Abstract
Background
Laparoscopic gastrectomy has become a common surgical treatment for gastric cancer in eastern Asian countries. However, a large-scale prospective study to investigate the benefit of laparoscopy-assisted distal gastrectomy (LADG) regarding long-term outcomes has never been reported. We have already reported the short-term outcomes of this study. Here we report long-term outcomes as the secondary endpoints of this study after a 5-year follow-up period.
Methods
This study comprised patients with clinical stage I gastric cancer who were able to undergo a distal gastrectomy. LADG with D1 plus suprapancreatic lymph node dissection was performed by credentialed gastric surgeons who had each conducted at least 30 LADG and 30 open gastrectomy procedures. The primary endpoint was the proportion of patients who developed either anastomotic leakage or pancreatic fistula. The secondary endpoints included overall survival and relapse-free survival.
Results
From November 2007 to September 2008, 176 eligible patients were enrolled, comprising 140 patients with pathological stage IA disease, 23 patients with pathological stage IB disease, 9 patients with pathological stage II disease, and 4 patients with pathological stage IIIA disease. No patients had recurrent disease, and three of the patients died within the follow-up period. The 5-year overall survival was 98.2% (95% confidence interval 94.4–99.4%) and the 5-year relapse-free survival was 98.2% (95% confidence interval 94.4–99.4%).
Conclusions
The long-term outcomes of stage I gastric cancer patients undergoing LADG seem comparable to those of patients undergoing an open procedure, although this result should be confirmed by a randomized control trial. We have already completed accrual of 921 patients for a multicenter randomized phase III trial (JCOG0912) to confirm the noninferiority of LADG compared with open gastrectomy in terms of relapse-free survival.
Similar content being viewed by others
Introduction
Laparoscopy-assisted distal gastrectomy (LADG) was first performed more than 20 years ago in Japan to treat gastric cancer [1], and since then the use of such procedures has gradually increased. A 2009 Japanese survey found an increase in the total number of gastric cancer patients treated by laparoscopic surgery annually, and that this increase was highest among patients with cT1N0 (stage IA), cT1N1 (stage IB), and cT2N0 (stage IB) tumors [2]. The safety of LADG with respect to morbidity and mortality has been demonstrated in several prospective multicenter trials [3, 4]. We [3] confirmed the safety of LADG performed by credentialed surgeons in a multi-institutional phase II trial (JCOG0703) for stage I gastric cancer patients looking at early surgical outcomes such as anastomotic leakage and pancreatic fistula formation. In that study the total proportion of patients who developed anastomotic leakage or pancreatic fistula was 1.7%, and the overall proportion of hospital grade 3 or grade 4 adverse events was 5.1%. These complication rates are lower than those reported previously [5, 6]. Similarly, Kim et al. [4] demonstrated no significant differences in morbidity or mortality between LADG and conventional open gastrectomy in a prospective randomized phase III trial (KLASS-I) in early gastric cancer patients.
In 2007 when this study was planned, there were few retrospective studies based on a large number of cases to investigate long-term outcomes of LADG for early gastric cancer. Huscher et al. [7] showed long-term outcomes of gastric cancer patients prospectively and reported no statistically significant difference in the 5-year overall survival (OS) rate between patients treated with open and laparoscopic procedures (55.4% vs 58.9%); however, that study had only a small sample size and enrolled patients with both early and advanced gastric cancer.
Although multicenter retrospective large number analysis demonstrated comparable long-term oncological outcomes of laparoscopy-assisted gastrectomy [6] and open surgery for gastric cancer recurrence, there is still little knowledge of the long-term outcomes of LADG for gastric cancer in terms of prospective observation.
Here we report long-term outcomes as the secondary endpoints of JCOG0703 multi-institutional phase II trial for stage I gastric cancer patients after a 5-year follow-up period. Five-year overall survival (OS) and relapse-free survival (RFS) were studied to assess outcomes.
Patients and methods
Study design and participants
Our study was designed as a multicenter, prospective phase II trial. The Japan Clinical Oncology Group (JCOG) Protocol Review Committee and the institutional review boards of each of the 14 participating Japanese hospitals approved the study protocol before its commencement.
