjects who developed DR were analysed, along with their respective controls (617 diabetic subjects without DR). These numbers are relatively small and therefore any inferences have to be cautious (Ioannidis et al. 2003). The strength of the present analysis, however, is based on the aggregation of published case-control studies, thus there is more information for investigating the effect of the allele under investigation (Zintzaras and Hadjigeorgiou 2004; Muncer 2002).
The overall results indicated a marginal association of the C677T MTHFR polymorphism with DR and large heterogeneity between study results. Sensitivity analysis, however, showed that there was no heterogeneity and no significant association when the analysis was restricted to studies with the controls in HWE. Although the sub-group analysis in East Asians showed a significant association, the subsequent sensitivity analysis produced a marginal association and no heterogeneity. The study with the controls not in HWE (Sun et al. 2003) (East Asians) supported an association, and therefore, this result can be considered dubious. Among studies with the controls in HWE, the two largest studies (Santos et al. 2003; Yoshioka et al. 2003) (one in Caucasians and one in East Asians) failed to show association while only the smallest and first published study (Neugebauer et al. 1997) (East Asians) claimed a susceptibility effect to DR. This trend of results and the difference in results between the large and small studies might be a source of potential bias in the published studies.
None of the studies reported a polymorphism to be in linkage disequilibrium with the MTHFR gene polymorphism. However, the discrepancy of results might be due to other locus that are probably in linkage disequilibrium and affect the susceptibility to DR. In linkage studies, the MTHFR gene region (1p36.3) has not been reported to be an important susceptibility locus in DR or any other form of diabetic micro-angiopathy (Imperatore et al. 1998).
Variability of the case inclusion criteria is a central possible confounding factor in all studies on the role of genetic markers, and therefore, the strict selection criteria ensures a clear case, control, and definition for meta-analysis. In the meta-analysis presented here, the cases and controls were well defined with similar inclusion criteria, albeit they unavoidably cover a wide spectrum of disease, in terms of duration and other manifestations.
In the sub-group analysis by racial descent, Chinese and Japanese were analysed together since these two populations are more homogeneous to each other than to Caucasians. In investigating the genetic effects for complex diseases in sub-group meta-analyses, Ioannidis et al. (2004) categorised the racial descent into three main categories: (1) European descent (populations from Europe and subjects of European descent from Oceania, North America, and South America), (2) African descent (populations of sub-Saharan Africa and African Americans), and (3) East Asian descent (populations from China, Japan, Korea, Indochina, and Philippines). These traditionally defined groups are typically used in sub-group meta-analyses by racial descent (Ioannidis et al. 2004; Thomas and White 2002; Zintzaras and Stefanidis 2005; Zintzaras and Hadjigeorgiou 2004). However, the consistency of genetic effects across the traditionally defined racial groups does not necessarily mean that race-specific genetic effects are exactly the same (Ioannidis et al. 2004).
The first case-control association study (Neugebauer et al. 1997) that investigated the relation between the MTHFR polymorphism and DR in type 2 diabetes showed the existence of an association. Patients with retinopathy in that study had diabetes-induced advanced renal failure. This fact was criticised by Maeda et al. (2003a–c) and Yosioka et al. (2003), as renal disease per se causes enhanced homocysteine levels and accelerated atherosclerosis (Perna et al. 1999). However, the TT genotype in type 2 diabetes is associated with enhanced homocysteine levels (Sun et al. 2003) independently from the co-existence of nephropathy (Sun et al. 2004). Furthermore, in a previous study (Fujita et al. 1999), there was no nephropathy effect in association with the MTHFR genotype in patients with type 2 diabetes and DR.
In conclusion, the meta-analysis and the subsequent sensitivity analyses supported marginal association between the MTHFR gene C677T polymorphism and DR. This conclusion is based on a relatively small number of studies and participants, and any inferences have to be cautious. Taking also into account that DR is a complex disease with multi-factorial aetiology, a minor contributing pathogenetic role of the C677T MTHFR gene polymorphism in specific cases, and in co-operation with other factors, cannot be totally excluded. Therefore, the relationship between the C677T MTHFR polymorphism and DR still remains an unresolved issue, and long-term prospective studies are required.
