Abstract
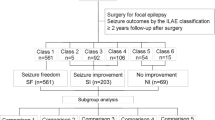
Epilepsy is a debilitating neurological disorder affecting approximately 1 % of the world’s population. Drug-resistant focal epilepsies are potentially surgically remediable. Although epilepsy surgery is dramatically underutilized among medically refractory patients, there is an expanding collection of evidence supporting its efficacy which may soon compel a paradigm shift. Of note is that a recent randomized controlled trial demonstrated that early resection leads to considerably better seizure outcomes than continued medical therapy in patients with pharmacoresistant temporal lobe epilepsy. In the present review, we provide a timely update of seizure freedom rates and predictors in resective epilepsy surgery, organized by the distinct pathological entities most commonly observed. Class I evidence, meta-analyses, and individual observational case series are considered, including the experiences of both our institution and others. Overall, resective epilepsy surgery leads to seizure freedom in approximately two thirds of patients with intractable temporal lobe epilepsy and about one half of individuals with focal neocortical epilepsy, although only the former observation is supported by class I evidence. Two common modifiable predictors of postoperative seizure freedom are early operative intervention and, in the case of a discrete lesion, gross total resection. Evidence-based practice guidelines recommend that epilepsy patients who continue to have seizures after trialing two or more medication regimens should be referred to a comprehensive epilepsy center for multidisciplinary evaluation, including surgical consideration.
Similar content being viewed by others
References
Abou-Khalil B (2007) An update on determination of language dominance in screening for epilepsy surgery: the Wada test and newer noninvasive alternatives. Epilepsia 48(3):442–455. doi:10.1111/j.1528-1167.2007.01012.x
Althausen A, Gleissner U, Hoppe C, Sassen R, Buddewig S, von Lehe M, Schramm J, Elger CE, Helmstaedter C (2012) Long-term outcome of hemispheric surgery at different ages in 61 epilepsy patients. J Neurol Neurosurg Psychiatry 84:529–536. doi:10.1136/jnnp-2012-303811
Aronica E, Becker AJ, Spreafico R (2012) Malformations of cortical development. Brain Pathol 22(3):380–401. doi:10.1111/j.1750-3639.2012.00581.x
Aronica E, Leenstra S, van Veelen CW, van Rijen PC, Hulsebos TJ, Tersmette AC, Yankaya B, Troost D (2001) Glioneuronal tumors and medically intractable epilepsy: a clinical study with long-term follow-up of seizure outcome after surgery. Epilepsy Res 43(3):179–191
Awad I, Jabbour P (2006) Cerebral cavernous malformations and epilepsy. Neurosurg Focus 21(1):e7
Barkovich AJ, Chuang SH (1990) Unilateral megalencephaly: correlation of MR imaging and pathologic characteristics. AJNR Am J Neuroradiol 11(3):523–531
Barkovich AJ, Kuzniecky RI, Jackson GD, Guerrini R, Dobyns WB (2001) Classification system for malformations of cortical development: update 2001. Neurology 57(12):2168–2178
Baumann CR, Schuknecht B, Lo Russo G, Cossu M, Citterio A, Andermann F, Siegel AM (2006) Seizure outcome after resection of cavernous malformations is better when surrounding hemosiderin-stained brain also is removed. Epilepsia 47(3):563–566. doi:10.1111/j.1528-1167.2006.00468.x
Begley CE, Beghi E, Beran RG, Heaney D, Langfitt JT, Pachlatko C, Silfvenius H, Sperling MR, Wiebe S (2002) ILAE Commission on the Burden of Epilepsy, Subcommission on the Economic Burden of Epilepsy: final report 1998–2001. Epilepsia 43(6):668–673
Bekelis K, Missios S, Desai A, Eskey C, Erkmen K (2012) Magnetic resonance imaging/magnetic resonance angiography fusion technique for intraoperative navigation during microsurgical resection of cerebral arteriovenous malformations. Neurosurg Focus 32(5):E7. doi:10.3171/2012.1.FOCUS127
Berger MS (1996) Minimalism through intraoperative functional mapping. Clin Neurosurg 43:324–337
Berger MS, Ghatan S, Haglund MM, Dobbins J, Ojemann GA (1993) Low-grade gliomas associated with intractable epilepsy: seizure outcome utilizing electrocorticography during tumor resection. J Neurosurg 79(1):62–69. doi:10.3171/jns.1993.79.1.0062
Berman JI, Berger MS, Chung SW, Nagarajan SS, Henry RG (2007) Accuracy of diffusion tensor magnetic resonance imaging tractography assessed using intraoperative subcortical stimulation mapping and magnetic source imaging. J Neurosurg 107(3):488–494. doi:10.3171/JNS-07/09/0488
Bilginer B, Yalnizoglu D, Soylemezoglu F, Turanli G, Cila A, Topcu M, Akalan N (2009) Surgery for epilepsy in children with dysembryoplastic neuroepithelial tumor: clinical spectrum, seizure outcome, neuroradiology, and pathology. Child’s Nerv Syst ChNS : Off J Int Soc Pediatric Neurosurg 25(4):485–491. doi:10.1007/s00381-008-0762-x
Bills D, Rosenfeld JV, Phelan EM, Klug GL (1996) Intracranial arteriovenous malformations in childhood: presentation, management and outcome. J Clin Neurosci: Off J Neurosurg Soc Australas 3(3):220–228
Binder JR (2011) Functional MRI is a valid noninvasive alternative to Wada testing. Epilepsy Behav: E&B 20(2):214–222. doi:10.1016/j.yebeh.2010.08.004
Bingaman WE (2004) Surgery for focal cortical dysplasia. Neurology 62(6 Suppl 3):S30–34
Blumcke I (2009) Neuropathology of focal epilepsies: a critical review. Epilepsy Behav: E&B 15(1):34–39. doi:10.1016/j.yebeh.2009.02.033
Blumcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, Jacques TS, Avanzini G, Barkovich AJ, Battaglia G, Becker A, Cepeda C, Cendes F, Colombo N, Crino P, Cross JH, Delalande O, Dubeau F, Duncan J, Guerrini R, Kahane P, Mathern G, Najm I, Ozkara C, Raybaud C, Represa A, Roper SN, Salamon N, Schulze-Bonhage A, Tassi L, Vezzani A, Spreafico R (2011) The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc ask force of the ILAE Diagnostic Methods Commission. Epilepsia 52(1):158–174. doi:10.1111/j.1528-1167.2010.02777.x
Bordey A, Sontheimer H (1998) Properties of human glial cells associated with epileptic seizure foci. Epilepsy Res 32(1–2):286–303
Bourneville D (1880) Sclerose tubereuse des circonvolutions cerebrales: idiotie et epilepsie hemiplegique. Arch Neurol 1:81–91
Buckingham MJ, Crone KR, Ball WS, Berger TS (1989) Management of cerebral cavernous angiomas in children presenting with seizures. Childs Nerv Syst: ChNS : Off J Int Soc Pediatr Neurosurg 5(6):347–349
Buckner JC (2003) Factors influencing survival in high-grade gliomas. Semin Oncol 30(6 Suppl 19):10–14
Bujarski KA, Hirashima F, Roberts DW, Jobst BC, Gilbert KL, Roth RM, Flashman LA, McDonald BC, Saykin AJ, Scott RC, Dinnerstein E, Preston J, Williamson PD, Thadani VM (2013) Long-term seizure, cognitive, and psychiatric outcome following trans-middle temporal gyrus amygdalohippocampectomy and standard temporal lobectomy. J Neurosurg 119(1):16–23. doi:10.3171/2013.3.JNS12714