The design of the trial was reported previously [3].
The patient inclusion criteria were as follows: histologically confirmed adenocarcinoma of the stomach; a clinical stage IA (T1N0) or stage IB [T1N1/T2(MP, SS)N0] tumor according to the 13th Japanese classification of gastric carcinoma, corresponding to the second English edition [8]; no indications for endoscopic mucosal resection according to the Japanese endoscopic treatment guidelines [9] [“no indications for endoscopic mucosal resection” corresponds to a clinical node-positive or clinical node-negative status by any of the following criteria: a tumor size 2 cm or larger, invasion of the submucosa or deeper, a histologically undifferentiated type, the presence of an ulcer or ulcerative scar (in cases of a depressed tumor), or the impossibility of en bloc resection]; a distal-gastrectomy-treatable tumor located in the middle or lower third of the stomach; no involvement of the duodenum; a patient age of 20–80 years; an Eastern Cooperative Oncology Group performance status of 0 or 1; a body mass index (BMI) of less than 30 kg/m2; the absence of tumor recurrence after endoscopic mucosal resection; no prior upper abdominal surgery or intestinal resection other than an appendectomy; no prior chemotherapy or radiotherapy for any malignancy; adequate organ function; and written informed consent.
The exclusion criteria were as follows: a synchronous or metachronous (within 5 years) malignancy other than carcinoma in situ or mucosal cancer; pregnancy or lactation; severe mental disease; the systemic administration of corticosteroids; unstable angina or myocardial infarction within 6 months before registration; uncontrolled hypertension; diabetes mellitus (both uncontrolled and controlled with insulin); and severe respiratory disease requiring continuous oxygen therapy.
After the inclusion/exclusion criteria had confirmed by patients telephoning or faxing the JCOG Data Center, the patients were registered in the JCOG0703 trial.
Surgery [3]
Patients in this study underwent LADG with D1 plus suprapancreatic node dissection, with the extent of dissection decided according to the surgical T and N category of the tumor, based on the gastric cancer treatment guidelines in Japan, second edition [9].
Patients requiring a pylorus-preserving distal gastrectomy, but not a total gastrectomy, were included in this trial, and the LADG was converted to open distal gastrectomy (ODG) if the intraoperative findings revealed a tumor stage of II or greater. The size of the mini-laparotomy incision was 6 cm or less, but the reconstruction approach, surgical method following resection, and the use of postoperative analgesia were not specified. Requests for analgesia were recorded for postoperative days 5–10. Adjuvant chemotherapy (S-1 for 1 year) was recommended for patients with curative resection and a pathological stage II, IIIA, or IIIB tumor.
Quality control of surgery
All surgeons participating in this trial had significant experience in gastric cancer surgery, particularly LADG and ODG (at least 30 of each was a prerequisite), and all agreed to the technical details for LADG before this trial commenced. We also centrally reviewed the surgical procedure by photographing all the cases and by videotaping selected cases arbitrarily. To assess compliance with the standard lymphadenectomy procedure, dissected nodes at all stations were counted, and the results were monitored.
Follow-up
All enrolled patients were followed up at least every 6 months for the first 2 years and then annually for another 3 years until 5 years after the close of registration.
Yearly follow-up for each patient comprised upper gastrointestinal endoscopy, abdominal computed tomography, and routine blood tests.
Endpoints
The primary study endpoint was the proportion of development of either an anastomotic leakage of grade 1 or greater or a pancreatic fistula of at least grade 2 among all surgically treated patients. The secondary endpoints for all patients were OS, RFS, the proportions of LADG completions and conversions from LADG to ODG, surgical morbidity, and short-term clinical outcomes. Adverse events were classified based on the Common Terminology Criteria for Adverse Events version 3.0. OS was defined as the number of days from enrollment to death from any cause; it was censored at the last day the patient was alive. RFS was defined as the number of days from enrollment to relapse or death from any cause; it was censored at the last day the patient was alive without any evidence of relapse. All these secondary outcomes except for OS and RFS were included in our previous publication [3].