References
Best RM, Chakravarthy U (1997) Diabetic retinopathy in pregnancy. Br J Ophthalmol 81:249–251
Bostom AG, Selhub J, Jacques PF, Rosenberg IH (2001) Power Shortage: clinical trials testing the “homocysteine hypothesis” against a background of folic acid-fortified cereal grain flour. Ann Intern Med 135:133–137
Boushey CJ, Beresford SA, Omenn GS, Motulsky AG (1995) A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes JAMA 274:1049–1057
Buysschaert M, Gala JL, Bessomo A, Hermans MP (2004) C677T methylene-tetrahydrofolate reductase mutation in type 2 diabetic patients with and without hyperhomocysteinaemia. Diabetes Metab 30:349–354
Cochran WG (1954) The combination of estimates from different experiments. Biometrics 10:101–129
Congdon N, O’Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, Kempen J, Taylor HR, Mitchell P (2004) Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 122:477–485
Constans J, Blann AD, Resplandy F, Parrot F, Seigneur M, Renard M, Amiral J, Guerin V, Boisseau MR, Conri C (1999) Endothelial dysfunction during acute methionine load in hyperhomocysteinaemic patients. Atherosclerosis 147:411–413
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10:111–113
Fujita H, Narita T, Meguro H, Ishii T, Hanyu O, Suzuki K, Kamoi K, Ito S (1999) No association between MTHFR gene polymorphism and diabetic nephropathy in Japanese type II diabetic patients with proliferative diabetic retinopathy. J Diabetes Complicat 13:284–287
Goldstein M, Leibovitch I, Yeffimov I, Gavendo S, Sela BA, Loewenstein A (2004) Hyperhomocysteinemia in patients with diabetes mellitus with and without diabetic retinopathy. Eye 18:460–465
Goyette P, Sumner JS, Milos R, Duncan AM, Rosenblatt DS, Matthews RG, Rozen R (1994) Human methylenetetrahydrofolate reductase: isolation of cDNA, mapping and mutation identification. Nat Genet 7:195–200
Higgins JP, Thompson SE (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Hoogeveen EK, Kostense PJ, Eysink PE, Polak BC, Beks PJ, Jakobs C, Dekker JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD (2000) Hyperhomocysteinemia is associated with the presence of retinopathy in type 2 diabetes mellitus: the Hoorn study. Arch Intern Med 160:2984–2990
Imperatore G, Hanson RL, Pettitt DJ, Kobes S, Bennett PH, Knowler WC (1998) Sib-pair linkage analysis for susceptibility genes for microvascular complications among Pima Indians with type 2 diabetes. Pima Diabetes Genes Group. Diabetes 47:821–830
Ioannidis JP, Ntzani EE, Trikalinos TA (2004) “Racial” differences in genetic effects for complex diseases. Nat Genet 36:1312–1318
Ioannidis JP, Trikalinos TA, Ntzani EE, Contopoulos-Ioannidis DG (2003) Genetic associations in large versus small studies: an empirical assessment. Lancet 361:567–571
Kang SS, Wong PW, Bock HG, Horwitz A, Grix A (1991) Intermediate hyperhomocysteinemia resulting from compound heterozygosity of methylenetetrahydrofolate reductase mutations. Am J Hum Genet 48:546–551
Klein R, Klein BE, Moss SE (1992) Epidemiology of proliferative diabetic retinopathy. Diabetes Care 15:1875–1891
Lau J, Antman EM, Jimenez-Silva J, Kupelnick B, Mosteller F, Chalmers TC (1992) Cumulative meta-analysis of therapeutic trials for myocardial infarction. N Engl J Med 327:248–254
Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127:820–826
Lewis PO, Zaykin D (2001) Genetic data analysis: computer program for the analysis of allelic data. Version 1.0 (d16c). Free program distributed by the authors over the internet from http://lewis.eeb.uconn.edu/lewishome/software.html