Carlson C, Teutonico F, Elliott RE, Moshel YA, LaJoie J, Miles D, Devinsky O, Weiner HL (2011) Bilateral invasive electroencephalography in patients with tuberous sclerosis complex: a path to surgery? J Neurosurg Pediatr 7(4):421–430. doi:10.3171/2011.1.PEDS10348
Chaichana KL, Parker SL, Olivi A, Quinones-Hinojosa A (2009) Long-term seizure outcomes in adult patients undergoing primary resection of malignant brain astrocytomas. Clinical article. J Neurosurg 111(2):282–292. doi:10.3171/2009.2.JNS081132
Chang EF, Christie C, Sullivan JE, Garcia PA, Tihan T, Gupta N, Berger MS, Barbaro NM (2010) Seizure control outcomes after resection of dysembryoplastic neuroepithelial tumor in 50 patients. J Neurosurg Pediatr 5(1):123–130. doi:10.3171/2009.8.PEDS09368
Chang EF, Clark A, Jensen RL, Bernstein M, Guha A, Carrabba G, Mukhopadhyay D, Kim W, Liau LM, Chang SM, Smith JS, Berger MS, McDermott MW (2009) Multiinstitutional validation of the University of California at San Francisco Low-Grade Glioma Prognostic Scoring System. J Neurosurg 111(2):203–210. doi:10.3171/2009.2.JNS081101
Chang EF, Clark A, Smith JS, Polley MY, Chang SM, Barbaro NM, Parsa AT, McDermott MW, Berger MS (2011) Functional mapping-guided resection of low-grade gliomas in eloquent areas of the brain: improvement of long-term survival. Clinical article. J Neurosurg 114(3):566–573. doi:10.3171/2010.6.JNS091246
Chang EF, Gabriel RA, Potts MB, Garcia PA, Barbaro NM, Lawton MT (2009) Seizure characteristics and control after microsurgical resection of supratentorial cerebral cavernous malformations. Neurosurgery 65(1):31–37. doi:10.1227/01, discussion 37–38
Chang EF, Nagarajan SS, Mantle M, Barbaro NM, Kirsch HE (2009) Magnetic source imaging for the surgical evaluation of electroencephalography-confirmed secondary bilateral synchrony in intractable epilepsy. J Neurosurg 111(6):1248–1256. doi:10.3171/2009.6.JNS081376
Chang EF, Potts MB, Keles GE, Lamborn KR, Chang SM, Barbaro NM, Berger MS (2008) Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg 108(2):227–235. doi:10.3171/JNS/2008/108/2/0227
Chang EF, Wang DD, Barkovich AJ, Tihan T, Auguste KI, Sullivan JE, Garcia PA, Barbaro NM (2011) Predictors of seizure freedom after surgery for malformations of cortical development. Ann Neurol 70(1):151–162. doi:10.1002/ana.22399
Choi H, Sell RL, Lenert L, Muennig P, Goodman RR, Gilliam FG, Wong JB (2008) Epilepsy surgery for pharmacoresistant temporal lobe epilepsy: a decision analysis. JAMA: J Am Med Assoc 300(21):2497–2505. doi:10.1001/jama.2008.771
Clusmann H, Kral T, Gleissner U, Sassen R, Urbach H, Blumcke I, Bogucki J, Schramm J (2004) Analysis of different types of resection for pediatric patients with temporal lobe epilepsy. Neurosurgery 54(4):847–859, discussion 859–860
Cohen-Gadol AA, Ozduman K, Bronen RA, Kim JH, Spencer DD (2004) Long-term outcome after epilepsy surgery for focal cortical dysplasia. J Neurosurg 101(1):55–65. doi:10.3171/jns.2004.101.1.0055
Cook SW, Nguyen ST, Hu B, Yudovin S, Shields WD, Vinters HV, Van de Wiele BM, Harrison RE, Mathern GW (2004) Cerebral hemispherectomy in pediatric patients with epilepsy: comparison of three techniques by pathological substrate in 115 patients. J Neurosurg 100(2 Suppl Pediatrics):125–141. doi:10.3171/ped.2004.100.2.0125
Couillard-Despres S, Winkler J, Uyanik G, Aigner L (2001) Molecular mechanisms of neuronal migration disorders, quo vadis? Curr Mol Med 1(6):677–688
Crawford PM, West CR, Shaw MD, Chadwick DW (1986) Cerebral arteriovenous malformations and epilepsy: factors in the development of epilepsy. Epilepsia 27(3):270–275
Crino PB, Nathanson KL, Henske EP (2006) The tuberous sclerosis complex. N Engl J Med 355(13):1345–1356. doi:10.1056/NEJMra055323
Cross JH, Jayakar P, Nordli D, Delalande O, Duchowny M, Wieser HG, Guerrini R, Mathern GW, International League against Epilepsy, Subcommission for Pediatric Epilepsy Surgery, Commissions of Neurosurgery and Paediatrics (2006) Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the Subcommission for Pediatric Epilepsy Surgery. Epilepsia 47(6):952–959. doi:10.1111/j.1528-1167.2006.00569.x
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fischbach AJ, Chang CH, Rotman M, Asbell SO, Krisch RE et al (1993) Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 85(9):704–710
Cusmai R, Chiron C, Curatolo P, Dulac O, Tran-Dinh S (1990) Topographic comparative study of magnetic resonance imaging and electroencephalography in 34 children with tuberous sclerosis. Epilepsia 31(6):747–755
Cyberonics I (2012) Cyberonics announces 100,000th patient implant of VNS therapy®. Accessed December 20, 2012
Dandy W (1928) Removal of right cerebral hemisphere for certain tumors with hemiplegia. JAMA: J Am Med Assoc 90:823–825
de Lanerolle NC, Lee TS, Spencer DD (2012) Histopathology of human epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. Bethesda, MD
DeAngelis LM (2001) Brain tumors. N Engl J Med 344(2):114–123. doi:10.1056/NEJM200101113440207
DeFazio RA, Hablitz JJ (2000) Alterations in NMDA receptors in a rat model of cortical dysplasia. J Neurophysiol 83(1):315–321
Devinsky O (2004) Diagnosis and treatment of temporal lobe epilepsy. Rev Neurol Dis 1(1):2–9
Di Rocco C, Battaglia D, Pietrini D, Piastra M, Massimi L (2006) Hemimegalencephaly: clinical implications and surgical treatment. Child’s Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 22(8):852–866. doi:10.1007/s00381-006-0149-9
Di Rocco C, Iannelli A (2000) Hemimegalencephaly and intractable epilepsy: complications of hemispherectomy and their correlations with the surgical technique. A report on 15 cases. Pediatr Neurosurg 33(4):198–207
Dimou S, Battisti RA, Hermens DF, Lagopoulos J (2013) A systematic review of functional magnetic resonance imaging and diffusion tensor imaging modalities used in presurgical planning of brain tumour resection. Neurosurg Rev 36(2):205–214. doi:10.1007/s10143-012-0436-8
Duffau H (2009) Surgery of low-grade gliomas: towards a ‘functional neurooncology’. Curr Opin Oncol 21(6):543–549. doi:10.1097/CCO.0b013e3283305996
Eisenschenk S, Gilmore RL, Friedman WA, Henchey RA (1998) The effect of LINAC stereotactic radiosurgery on epilepsy associated with arteriovenous malformations. Stereotact Funct Neurosurg 71(2):51–61
Elliott I, Kadis DS, Lach L, Olds J, McCleary L, Whiting S, Snyder T, Smith ML (2012) Quality of life in young adults who underwent resective surgery for epilepsy in childhood. Epilepsia 53(9):1577–1586. doi:10.1111/j.1528-1167.2012.03594.x