Statistical methods
The previous report of this trial confirmed the safety of LADG in terms of the incidence of anastomotic leakage or pancreatic fistula [3]. This article presents further trial results regarding long-term outcomes. OS and RFS were estimated by the Kaplan–Meier method. The planned sample size was 170 patients with one-sided alpha of 10%, power of 90%, the threshold value in the primary endpoint of 8%, and the expected value of 3%.
All statistical analyses were performed with SAS version 9.1 (SAS Institute, Cary, NC, USA). This study was registered with the University Hospital Medical Information Network Clinical Trials Registry (http://www.umin.ac.jp/ctr/), under identification number UMIN000000874.
The JCOG Data Center and study coordinator conducted central monitoring and issued a monitoring report every 6 months to evaluate study progress and increase data integrity and patient safety. For quality assurance, site audits were performed by the JCOG Audit Committee (not on a study-specific basis but for the study group).
Results
Patient characteristics
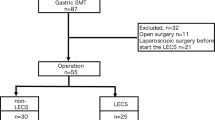
From November 2007 to September 2008, 177 patients from 14 hospitals with institutional review board approval were registered in the trial. The final analysis was conducted in September 2013, 5 years after the last patient was enrolled. One patient was deemed ineligible after enrollment as no written informed consent was provided, which originated from a miscommunication among the patient’s physicians. Table 1 shows details of the characteristics of all enrolled patients. The clinical and histological stages described are based on the Japanese classification of gastric carcinoma, second English edition [8], whereas the results shown in Table 2 are based on both the Japanese classification of gastric carcinoma and the Union for International Cancer Control TNM classification, sixth edition.
The median patient age was 59 years, with a male-to-female ratio of approximately 1:1. More than 90% of the patients had clinical stage IA (cT1N0) disease and a median BMI of 21.8 kg/m2. About two thirds of the tumors were located in the middle third of the stomach. Table 2 also summarizes the histological findings. Early gastric cancer (T1) was confirmed pathologically in approximately 90% of the patients. Of the total patient group, 15.3% had nodal involvement (27 of 176 patients), and approximately 20% of these node-positive patients had suprapancreatic node metastasis. The accuracy of the preoperative diagnosis of stage I (Japanese classification of gastric carcinoma) disease was 92.6%, and 14 patients underwent adjuvant chemotherapy with S-1 (8.0%).
Late postoperative complications
Grade 3 late postoperative complications occurred in six patients (3.4%). They were anastomotic stenosis (one patient; 0.6%), bowel obstruction (one patient; 0.6%), low hemoglobin count (one patient; 0.6%), cholangitis (one patient; 0.6%), and cholecystitis (two patients; (1.1%). There were no grade 4 adverse events.
Long-term survival outcomes
No patients had recurrence, although three patients died without recurrence during the follow-up (two patients died of other diseases and one patient died of an unknown cause). The 5-year OS was 98.2% (95% confidence interval 94.4–99.4%) (Fig. 1a) and the 5-year RFS was 98.2% (95% confidence interval 94.4–99.4%) (Fig. 1b).
Discussion
This prospective study showed the long-term outcomes of patients who underwent LADG for stage I gastric cancer. The 5-year survival rate of 98.2% for both OS and RFS is comparable with that of previous retrospective studies assessing laparoscopic gastrectomy [10,11,12]. For open surgery, Nashimoto et al. [13] reported survival outcomes of 13,626 patients with primary gastric cancer treated with open procedures in 2002 as Union for International Cancer Control and Japanese Gastric Cancer Association 5-year survival of 92.2% and 92.3% respectively for stage IA cancer patients and 85.3% and 84.7% respectively for stage IB cancer patients, which are comparable with the long-term survival findings for the present series.
Kim et al. [12] reported the OS after matching for the operation method and surgeons did not show any significant differences between open gastrectomy and laparoscopic gastrectomy for all stages of cancer. A recent observational study of 1848 stage I gastric cancer patients adjusted the backgrounds using propensity matching with confounding factors to demonstrate favorable long-term survival of LADG patients compared with ODG patients. After such propensity matching, the 5-year OS was 96.3% for the ODG group compared with 97.1% for LADG patients [14].