Maeda M, Yamamoto I, Fujio Y, Azuma J (2003a) Homocysteine induces vascular endothelial growth factor expression in differentiated THP-1 macrophages. Biochim Biophys Acta 1623:41–46
Maeda M, Yamamoto I, Fukuda M, Nishida M, Fujitsu J, Nonen S, Igarashi T, Motomura T, Inaba M, Fujio Y, Azuma J (2003b) Diabetic retinopathy possibly results from poor blood sugar control associated with MTHFR gene polymorphism in type 2 diabetic patients. Diabetes Care 26:1948
Maeda M, Yamamoto I, Fukuda M, Nishida M, Fujitsu J, Nonen S, Igarashi T, Motomura T, Inaba M, Fujio Y, Azuma J (2003c) MTHFR gene polymorphism as a risk factor for diabetic retinopathy in type 2 diabetic patients without serum creatinine elevation. Diabetes Care 26:547–548
McCully KS (1969) Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol 56:111–128
McCully KS (1996) Homocysteine and vascular disease. Nat Med 2:386–389
Moczulski D, Fojcik H, Zukowska-Szczechowska E, Szydlowska I, Grzeszczak W (2003) Effects of the C677T and A1298C polymorphisms of the MTHFR gene on the genetic predisposition for diabetic nephropathy. Nephrol Dial Transplant 18:1535–1540
Muncer S (2002) Response to: Power dressing and meta-analysis: incorporating power analysis into meta-analysis. J Adv Nursing 38:274–280
Munier A, Gunning T, Kenny D, O’Keefe M (1998) Causes of blindness in the adult population of the Republic of Ireland. Br J Ophthalmol 82:630–633
Neugebauer S, Baba T, Kurokawa K, Watanabe T (1997) Defective homocysteine metabolism as a risk factor for diabetic retinopathy. Lancet 349:473–474
Perna AF, Castaldo P, Ingrosso D, De Santo NG (1999) Homocysteine, a new cardiovascular risk factor, is also a powerful uremic toxin. J Nephrol 12:230–240
Ray D, Mishra M, Ralph S, Read I, Davies R, Brenchley P (2004) Association of the VEGF gene with proliferative diabetic retinopathy but not proteinuria in diabetes. Diabetes 53:861–864
Roybal CN, Yang S, Sun CW, Hurtado D, Vander Jagt DL, Townes TM, Abcouwer SF (2004) Homocysteine increases the expression of vascular endothelial growth factor by a mechanism involving endoplasmic reticulum stress and transcription factor ATF4. J Biol Chem 279:14844–14852
Santos KG, Tschiedel B, Schneider J, Souto K, Roisenberg I (2003) Diabetic retinopathy in Euro-Brazilian type 2 diabetic patients: relationship with polymorphisms in the aldose reductase, the plasminogen activator inhibitor-1 and the methylenetetrahydrofolate reductase genes. Diabetes Res Clin Pract 61:133–136
Shpichinetsky V, Raz I, Friedlander Y, Goldschmidt N, Wexler ID, Ben Yehuda A, Friedman G (2000) The association between two common mutations C677T and A1298C in human methylenetetrahydrofolate reductase gene and the risk for diabetic nephropathy in type II diabetic patients. J Nutr 130:2493–2497
Silverman EK, Palmer LJ (2000) Case-control association studies for the genetics of complex respiratory diseases. Am J Respir Cell Mol Biol 22:645–648
Simonelli F, Testa F, Bandello F (2001) Genetics of diabetic retinopathy. Semin Ophthalmol 16:41–51
Sun J, Xu Y, Zhu Y, Lu H (2004) Genetic polymorphism of methylenetetrahydrofolate reductase as a risk factor for diabetic nephropathy in Chinese type 2 diabetic patients. Diabetes Res Clin Pract 64:185–190
Sun J, Xu Y, Zhu Y, Lu H, Deng H, Fan Y, Sun S, Zhang Y (2003) The relationship between MTHFR gene polymorphisms, plasma homocysteine levels and diabetic retinopathy in type 2 diabetes mellitus. Chin Med J (Engl) 116:145–147
The Diabetes Control, Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
The Diabetes Control, Complications Trial Research Group (1997) Clustering of long-term complications in families with diabetes in the diabetes control and complications trial. Diabetes 46:1829–1839