Ellis MJ, Kulkarni AV, Drake JM, Rutka JT, Armstrong D, Dirks PB (2010) Intraoperative angiography during microsurgical removal of arteriovenous malformations in children. J Neurosurg Pediatr 6(5):435–443. doi:10.3171/2010.8.PEDS10134
Engel J Jr (1987) Outcome with respect to epileptic seizures. In: Engel J Jr (ed) Surgical treatment of the epilepsies. Raven, New York, pp 553–571
Engel J Jr (1996) Surgery for seizures. N Engl J Med 334(10):647–652. doi:10.1056/NEJM199603073341008
Engel J Jr (2001) Finally, a randomized, controlled trial of epilepsy surgery. N Engl J Med 345(5):365–367. doi:10.1056/NEJM200108023450510
Engel J Jr (2008) Surgical treatment for epilepsy: too little, too late? JAMA: J Am Med Assoc 300(21):2548–2550. doi:10.1001/jama.2008.756
Engel J Jr, McDermott MP, Wiebe S, Langfitt JT, Stern JM, Dewar S, Sperling MR, Gardiner I, Erba G, Fried I, Jacobs M, Vinters HV, Mintzer S, Kieburtz K (2012) Early surgical therapy for drug-resistant temporal lobe epilepsy: a randomized trial. JAMA: J Am Med Assoc 307(9):922–930. doi:10.1001/jama.2012.220
Engel J Jr, Wiebe S (2012) Who is a surgical candidate? Handb Clin Neurol 108:821–828. doi:10.1016/B978-0-444-52899-5.00030-7
Engel J Jr, Wiebe S, French J, Sperling M, Williamson P, Spencer D, Gumnit R, Zahn C, Westbrook E, Enos B (2003) Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology 60(4):538–547
Engel J, Van Ness P, Rasmussen T, Ojemann L (1993) Outcome with respect to epileptic seizures. In: Engel J (ed) Surgical treatment of the epilepsies, 2nd edn. Raven, New York, pp 609–621
Engel J, Williamson PD (2007) Limbic seizures. In: Engel J, Pedley TA (eds) Epilepsy: a comprehensive textbook. Lippincott Williams & Wilkins, Philadelphia, pp 541–552
Englot DJ, Berger MS, Barbaro NM, Chang EF (2011) Predictors of seizure freedom after resection of supratentorial low-grade gliomas. A review. J Neurosurg 115(2):240–244. doi:10.3171/2011.3.JNS1153
Englot DJ, Berger MS, Chang EF, Garcia PA (2012) Characteristics and treatment of seizures in patients with high-grade glioma: a review. Neurosurg Clin N Am 23(2):227–235. doi:10.1016/j.nec.2012.01.009
Englot DJ, Blumenfeld H (2009) Consciousness and epilepsy: why are complex-partial seizures complex? Prog Brain Res 177:147–170. doi:10.1016/S0079-6123(09)17711-7
Englot DJ, Breshears JD, Sun PP, Chang EF, Auguste KI (2013) Seizure outcomes after resective surgery for extra-temporal lobe epilepsy in pediatric patients. J Neurosurg Pediatr 12(2):126–133. doi:10.3171/2013.5.PEDS1336
Englot DJ, Han SJ, Berger MS, Barbaro NM, Chang EF (2012) Extent of surgical resection predicts seizure freedom in low-grade temporal lobe brain tumors. Neurosurgery 70(4):921–928. doi:10.1227/NEU.0b013e31823c3a30, discussion 928
Englot DJ, Han SJ, Lawton MT, Chang EF (2011) Predictors of seizure freedom in the surgical treatment of supratentorial cavernous malformations. J Neurosurg 115(6):1169–1174. doi:10.3171/2011.7.JNS11536
Englot DJ, Lee AT, Tsai C, Halabi C, Barbaro NM, Auguste KI, Garcia PA, Chang EF (2013) Seizure types and frequency in patients who “fail” temporal lobectomy for intractable epilepsy. Neurosurgery 73(5):838–844. doi:10.1227/NEU.0000000000000120
Englot DJ, Ouyang D, Garcia PA, Barbaro NM, Chang EF (2012) Epilepsy surgery trends in the United States, 1990–2008. Neurology 78(16):1200–1206. doi:10.1212/WNL.0b013e318250d7ea
Englot DJ, Ouyang D, Wang DD, Rolston JD, Garcia PA, Chang EF (2013) Relationship between hospital surgical volume, lobectomy rates, and adverse perioperative events at US epilepsy centers. J Neurosurg 118(1):169–174. doi:10.3171/2012.9.JNS12776
Englot DJ, Rolston JD, Wang DD, Sun PP, Chang EF, Auguste KI (2013) Seizure outcomes after temporal lobectomy in pediatric patients. J Neurosurg Pediatr 12(2):134–141. doi:10.3171/2013.5.PEDS12526
Englot DJ, Rutkowski MJ, Ivan ME, Sun PP, Kuperman RA, Chang EF, Gupta N, Sullivan JE, Auguste KI (2013) Effects of temporal lobectomy on consciousness-impairing and consciousness-sparing seizures in children. Childs Nerv Syst ChNS: Off J Int Soc Pediatr Neurosurg 29(10):1915–1922. doi:10.1007/s00381-013-2168-7
Englot DJ, Wang DD, Rolston JD, Shih TT, Chang EF (2012) Rates and predictors of long-term seizure freedom after frontal lobe epilepsy surgery: a systematic review and meta-analysis. J Neurosurg 116(5):1042–1048. doi:10.3171/2012.1.JNS111620
Englot DJ, Yang L, Hamid H, Danielson N, Bai X, Marfeo A, Yu L, Gordon A, Purcaro MJ, Motelow JE, Agarwal R, Ellens DJ, Golomb JD, Shamy MC, Zhang H, Carlson C, Doyle W, Devinsky O, Vives K, Spencer DD, Spencer SS, Schevon C, Zaveri HP, Blumenfeld H (2010) Impaired consciousness in temporal lobe seizures: role of cortical slow activity. Brain J Neurol 133(Pt 12):3764–3777. doi:10.1093/brain/awq316
Englot DJ, Young WL, Han SJ, McCulloch CE, Chang EF, Lawton MT (2012) Seizure predictors and control after microsurgical resection of supratentorial arteriovenous malformations in 440 patients. Neurosurgery 71(3):572–580. doi:10.1227/NEU.0b013e31825ea3ba
Evans LT, Morse R, Roberts DW (2012) Epilepsy surgery in tuberous sclerosis: a review. Neurosurg Focus 32(3):E5. doi:10.3171/2012.1.FOCUS11330
Fallah A, Guyatt GH, Snead OC 3rd, Ebrahim S, Ibrahim GM, Mansouri A, Reddy D, Walter SD, Kulkarni AV, Bhandari M, Banfield L, Bhatnagar N, Liang S, Teutonico F, Liao J, Rutka JT (2013) Predictors of seizure outcomes in children with tuberous sclerosis complex and intractable epilepsy undergoing resective epilepsy surgery: an individual participant data meta-analysis. PloS One 8(2):e53565. doi:10.1371/journal.pone.0053565
FDA (2013) Device approvals and clearances. Accessed March 30, 2013
Ferrer I, Oliver B, Russi A, Casas R, Rivera R (1994) Parvalbumin and calbindin-D28k immunocytochemistry in human neocortical epileptic foci. J Neurolog Sci 123(1–2):18–25
Fish DR, Spencer SS (1995) Clinical correlations: MRI and EEG. Magn Reson Imaging 13(8):1113–1117
Flores-Sarnat L (2002) Hemimegalencephaly: part 1. Genetic, clinical, and imaging aspects. J Child Neurol 17(5):373–384, discussion 384
Fountas KN, Smith JR, Robinson JS, Tamburrini G, Pietrini D, Di Rocco C (2006) Anatomical hemispherectomy. Childs Nerv Syst ChNS: Off J Int Soc Pediatr Neurosurg 22(8):982–991. doi:10.1007/s00381-006-0135-2
French JA, Williamson PD, Thadani VM, Darcey TM, Mattson RH, Spencer SS, Spencer DD (1993) Characteristics of medial temporal lobe epilepsy: I. Results of history and physical examination. Ann Neurol 34(6):774–780. doi:10.1002/ana.410340604
Fried I, Kim JH, Spencer DD (1994) Limbic and neocortical gliomas associated with intractable seizures: a distinct clinicopathological group. Neurosurgery 34(5):815–823, discussion 823–814