A large-scale retrospective multicenter study from the Japanese Laparoscopic Surgery Study Group showed excellent long-term outcomes, with 5-year disease-free survival of 99.8% in patients with stage IA cancer, 98.7% in patients with stage IB cancer, and 85.7% in patients with stage II cancer [6]; however, this study was retrospective.
The previous retrospective studies assessing the long-term outcome of LADG for gastric cancer showed a proportion of 2.5–3.5% for any recurrence in stage I cancer [11, 15, 16]. Although our evaluation of long-term survival following LADG for clinical stage I gastric cancer patients showed no recurrence over the 5-year observation period, these patients include 7.4% with a histologically advanced stage of gastric cancer greater than stage II. These results are also comparable with those for patients treated by conventional open procedures.
The first probable reason for this excellent long-term outcome is the relatively high proportion of stage IA cancer patients (approximately 80%) and the relatively low proportion of stage IB cancer patients (13%) among all stage I cancer patients. A previous study reported the proportion of stage IB cancer patients among stage I cancer patients was about 25% [17].
Second, the relatively high proportion of female patients in this study could have influenced the long-term outcomes, because several studies have described better rates of survival for female gastric cancer patients compared with male gastric cancer patients [18]. It is possible that a higher than average number of female patients might have been arbitrarily selected in the patient recruitment because female patients with their relatively lower amount of intraoperative fat are favored for laparoscopic procedures.
Additionally, this study recruited patients with a relatively low BMI, which could partially influence the better long-term outcomes. The initial protocol design of this study excluded patients with a BMI greater than 30 kg/m2 (the median BMI was 21.8 kg/m2), which makes the laparoscopic procedures easier to perform. In contrast, the median BMI of patients in Western countries is 26–29 kg/m2, which results in relatively high morbidities [3]. This factor of patient recruitment could have introduced a selection bias into this study.
Third, the LADG was performed only by credentialed surgeons, who had to meet strict selection criteria. We selected only surgeons who had performed more than 30 LADG procedures and more than 30 ODG procedures before this trial [3]. These surgeons could therefore perform precise and accurate lymph node dissection, improving the oncological validity of the study and consequently the long-term patient outcomes. Although the histological node status showed more than 15% of lymph node metastasis in the stage I cancer patients, which is a relatively high proportion of lymph node metastasis compared with previous studies, lymph node clearance might be sufficiently done in this trial. These credentialed operators also achieved a low proportion of conversions to ODG (2.9%). These proportions were low enough to justify a subsequent phase III trial (LADG vs ODG) [13, 18]. Furthermore, the relatively high number of undifferentiated cancer patients in this series could underlie the high incidence of lymph node metastasis because of the higher number of patients initially treated by endoscopic submucosal dissection. Many of the early gastric cancer patients were treated by endoscopic submucosal dissection, and most of the undifferentiated cancer was treated by surgery as an extra indication of endoscopic submucosal dissection cases.
Fourth, as described in previous reports [3], the proportion of patients who developed severe complications was low. The proportion of anastomotic leakage or pancreatic fistula formation was only 1.7%, which was what we expected from this study design and is lower than that reported in previous publications [5, 18]. Several studies demonstrated that postoperative complications were related to poor prognosis [19]. Thus, the low incidence of complications in this study would have advantages for long-term survival.
Bowel obstruction was not common after laparoscopic gastrectomy as in previous reports. Although this finding requires prospective evaluation, this study suggests that LADG for gastric cancer is a feasible procedure from the standpoint of late postoperative complications [16, 17].
This study had some limitations. First, it was a single-arm study and the long-term outcomes could not be compared with those of conventional open gastrectomy. This study also recruited only patients with a relatively low BMI and included more female patients and those with more undifferentiated carcinoma; these patient groups might have influenced the relatively good long-term survival observed in this study. Additionally, all surgical procedures were performed by outstanding credentialed surgeons and therefore the data might not represent the total data of Japanese patients.