Thomas DC, White JS (2002) Point: population stratification: a problem for case-control studies of candidate-gene associations? Cancer Epidemiol Biomarkers Prev 11:505–512
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853
van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD, Polak BC (2003) Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Arch Ophthalmol 121:245–251
Walker JM, Cove DH, Beevers DG, Dodson PM, Leatherdale BA, Fletcher RF, Wright AD (1985) Cigarette smoking, blood pressure and the control of blood glucose in the development of diabetic retinopathy. Diabetes Res 2:183–186
Warpeha KM, Chakravarthy U (2003) Molecular genetics of microvascular disease in diabetic retinopathy. Eye 17:305–311
Weir BS (1996) Genetic data analysis II: methods for discrete population genetic data. Sinauer Associates, Sunderland, MA, USA
Whitehead A (1997) A prospectively planned cumulative meta-analysis applied to a series of concurrent clinical trials. Stat Med 16:2901–2913
Whitehead A (2002) Meta-analysis of controlled clinical trials. Wiley, Chichester
Xu J, Turner A, Little J, Bleecker ER, Meyers DA (2002) Positive results in association studies are associated with departure from Hardy–Weinberg equilibrium: hint for genotyping error?. Hum Genet 111:573–574
Yanko L, Goldbourt U, Michaelson IC, Shapiro A, Yaari S (1983) Prevalence and 15-year incidence of retinopathy and associated characteristics in middle-aged and elderly diabetic men. Br J Ophthalmol 67:759–765
Yoshioka K, Yoshida T, Takakura Y, Kogure A, Umekawa T, Toda H, Yoshikawa T (2003) No association between the MTHFR gene polymorphism and diabetic retinopathy in type 2 diabetic patients without overt nephropathy. Diabetes Care 26:1947–1948
Yoshioka K, Yoshida T, Umekawa T, Kogure A, Takakura Y, Toda H, Yoshikawa T (2004) Methylenetetrahydrofolate reductase gene polymorphism is not related to diabetic nephropathy in Japanese Type 2 diabetic patients. Diabet Med 21:1051–1052
Zintzaras E, Hadjigeorgiou GM (2004) Association of paraoxonase 1 gene polymorphisms with risk of Parkinson’s disease: a meta-analysis. J Hum Genet 49:474–481
Zintzaras E, Ioannidis JP (2005) Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol 28:123–137
Zintzaras E, Stefanidis I (2005) Association between the GLUT1 gene polymorphism and the risk of diabetic nephropathy: a meta-analysis. J Hum Genet 50:84–91
Acknowledgements
We thank Dr. M. Maeda for providing information on the MTHFR genotype distribution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zintzaras, E., Chatzoulis, D.Z., Karabatsas, C.H. et al. The relationship between C677T methylenetetrahydrofolate reductase gene polymorphism and retinopathy in type 2 diabetes: a meta-analysis. J Hum Genet 50, 267–275 (2005). https://doi.org/10.1007/s10038-005-0250-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-005-0250-z
Keywords
This article is cited by
-
Effect of IFN-γ +874 T/A polymorphism on clinical manifestations of dengue: a meta-analysis
Journal of Genetics (2021)
-
Association between KIF6 rs20455 polymorphism and the risk of coronary heart disease (CHD): a pooled analysis of 50 individual studies including 40,059 cases and 64,032 controls
Lipids in Health and Disease (2018)
-
Multilocus genetic risk score for diabetic retinopathy in the Han Chinese population of Taiwan
Scientific Reports (2018)
-
Association between glutathione S-transferases M1 and T1 gene polymorphisms and prostate cancer risk: a systematic review and meta-analysis
Tumor Biology (2014)
-
The association between the polymorphism rs2231142 in the ABCG2 gene and gout risk: a meta-analysis
Clinical Rheumatology (2014)