Fullerton HJ, Achrol AS, Johnston SC, McCulloch CE, Higashida RT, Lawton MT, Sidney S, Young WL (2005) Long-term hemorrhage risk in children versus adults with brain arteriovenous malformations. Stroke 36(10):2099–2104. doi:10.1161/01.STR.0000181746.77149.2b
Gerszten PC, Adelson PD, Kondziolka D, Flickinger JC, Lunsford LD (1996) Seizure outcome in children treated for arteriovenous malformations using gamma knife radiosurgery. Pediatr Neurosurg 24(3):139–144
Gil-Nagel A, Abou-Khalil B (2012) Electroencephalography and video-electroencephalography. Handb Clin Neurol 107:323–345. doi:10.1016/B978-0-444-52898-8.00020-3 (edited by PJ Vinken and GW Bruyn)
Giulioni M, Galassi E, Zucchelli M, Volpi L (2005) Seizure outcome of lesionectomy in glioneuronal tumors associated with epilepsy in children. J Neurosurg 102(3 Suppl):288–293. doi:10.3171/ped.2005.102.3.0288
Giulioni M, Gardella E, Rubboli G, Roncaroli F, Zucchelli M, Bernardi B, Tassinari CA, Calbucci F (2006) Lesionectomy in epileptogenic gangliogliomas: seizure outcome and surgical results. J Clin Neurosci: Off J Neurosurg Soc Australas 13(5):529–535. doi:10.1016/j.jocn.2005.07.017
Giulioni M, Rubboli G, Marucci G, Martinoni M, Volpi L, Michelucci R, Marliani AF, Bisulli F, Tinuper P, Castana L, Sartori I, Calbucci F (2009) Seizure outcome of epilepsy surgery in focal epilepsies associated with temporomesial glioneuronal tumors: lesionectomy compared with tailored resection. J Neurosurg 111(6):1275–1282. doi:10.3171/2009.3.JNS081350
Glantz MJ, Cole BF, Forsyth PA, Recht LD, Wen PY, Chamberlain MC, Grossman SA, Cairncross JG (2000) Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 54(10):1886–1893
Goldstein LH, Polkey CE (1992) Behavioural memory after temporal lobectomy or amygdalo-hippocampectomy. Br J Clin Psychol/Br Psychol Soc 31(Pt 1):75–81
Goncalves-Ferreira A, Campos AR, Herculano-Carvalho M, Pimentel J, Bentes C, Peralta AR, Morgado C (2013) Amygdalohippocampotomy: surgical technique and clinical results. J Neurosurg 118(5):1107–1113. doi:10.3171/2013.1.JNS12727
Gonzalez-Martinez JA, Gupta A, Kotagal P, Lachhwani D, Wyllie E, Luders HO, Bingaman WE (2005) Hemispherectomy for catastrophic epilepsy in infants. Epilepsia 46(9):1518–1525. doi:10.1111/j.1528-1167.2005.53704.x
Goodman M, Lamm SH, Engel A, Shepherd CW, Houser OW, Gomez MR (1997) Cortical tuber count: a biomarker indicating neurologic severity of tuberous sclerosis complex. J Child Neurol 12(2):85–90
Haglund MM, Berger MS, Kunkel DD, Franck JE, Ghatan S, Ojemann GA (1992) Changes in gamma-aminobutyric acid and somatostatin in epileptic cortex associated with low-grade gliomas. J Neurosurg 77(2):209–216. doi:10.3171/jns.1992.77.2.0209
Hammen T, Romstock J, Dorfler A, Kerling F, Buchfelder M, Stefan H (2007) Prediction of postoperative outcome with special respect to removal of hemosiderin fringe: a study in patients with cavernous haemangiomas associated with symptomatic epilepsy. Seizure: J Br Epilepsy Assoc 16(3):248–253. doi:10.1016/j.seizure.2007.01.001
Haneef Z, Stern J, Dewar S, Engel J Jr (2010) Referral pattern for epilepsy surgery after evidence-based recommendations: a retrospective study. Neurology 75(8):699–704. doi:10.1212/WNL.0b013e3181eee457
Hauptman JS, Mathern GW (2012) Surgical treatment of epilepsy associated with cortical dysplasia: 2012 update. Epilepsia 53(Suppl 4):98–104. doi:10.1111/j.1528-1167.2012.03619.x
Heikkinen ER, Konnov B, Melnikov L, Yalynych N, Zubkov Yu N, Garmashov Yu A, Pak VA (1989) Relief of epilepsy by radiosurgery of cerebral arteriovenous malformations. Stereotact Funct Neurosurg 53(3):157–166
Helmstaedter C, Kockelmann E (2006) Cognitive outcomes in patients with chronic temporal lobe epilepsy. Epilepsia 47(Suppl 2):96–98. doi:10.1111/j.1528-1167.2006.00702.x
Herman ST (2002) Epilepsy after brain insult: targeting epileptogenesis. Neurology 59(9 Suppl 5):S21–26
Heros RC, Korosue K, Diebold PM (1990) Surgical excision of cerebral arteriovenous malformations: late results. Neurosurgery 26(4):570–577, discussion 577–578
Hilbig A, Babb TL, Najm I, Ying Z, Wyllie E, Bingaman W (1999) Focal cortical dysplasia in children. Dev Neurosci 21(3–5):271–280
Hogan RE, Kaiboriboon K (2003) The “dreamy state”: John Hughlings-Jackson’s ideas of epilepsy and consciousness. Am J Psychiatry 160(10):1740–1747
Hoh BL, Chapman PH, Loeffler JS, Carter BS, Ogilvy CS (2002) Results of multimodality treatment for 141 patients with brain arteriovenous malformations and seizures: factors associated with seizure incidence and seizure outcomes. Neurosurgery 51(2):303–309, discussion 309–311
Hughlings-Jackson J, Stewart J (1899) Epileptic attacks with a warning of a crude sensation of smell and with the intellectual aura (dreamy state) in a patient who had symptoms pointing to gross organic disease of the right temporo-sphenoidal lobe. Brain J Neurol 22:534–543
Jackson GD, Badawy RA (2011) Selecting patients for epilepsy surgery: identifying a structural lesion. Epilepsy Behav: E&B 20(2):182–189. doi:10.1016/j.yebeh.2010.09.019
Jansen FE, Huiskamp G, van Huffelen AC, Bourez-Swart M, Boere E, Gebbink T, Vincken KL, van Nieuwenhuizen O (2006) Identification of the epileptogenic tuber in patients with tuberous sclerosis: a comparison of high-resolution EEG and MEG. Epilepsia 47(1):108–114. doi:10.1111/j.1528-1167.2006.00373.x
Jansen FE, van Huffelen AC, Algra A, van Nieuwenhuizen O (2007) Epilepsy surgery in tuberous sclerosis: a systematic review. Epilepsia 48(8):1477–1484. doi:10.1111/j.1528-1167.2007.01117.x
Janszky J, Ebner A, Kruse B, Mertens M, Jokeit H, Seitz RJ, Witte OW, Tuxhorn I, Woermann FG (2003) Functional organization of the brain with malformations of cortical development. Ann Neurol 53(6):759–767. doi:10.1002/ana.10545
Jonas R, Nguyen S, Hu B, Asarnow RF, LoPresti C, Curtiss S, de Bode S, Yudovin S, Shields WD, Vinters HV, Mathern GW (2004) Cerebral hemispherectomy: hospital course, seizure, developmental, language, and motor outcomes. Neurology 62(10):1712–1721
Jooma R, Yeh HS, Privitera MD, Gartner M (1995) Lesionectomy versus electrophysiologically guided resection for temporal lobe tumors manifesting with complex partial seizures. J Neurosurg 83(2):231–236. doi:10.3171/jns.1995.83.2.0231
Josephson CB, Leach JP, Duncan R, Roberts RC, Counsell CE, Al-Shahi Salman R, Scottish Audit of Intracranial Vascular Malformations (SAIVMs) Steering Committee and Collaborators (2011) Seizure risk from cavernous or arteriovenous malformations: prospective population-based study. Neurology 76(18):1548–1554. doi:10.1212/WNL.0b013e3182190f37
Kim JH, Guimaraes PO, Shen MY, Masukawa LM, Spencer DD (1990) Hippocampal neuronal density in temporal lobe epilepsy with and without gliomas. Acta Neuropathol 80(1):41–45