In conclusion, we demonstrated long-term outcomes of stage I gastric cancer patients treated by LADG that were comparable to those of patients treated by an open procedure. Enrollment of patients for a subsequent phase III trial (JCOG0912) has been completed. LADG will be an alternative procedure in clinical IA/IB gastric cancer if the noninferiority of LADG with regard to RFS is confirmed.
References
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–8.
Etoh T, Shiraishi N, Kitano S. Current trends of laparoscopic gastrectomy for gastric cancer in Japan. Asian J Endosc Surg. 2009;2:18–21.
Katai H, Sasako M, Fukuda H, Nakamura K, Hiki N, Sakai M, Yamaue M, Yoshikawa T, Kojima K. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703). Gastric Cancer. 2010;13:238–44.
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016;263(1):28–35.
Fujiwara M, Kodera Y, Kasai Y, Kanyama Y, Hibi K, Ito K, et al. Laparoscopy-assisted distal gastrectomy with systemic lymphnode dissection for early gastric carcinoma: a review of 43 cases. J Am Coll Surg. 2003;196:75–81.
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007;245:68–72.
Huscher CG, Mingoli A, Sgarzini G, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer. Ann Surg. 2005;241:232–7.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma. 2nd English edition. Gastric Cancer. 1998;1:10–24.
Nakajima T. Gastric cancer treatment guidelines in Japan. Gastric Cancer. 2002;5:1–5.
Song J, Lee HJ, Cho GS, Han SU, Kim MC, Ryu SW, Kim W, Song KY, Kim HH, Hyung WJ, Korean Laparoscopic Gastrointestinal Surgery Study (KLASS) Group. Recurrence following laparoscopy-assisted gastrectomy for gastric cancer: a multicenter retrospective analysis of 1,417 patients. Ann Surg Oncol. 2010;17:1777–86.
Lee JH, Lee CM, Son SY, Ahn SH, Park do J, Kim HH. Laparoscopic versus open gastrectomy for gastric cancer: long-term oncologic results. Surgery. 2014;155:154–64
Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, Ryu SW, Cho GS, Song KY, Ryu SY. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014;32:627–33
Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, Tsujitani S, Seto Y, Furukawa H, Oda I, Ono H, Tanabe S, Kaminishi M. Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer. 2013;16:1–27.
Honda M, Hiki N, Kinoshita T, Yabusaki H, Abe T, Nunobe S, et al. Long-term outcomes of laparoscopic versus open surgery for clinical stage I gastric cancer: the LOC-1 study. Ann Surg. 2016;264:214–22.
Sugita H, Kojima K, Inokuchi M, Kato K. Long-term outcomes of laparoscopic gastrectomy for gastric cancer. J Surg Res. 2015;193:190–5.
Nakagawa M, Kojima K, Inokuchi M, Kato K, Sugita H, Kawano T, Sugihara K. Patterns, timing and risk factors of recurrence of gastric cancer after laparoscopic gastrectomy: reliable results following long-term follow-up. Eur J Surg Oncol. 2014;40:1376–82.
Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol. 2005;91:90–4.
Inomata M, Yasuda K, Shiraishi N, Kitano S. Clinical evidences of laparoscopic versus open surgery for colorectal cancer. Jpn J Clin Oncol. 2009;39:471–7.
Kubota T, Hiki N, Sano T, Nomura S, Nunobe S, Kumagai K, Aikou S, Watanabe R, Kosuga T, Yamaguchi T. Prognostic significance of complications after curative surgery for gastric cancer. Ann Surg Oncol. 2014;21:891–8.
Acknowledgements
This study was supported in part by Grants-in-Aid for Cancer Research (17S-3, 17S-5, 17-11, 20S-3, 20S-6, 23-A-19, 26-A-4) from the Ministry of Health, Labour and Welfare, Japan.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for their being included in the study.
Rights and permissions
About this article
Cite this article
Hiki, N., Katai, H., Mizusawa, J. et al. Long-term outcomes of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG0703). Gastric Cancer 21, 155–161 (2018). https://doi.org/10.1007/s10120-016-0687-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0687-0