Kingwell K (2012) Epilepsy: surgical therapy should not be considered a last resort for pharmacoresistant epilepsy. Nat Rev Neurol 8(5):238. doi:10.1038/nrneurol.2012.55
Klein M, Engelberts NH, van der Ploeg HM, Kasteleijn-Nolst Trenite DG, Aaronson NK, Taphoorn MJ, Baaijen H, Vandertop WP, Muller M, Postma TJ, Heimans JJ (2003) Epilepsy in low-grade gliomas: the impact on cognitive function and quality of life. Ann Neurol 54(4):514–520. doi:10.1002/ana.10712
Kobayashi K, Ohtsuka Y, Ohno S, Ohmori I, Ogino T, Yoshinaga H, Tanaka A, Hiraki Y, Oka E (2001) Clinical spectrum of epileptic spasms associated with cortical malformation. Neuropediatrics 32(5):236–244. doi:10.1055/s-2001-19117
Kondziolka D, Humphreys RP, Hoffman HJ, Hendrick EB, Drake JM (1992) Arteriovenous malformations of the brain in children: a forty year experience. Can J Neurol Sci 19(1):40–45
Kondziolka D, Lunsford LD, Kestle JR (1995) The natural history of cerebral cavernous malformations. J Neurosurg 83(5):820–824. doi:10.3171/jns.1995.83.5.0820
Kraemer DL, Awad IA (1994) Vascular malformations and epilepsy: clinical considerations and basic mechanisms. Epilepsia 35(Suppl 6):S30–43
Kwan P, Brodie MJ (2000) Early identification of refractory epilepsy. N Engl J Med 342(5):314–319. doi:10.1056/NEJM200002033420503
Kwan P, Sperling MR (2009) Refractory seizures: try additional antiepileptic drugs (after two have failed) or go directly to early surgery evaluation? Epilepsia 50(Suppl 8):57–62. doi:10.1111/j.1528-1167.2009.02237.x
Labiner DM, Bagic AI, Herman ST, Fountain NB, Walczak TS, Gumnit RJ, National Association of Epilepsy C (2010) Essential services, personnel, and facilities in specialized epilepsy centers—revised 2010 guidelines. Epilepsia 51(11):2322–2333. doi:10.1111/j.1528-1167.2010.02648.x
Leblanc R, Feindel W, Ethier R (1983) Epilepsy from cerebral arteriovenous malformations. Can J Neurol Sci 10(2):91–95
Leventer RJ, Guerrini R, Dobyns WB (2008) Malformations of cortical development and epilepsy. Dialogues Clin Neurosci 10(1):47–62
Luyken C, Blumcke I, Fimmers R, Urbach H, Elger CE, Wiestler OD, Schramm J (2003) The spectrum of long-term epilepsy-associated tumors: long-term seizure and tumor outcome and neurosurgical aspects. Epilepsia 44(6):822–830
Macrodimitris S, Sherman EM, Williams TS, Bigras C, Wiebe S (2011) Measuring patient satisfaction following epilepsy surgery. Epilepsia 52(8):1409–1417. doi:10.1111/j.1528-1167.2011.03160.x
Marcotte L, Crino PB (2006) The neurobiology of the tuberous sclerosis complex. Neuromol Med 8(4):531–546. doi:10.1385/NMM:8:4:531
Martino J, Honma SM, Findlay AM, Guggisberg AG, Owen JP, Kirsch HE, Berger MS, Nagarajan SS (2011) Resting functional connectivity in patients with brain tumors in eloquent areas. Ann Neurol 69(3):521–532. doi:10.1002/ana.22167
McKenzie K (1938) The present status of a patient who had the right cerebral hemisphere removed. JAMA: J Am Med Assoc 111:168
Mengesha T, Abu-Ata M, Haas KF, Lavin PJ, Sun DA, Konrad PE, Pearson M, Wang L, Song Y, Abou-Khalil BW (2009) Visual field defects after selective amygdalohippocampectomy and standard temporal lobectomy. J NeuroOphthalmol: Off J N American NeuroOphthalmol Soc 29(3):208–213. doi:10.1097/WNO.0b013e3181b41262
Milandre L, Pellissier JF, Boudouresques G, Bonnefoi B, Ali Cherif A, Khalil R (1987) Non-hereditary multiple telangiectasias of the central nervous system. Report of two clinicopathological cases. J Neurol Sci 82(1–3):291–304
Moosa AN, Gupta A, Jehi L, Marashly A, Cosmo G, Lachhwani D, Wyllie E, Kotagal P, Bingaman W (2013) Longitudinal seizure outcome and prognostic predictors after hemispherectomy in 170 children. Neurology 80(3):253–260. doi:10.1212/WNL.0b013e31827dead9
Moots PL, Maciunas RJ, Eisert DR, Parker RA, Laporte K, Abou-Khalil B (1995) The course of seizure disorders in patients with malignant gliomas. Arch Neurol 52(7):717–724
Moran NF, Fish DR, Kitchen N, Shorvon S, Kendall BE, Stevens JM (1999) Supratentorial cavernous haemangiomas and epilepsy: a review of the literature and case series. J Neurol Neurosurg Psychiatry 66(5):561–568
Moreno A, de Felipe J, Garcia Sola R, Navarro A, Ramon y Cajal S (2001) Neuronal and mixed neuronal glial tumors associated to epilepsy. A heterogeneous and related group of tumours. Histol Histopathol 16(2):613–622
Morino M, Uda T, Naito K, Yoshimura M, Ishibashi K, Goto T, Ohata K, Hara M (2006) Comparison of neuropsychological outcomes after selective amygdalohippocampectomy versus anterior temporal lobectomy. Epilepsy Behav: E&B 9(1):95–100. doi:10.1016/j.yebeh.2006.04.017
Murphy MJ (1985) Long-term follow-up of seizures associated with cerebral arteriovenous malformations. Results of therapy. Arch Neurol 42(5):477–479
Nagata S, Morioka T, Matsukado K, Natori Y, Sasaki T (2006) Retrospective analysis of the surgically treated temporal lobe arteriovenous malformations with focus on the visual field defects and epilepsy. Surg Neurol 66(1):50–55. doi:10.1016/j.surneu.2005.12.017, discussion 55
Nakaji P, Spetzler RF (2005) Indications for surgical treatment of arteriovenous malformations. Neurosurg Clin N Am 16(2):365–366. doi:10.1016/j.nec.2004.08.016
O'Brien DF, Basu S, Williams DH, May PL (2006) Anatomical hemispherectomy for intractable seizures: excellent seizure control, low morbidity and no superficial cerebral haemosiderosis. Childs Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 22(5):489–498. doi:10.1007/s00381-005-0023-1, discussion 499
O'Brien DF, Farrell M, Delanty N, Traunecker H, Perrin R, Smyth MD, Park TS (2007) The Children’s Cancer and Leukaemia Group guidelines for the diagnosis and management of dysembryoplastic neuroepithelial tumours. Br J Neurosurg 21(6):539–549. doi:10.1080/02688690701594817
Ogiwara H, Nordli DR, DiPatri AJ, Alden TD, Bowman RM, Tomita T (2010) Pediatric epileptogenic gangliogliomas: seizure outcome and surgical results. J Neurosurg Pediatr 5(3):271–276. doi:10.3171/2009.10.PEDS09372
Ojemann RG, Ogilvy CS (1999) Microsurgical treatment of supratentorial cavernous malformations. Neurosurg Clin N Am 10(3):433–440
Ondra SL, Troupp H, George ED, Schwab K (1990) The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg 73(3):387–391. doi:10.3171/jns.1990.73.3.0387
Palmini A, Najm I, Avanzini G, Babb T, Guerrini R, Foldvary-Schaefer N, Jackson G, Luders HO, Prayson R, Spreafico R, Vinters HV (2004) Terminology and classification of the cortical dysplasias. Neurology 62(6 Suppl 3):S2–8
Park YS, Kim DS, Shim KW, Kim JH, Choi JU (2008) Factors contributing to resectability and seizure outcomes in 44 patients with ganglioglioma. Clin Neurol Neurosurg 110(7):667–673. doi:10.1016/j.clineuro.2008.03.017
Parrent AG, Blume WT (1999) Stereotactic amygdalohippocampotomy for the treatment of medial temporal lobe epilepsy. Epilepsia 40(10):1408–1416
Pasquier B, Peoc HM, Fabre-Bocquentin B, Bensaadi L, Pasquier D, Hoffmann D, Kahane P, Tassi L, Le Bas JF, Benabid AL (2002) Surgical pathology of drug-resistant partial epilepsy. A 10-year-experience with a series of 327 consecutive resections. Epileptic Disord 4(2):99–119
Phi JH, Chung CK (2009) Brain tumors in the mesial temporal lobe: long-term oncological outcome. Neurosurg Focus 27(2):E5. doi:10.3171/2009.5.FOCUS09106
Phi JH, Kim SK, Cho BK, Lee SY, Park SY, Park SJ, Lee SK, Kim KJ, Chung CK (2009) Long-term surgical outcomes of temporal lobe epilepsy associated with low-grade brain tumors. Cancer 115(24):5771–5779. doi:10.1002/cncr.24666
Piepgras DG, Sundt TM Jr, Ragoowansi AT, Stevens L (1993) Seizure outcome in patients with surgically treated cerebral arteriovenous malformations. J Neurosurg 78(1):5–11. doi:10.3171/jns.1993.78.1.0005
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P, Afra D, Cornu P, Bolla M, Vecht C, Karim AB, European Organization for R, Treatment of Cancer Brain Tumor Cooperative G, European Organization for R, Treatment of Cancer Radiotherapy Cooperative G (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol: Off J Am Soc Clin Oncol 20(8):2076–2084
Rasmussen T (1973) Postoperative superficial hemosiderosis of the brain, its diagnosis, treatment and prevention. Trans Am Neurol Assoc 98:133–137
Recht L, Glantz M (2008) Neoplastic diseases. In: Engel J Jr, Pedley T (eds) Epilepsy: a comprehensive textbook. Lippincott, Williams, and Wilkins, New York, pp 2637–2642
Ritaccio A, Beauchamp M, Bosman C, Brunner P, Chang E, Crone N, Gunduz A, Gupta D, Knight R, Leuthardt E, Litt B, Moran D, Ojemann J, Parvizi J, Ramsey N, Rieger J, Viventi J, Voytek B, Williams J, Schalk G (2012) Proceedings of the Third International Workshop on Advances in Electrocorticography. Epilepsy Behav: E&B 25(4):605–613. doi:10.1016/j.yebeh.2012.09.016
Robinson JR, Awad IA, Little JR (1991) Natural history of the cavernous angioma. J Neurosurg 75(5):709–714. doi:10.3171/jns.1991.75.5.0709
Robinson JR Jr, Awad IA, Masaryk TJ, Estes ML (1993) Pathological heterogeneity of angiographically occult vascular malformations of the brain. Neurosurgery 33(4):547–554, discussion 554–545
Romanelli P, Weiner HL, Najjar S, Devinsky O (2001) Bilateral resective epilepsy surgery in a child with tuberous sclerosis: case report. Neurosurgery 49(3):732–734, discussion 735
Roper SN (2009) Surgical treatment of the extratemporal epilepsies. Epilepsia 50(Suppl 8):69–74. doi:10.1111/j.1528-1167.2009.02239.x
Rosati A, Marconi S, Pollo B, Tomassini A, Lovato L, Maderna E, Maier K, Schwartz A, Rizzuto N, Padovani A, Bonetti B (2009) Epilepsy in glioblastoma multiforme: correlation with glutamine synthetase levels. J Neurooncol 93(3):319–324. doi:10.1007/s11060-008-9794-z
Ross J, Al-Shahi Salman R (2010) Interventions for treating brain arteriovenous malformations in adults. Cochrane Database Syst Rev 7:CD003436. doi:10.1002/14651858.CD003436.pub3
Rowland NC, Englot DJ, Cage TA, Sughrue ME, Barbaro NM, Chang EF (2012) A meta-analysis of predictors of seizure freedom in the surgical management of focal cortical dysplasia. J Neurosurg 116(5):1035–1041. doi:10.3171/2012.1.JNS111105
Ruda R, Trevisan E, Soffietti R (2010) Epilepsy and brain tumors. Curr Opin Oncol 22(6):611–620. doi:10.1097/CCO.0b013e32833de99d
Ryvlin P, Mauguiere F, Sindou M, Froment JC, Cinotti L (1995) Interictal cerebral metabolism and epilepsy in cavernous angiomas. Brain: J Neurol 118(Pt 3):677–687
Sanai N, Mirzadeh Z, Berger MS (2008) Functional outcome after language mapping for glioma resection. N Engl J Med 358(1):18–27. doi:10.1056/NEJMoa067819
Scheidegger O, Wiest R, Jann K, Konig T, Meyer K, Hauf M (2013) Epileptogenic developmental venous anomaly: insights from simultaneous EEG/fMRI. Clin EEG Neurosci 44(2):157–160. doi:10.1177/1550059412464463
Schiltz NK, Koroukian SM, Lhatoo SD, Kaiboriboon K (2013) Temporal trends in pre-surgical evaluations and epilepsy surgery in the U.S. from 1998 to 2009. Epilepsy Res 103(2–3):270–278. doi:10.1016/j.eplepsyres.2012.07.016
Schomer DL, Lewis RJ (2012) Stopping seizures early and the surgical epilepsy trial that stopped even earlier. JAMA: J Am Med Assoc 307(9):966–968. doi:10.1001/jama.2012.251
Schramm J (2008) Temporal lobe epilepsy surgery and the quest for optimal extent of resection: a review. Epilepsia 49(8):1296–1307. doi:10.1111/j.1528-1167.2008.01604.x
Schramm J, Kuczaty S, Sassen R, Elger CE, von Lehe M (2012) Pediatric functional hemispherectomy: outcome in 92 patients. Acta Neurochir (Wien) 154(11):2017–2028. doi:10.1007/s00701-012-1481-3
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003. doi:10.1016/S1470-2045(11)70196-6
Shamji MF, Fric-Shamji EC, Benoit BG (2009) Brain tumors and epilepsy: pathophysiology of peritumoral changes. Neurosurg Rev 32(3):275–284. doi:10.1007/s10143-009-0191-7, discussion 284–276
Sheth RD (2002) Adolescent issues in epilepsy. J Child Neurol 17(Suppl 2):2S23–22S27
Sims J (1835) On the hypertrophy and atrophy of the brain. Medicochirurgical Trans R Med Chir Soc (London) 19:315–380
Southwell DG, Garcia PA, Berger MS, Barbaro NM, Chang EF (2012) Long-term seizure control outcomes after resection of gangliogliomas. Neurosurgery 70(6):1406–1413. doi:10.1227/NEU.0b013e3182500a4c, discussion 1413–1404
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7(6):525–537. doi:10.1016/S1474-4422(08)70109-1
Spreafico R, Tassi L, Colombo N, Bramerio M, Galli C, Garbelli R, Ferrario A, Lo Russo G, Munari C (2000) Inhibitory circuits in human dysplastic tissue. Epilepsia 41(Suppl 6):S168–173
Stavrou I, Baumgartner C, Frischer JM, Trattnig S, Knosp E (2008) Long-term seizure control after resection of supratentorial cavernomas: a retrospective single-center study in 53 patients. Neurosurgery 63(5):888–896. doi:10.1227/01.NEU.0000327881.72964.6E, discussion 897
Tang SC, Jeng JS, Liu HM, Yip PK (2003) Diffuse capillary telangiectasia of the brain manifested as a slowly progressive course. Cerebrovasc Dis 15(1–2):140–142
Taphoorn MJ (2003) Neurocognitive sequelae in the treatment of low-grade gliomas. Semin Oncol 30(6 Suppl 19):45–48
Taphoorn MJ, Klein M (2004) Cognitive deficits in adult patients with brain tumours. Lancet Neurol 3(3):159–168. doi:10.1016/S1474-4422(04)00680-5
Thapa A, Chandra PS, Sinha S, Gupta A, Singh M, Suri A, Sharma BS (2009) Surgical interventions in intracranial arteriovenous malformations: indications and outcome analysis in a changing scenario. Neurol India 57(6):749–755. doi:10.4103/0028-3886.59471
Thom M (2009) Hippocampal sclerosis: progress since Sommer. Brain Pathol 19(4):565–572. doi:10.1111/j.1750-3639.2008.00201.x
Thom M, Mathern GW, Cross JH, Bertram EH (2010) Mesial temporal lobe epilepsy: how do we improve surgical outcome? Ann Neurol 68(4):424–434. doi:10.1002/ana.22142
Thorpe ML, Cordato DJ, Morgan MK, Herkes GK (2000) Postoperative seizure outcome in a series of 114 patients with supratentorial arteriovenous malformations. J Clin Neurosci: Off J Neurosurg Soc Australas 7(2):107–111. doi:10.1054/jocn.1999.0159
Thudium MO, Campos AR, Urbach H, Clusmann H (2010) The basal temporal approach for mesial temporal surgery: sparing the Meyer loop with navigated diffusion tensor tractography. Neurosurgery 67(2 Suppl Operative):385–390. doi:10.1227/NEU.0b013e3181f7424b
Tinkle BT, Schorry EK, Franz DN, Crone KR, Saal HM (2005) Epidemiology of hemimegalencephaly: a case series and review. Am J Med Genet A 139(3):204–211. doi:10.1002/ajmg.a.31024
Tonini C, Beghi E, Berg AT, Bogliun G, Giordano L, Newton RW, Tetto A, Vitelli E, Vitezic D, Wiebe S (2004) Predictors of epilepsy surgery outcome: a meta-analysis. Epilepsy Res 62(1):75–87. doi:10.1016/j.eplepsyres.2004.08.006
Villanueva V, Codina M, Elices E (2008) Management of epilepsy in oncological patients. Neurologist 14(6 Suppl 1):S44–54. doi:10.1097/01.nrl.0000340791.53413.f4
von Essen C, Rydenhag B, Nystrom B, Mozzi R, van Gelder N, Hamberger A (1996) High levels of glycine and serine as a cause of the seizure symptoms of cavernous angiomas? J Neurochem 67(1):260–264
Wachi M, Tomikawa M, Fukuda M, Kameyama S, Kasahara K, Sasagawa M, Shirane S, Kanazawa O, Yoshino M, Aoki S, Sohma Y (2001) Neuropsychological changes after surgical treatment for temporal lobe epilepsy. Epilepsia 42(Suppl 6):4–8
Wang DD, Deans AE, Barkovich AJ, Tihan T, Barbaro NM, Garcia PA, Chang EF (2013) Transmantle sign in focal cortical dysplasia: a unique radiological entity with excellent prognosis for seizure control. J Neurosurg 118(2):337–344. doi:10.3171/2012.10.JNS12119
Wang VY, Chang EF, Barbaro NM (2006) Focal cortical dysplasia: a review of pathological features, genetics, and surgical outcome. Neurosurg Focus 20(1):E7
Washington CW, McCoy KE, Zipfel GJ (2010) Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurgical Focus 29(3):E7. doi:10.3171/2010.5.FOCUS10149
Westerveld M, Sass KJ, Chelune GJ, Hermann BP, Barr WB, Loring DW, Strauss E, Trenerry MR, Perrine K, Spencer DD (2000) Temporal lobectomy in children: cognitive outcome. J Neurosurg 92(1):24–30. doi:10.3171/jns.2000.92.1.0024
Westmoreland B (1999) The electroencephalogram in tuberous sclerosis. In: Rodriguez-Gomez M, Sampson J, Whittemore V (eds) Tubrous sclerosis complex: developmental perspectives in psychiatry, 3rd edn. Oxford University Press, New York, pp 63–73
White JC, Liu CT, Mixter WJ (1948) Focal epilepsy; a statistical study of its causes and the results of surgical treatment; epilepsy secondary to intracranial tumors. N Engl J Med 238(26):891–899. doi:10.1056/NEJM194806242382601
White R, Hua Y, Scheithauer B, Lynch DR, Henske EP, Crino PB (2001) Selective alterations in glutamate and GABA receptor subunit mRNA expression in dysplastic neurons and giant cells of cortical tubers. Ann Neurol 49(1):67–78
Wiebe S (2004) Effectiveness and safety of epilepsy surgery: what is the evidence? CNS Spectr 9(2):120–122, 126–132
Wiebe S, Berg AT (2013) Big epilepsy surgery for little people: what’s the full story on hemispherectomy? Neurology 80(3):232–233. doi:10.1212/WNL.0b013e31827dec32
Wiebe S, Blume WT, Girvin JP, Eliasziw M (2001) A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 345(5):311–318. doi:10.1056/NEJM200108023450501
Wilkins RH (1985) Natural history of intracranial vascular malformations: a review. Neurosurgery 16(3):421–430
Williamson A, Patrylo PR, Lee S, Spencer DD (2003) Physiology of human cortical neurons adjacent to cavernous malformations and tumors. Epilepsia 44(11):1413–1419
Wilson SJ, Engel J Jr (2010) Diverse perspectives on developments in epilepsy surgery. Seizure: J Br Epilepsy Assoc 19(10):659–668. doi:10.1016/j.seizure.2010.10.028
Wolf HK, Roos D, Blumcke I, Pietsch T, Wiestler OD (1996) Perilesional neurochemical changes in focal epilepsies. Acta Neuropathol 91(4):376–384
Wolf RL, Ivnik RJ, Hirschorn KA, Sharbrough FW, Cascino GD, Marsh WR (1993) Neurocognitive efficiency following left temporal lobectomy: standard versus limited resection. J Neurosurg 79(1):76–83. doi:10.3171/jns.1993.79.1.0076
Wong M, Ess KC, Uhlmann EJ, Jansen LA, Li W, Crino PB, Mennerick S, Yamada KA, Gutmann DH (2003) Impaired glial glutamate transport in a mouse tuberous sclerosis epilepsy model. Ann Neurol 54(2):251–256. doi:10.1002/ana.10648
Yang I, Chang EF, Han SJ, Barry JJ, Fang S, Tihan T, Barbaro NM, Parsa AT (2011) Early surgical intervention in adult patients with ganglioglioma is associated with improved clinical seizure outcomes. J Clin Neurosci: Off J Neurosurg Soc Australas 18(1):29–33. doi:10.1016/j.jocn.2010.05.002
Yasargil MG, Krayenbuhl N, Roth P, Hsu SP, Yasargil DC (2010) The selective amygdalohippocampectomy for intractable temporal limbic seizures. J Neurosurg 112(1):168–185. doi:10.3171/2008.12.JNS081112
Yeh HS, Privitera MD (1991) Secondary epileptogenesis in cerebral arteriovenous malformations. Arch Neurol 48(11):1122–1124
Yeh HS, Tew JM Jr, Gartner M (1993) Seizure control after surgery on cerebral arteriovenous malformations. J Neurosurg 78(1):12–18. doi:10.3171/jns.1993.78.1.0012
Yeon JY, Kim JS, Choi SJ, Seo DW, Hong SB, Hong SC (2009) Supratentorial cavernous angiomas presenting with seizures: surgical outcomes in 60 consecutive patients. Seizure: J Br Epilepsy Assoc 18(1):14–20. doi:10.1016/j.seizure.2008.05.010
You G, Sha ZY, Yan W, Zhang W, Wang YZ, Li SW, Sang L, Wang Z, Li GL, Li SW, Song YJ, Kang CS, Jiang T (2012) Seizure characteristics and outcomes in 508 Chinese adult patients undergoing primary resection of low-grade gliomas: a clinicopathological study. Neuro-oncology 14(2):230–241. doi:10.1093/neuonc/nor205
Yuan J, Chen Y, Hirsch E (2012) Intracranial electrodes in the presurgical evaluation of epilepsy. Neurol Sci 33(4):723–729. doi:10.1007/s10072-012-1020-2
Zaatreh MM, Firlik KS, Spencer DD, Spencer SS (2003) Temporal lobe tumoral epilepsy: characteristics and predictors of surgical outcome. Neurology 61(5):636–641
Zevgaridis D, van Velthoven V, Ebeling U, Reulen HJ (1996) Seizure control following surgery in supratentorial cavernous malformations: a retrospective study in 77 patients. Acta Neurochir (Wien) 138(6):672–677
Acknowledgement
We would like to thank the practitioners of the UCSF Comprehensive Epilepsy Center for their tireless dedication to the patients and to advancing care.
Disclosures
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Hartmut Vatter and Christian E. Elger, Bonn, Germany
Recently, convincing data by Engel et al. are available, which demonstrate the superiority of early resective epilepsy surgery compared with conservative treatment. Accordingly, the recommendations of the International League against Epilepsy and several national neurological societies are supporting an earlier referral of patients with drug-resistant epilepsy in high-volume centers for pre-surgical evaluation and, if suitable, for epilepsy surgery. In spite of these recommendations, neither the number of referrals to specialized centers nor the number of epilepsy surgery increased significantly.
Therefore, this excellent review article by Englot and Chang is hopefully a sufficient instrument to support the operative treatment of epilepsy in specialized centers. The authors report in a concise form about the essential literature, the recent data, and their own experience as a “high-volume center” for resective epilepsy surgery. The review is clearly structured in the most important morphological changes underlying epilepsy. The expected rates of seizure reduction/freedom and the outcome predictors are clearly given in tables for each etiology.
Some important topics could be even more emphasized. The first is the impressing development of the pre-surgical diagnostic opportunities including functional neuroimaging, white matter tractography, and further sophisticated MRI sequences. These methods will more and more precisely define potential epileptic brain areas in correlation with eloquent cortex areas and tracts. The proof of the epilepsy origin of such areas could significantly be improved by the development of invasive electrophysiological investigations, which enable measurements even on a single-cell level. The accurate placement of these probes and the following observation is, however, standard in any specialized epilepsy center. Another significant development is the possibility of an accurate control of the resection of the pre- and/or intraoperatively defined brain tissue by intraoperative MRI. The inclusion of these new developments in the standardized pre- and intra-surgical workup will facilitate specialized centers to perform epilepsy surgery as a well-tailored lesionectomy, in which the personal facilities of the patient, the burden of the seizures, and the etiology of the epilepsy could be taken into account, comparably.
These topics may be added to further support the educational character of this excellent article and to improve the ranking of invasive diagnostic and surgical treatment of drug-resistant epilepsy.
Karl Schaller, Geneva, Switzerland
The present review is coming from one of the most eminent North American epilepsy surgical centers. The authors have outlined the present state of knowledge on epidemiology, underlying pathology and diagnosis of epilepsy on the one hand, and on the presently available options of resective epilepsy surgical procedures and on its potential benefits and outcomes. They have to be commended for the important and comprehensive work they have done in that regard; without doubt, this review will serve as a standard reference on the matter for years to come. As they had restricted themselves to an analysis of the body of literature in the field of resective epilepsy surgery, it is tempting for a commentator to provide some further reflections on the concept of epilepsy surgery as a whole. Epilepsy surgery may have a high socioeconomic impact because there is proof that the mortality rate of epileptics is clearly elevated when compared with person-years of an age-matched control population.
I do fully agree with the authors that, given the right indication, neurosurgical interventions in pediatric epilepsy may improve or normalize the psychomotor development. Concerning the pathogenesis of temporal epilepsy, I would like to add that there is evidence that the particular ontogenetic zytoarchitectonics of the temporal lobe may in part be held responsible for epileptogenesis. This concerns the mesocortical regions, which are connecting the lateral isocortex with the mesial temporal lobe and the limbic system in particular. Thus, it is presumed that this specific zytoarchitecture may facilitate the occurrence of malformations of cortical development and the scattering of ectopic neurons with epileptogenic potential on the one side and the genesis and growth of intrinsic and long-term epilepsy-associated tumors on the other side. These neuropathological specifics in temporal epilepsy seem to be contributive to better long-term epileptological outcome following additional temporo-polar resection in pediatric temporal lobe epilepsy, when compared with the results of more selective temporo-mesial resection. This may be due to the presence of ectopic neurons in the temporal pole of epileptic children, whereas in adult temporal lobe epilepsy, mesio-temporal sclerosis plays a by far more important role. The seizure freeness rates in adults do not differ between standard anterior temporal lobectomies and more selective temporo-mesial approaches, as has been highlighted by the authors
Epilepsy surgery can be considered an asset and a luxury for a given society. This is reflected by the fact that there are important variations between societies with different socioeconomic status with regard to the existence of epilepsy surgical centres. This may even differ from state to state and with the insurance status of the affected population, according to recent North American comparative studies. It is a subspecialty, which is embedded in the setting of pluridisciplinary evaluation and research, which requires important financial funding, and the surgical partner cannot function on his own in a proper way. Only the close cooperation between clinicians, epileptologists, neurosurgeons, neuropsychologists, and neuroradiologists, together with fundamental neuroscientists and signal analysts, allows for profound evaluation of epilepsy disorders and of potential epilepsy surgery candidates. This holds particularly true for the evaluation of extra-temporal and cryptogenic epilepsies. This close cooperation between subspecialized clinicians and researchers from various fields has triggered important knowledge about the function of the human brain, including contributions to modern neuroscientific concepts about memory, behavior, awareness, and the human self. It is thus important that the community with an interest in epilepsy diagnostics and epilepsy surgery will work into the direction of more precise spatial allocation of the epileptogenic zone, be it by a combination of signal analysis and imaging or by co-registration of various morphologic, functional, and metabolic imaging modalities in order to further improve the long-term outcome. There is still considerable room for improvement when looking at the present rates for seizure freeness, which have been outlined by the authors of this review, which are in the range of 60–70 % for temporal lobe epilepsy surgical procedures and clearly lesser for extra-temporal epilepsy surgical procedures. Deep brain stimulation for modulation of neuronal circuits and, experimentally, possibly by optogenetics, will further improve our knowledge and potential clinical outcome in this fascinating field of applied clinical neuroscience.
Antonio Gonçalves-Ferreira, Lisbon, Portugal
The authors present a comprehensive review of rates and predictors of seizure freedom after resective epilepsy surgery based on an extensive class I evidence meta-analyses and the experience of their own institution, the UCSF Comprehensive Epilepsy Center. They divide this subject into four main categories—mesial temporal lobe sclerosis, brain tumors, malformations of cortical development, and vascular malformations—that are indeed the major causes of refractory epilepsy. Nevertheless, other lesions like extrinsic neoplasms, namely, meningeomas are also important epileptogenic pathologies that stay out of the scope of this review, but cannot be forgotten.
The discussion about the surgical management of epilepsy for the lesions focused in each chapter is well elaborated and includes the most significant aspects that must be taken into consideration by those who are involved in this practice. As the title indicates, nothing is mentioned about other kinds of surgical treatment of epilepsy such as radiosurgery or the different forms of palliative surgery, namely, calosotomy or other more recent disconnection procedures; these treatments, as well as the neuromodulation techniques (VNS, DBS), represent nowadays an important contribution for the treatment of refractory epilepsy, although seldom resulting in a complete seizure freedom.
As the authors point in their own “Limitations” comment, they do not present any detailed information about the surgical complications, a matter of great concern for the neurosurgeons. The postoperative quality of life including neuropsychological and psychiatric implications is equally assumed as out of focus in this text.
The conclusions highlight the two main predictors of seizure freedom that are modifiable in the natural history of this kind of epilepsies: the early surgical intervention and the gross total removal of the epileptogenic zone.
Globally considered, it is a very interesting review on this subject, pleasant to read, and providing important updated information for all people engaged in the surgical treatment of epilepsy, notably the young doctors.
This manuscript has not been previously published in whole or in part and is not currently submitted elsewhere for review.
Rights and permissions
About this article
Cite this article
Englot, D.J., Chang, E.F. Rates and predictors of seizure freedom in resective epilepsy surgery: an update. Neurosurg Rev 37, 389–405 (2014). https://doi.org/10.1007/s10143-014-0527-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0527-9