Abstract
Purpose
The purpose of this study was to evaluate the diagnostic accuracy of the sonographic fat pad sign (FPS) as a predictor for pediatric elbow fractures.
Patients and methods
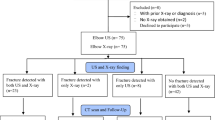
This is a prospective study of children under 14 years with suspected elbow fractures. All participants underwent at first ultrasonography focused on a FPS followed by standard elbow radiographs. US findings were compared to final fracture diagnosis.
Results
38 out of 79 children had an elbow fracture. A sonographic FPS predicted an elbow fracture with a sensitivity/specificity of 97.3/90.5 %, positive/negative likelihood ratios (LR) were 10.2/0.03 and correct/false classification rates were 93.7/6.3 %. Primary US findings were later reviewed by a blinded physician giving a congruity of 96.2 %. These secondary US findings predicted an elbow fracture with a sensitivity/specificity of 92.1/92.7 %, positive/negative LRs were 12.6/0.09 and correct/false classification rates were 92.4/7.5 %.
Conclusion
The sonographic FPS could serve as a useful screening tool in primary evaluation of pediatric elbow injuries. If a fracture is unlikely after clinical and US evaluation, additional radiographs are dispensable, thereby potentially minimizing the radiation burden in childhood and reducing the length of stay in the Emergency Department.




Similar content being viewed by others
References
Bache E. Elbow injuries. In: Johnson KJ, Bache E, editors. Imaging in pediatric skeletal trauma. 1st ed. Berlin: Springer; 2008. p. 257–80.
Hell A, Weinberg AM, Kraus R, et al. Kapitel 14 Ellbogen. In: Weinberg AM, Tscherne H, editors. Unfallchirurgie im Kindesalter. Berlin: Springer; 2006. p. 253–95.
Alzen G, Duque-Reina D, Urhan R, et al. Radiological examinations after trauma in children: clinical and medico-legal considerations about their indications. Dtsch Med Wschr. 1992;117:363–7.
Alzen G, Benz-Bohm G. Radiation protection in pediatric radiology. Dtsch Arztebl Int. 2011;108:407–14.
Brenner DJ, Dollc R, Goodheadd DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. PNAS. 2003;100:13761–6.
Brix G, Nekolla E, Griebel J. Radiation exposure of patients from diagnostic and interventional X-ray procedures. Facts, assessment and trends. Radiologe. 2005;45:340–9.
Fletcher EW, Baum JD, Draper G. The risk of diagnostic radiation of the newborn. Br J Radiol. 1986;59:165–70.
Linet MS, Kim K, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol. 2009;39:S4.
Donnelly LF, Klostermeier TT, Klosterman LA. Traumatic elbow effusions in pediatric patients: are occult fractures the rule? AJR. 1998;171:243–5.
Fick DS, Lyons TA. Interpreting elbow radiographs in children. Am Fam Physician. 1997;55:1278–82.
Kraus R, Berthold LD, von Laer L. Efficient imaging of elbow injuries in children and adolescents. Klin Padiatr. 2007;219:282–7.
Major NM, Crawford ST. Elbow effusions in trauma in adults and children: is there an occult fracture? AJR. 2002;178:413–8.
Norell HG. Roentgenologic visualization of the extracapsular fat; its importance in the diagnosis of traumatic injuries to the elbow. Acta Radiol. 1954;42:205–10.
O’Dwyer H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J Comput Assist Tomogr. 2004;28:562–5.
Skaggs D, Pershad J. Pediatric elbow trauma. Pediatr Emerg Care. 1997;13:425–34.
Miles KA, Lamont AC. Ultrasonic demonstration of the elbow fat pads. Clin Radiol. 1989;40:602–4.
Rabiner JE, Khine H, Avner JR, et al. Accuracy of point-of-care ultrasonography for diagnosis of elbow fractures in children. Ann Emerg Med. 2013;61:9–17.
Barata I, Spencer R, Suppiah A, et al. Emergency ultrasound in the detection of pediatric long-bone fractures. Pediatr Emerg Care. 2012;28:1154–7.
Hübner U, Schlicht W, Outzen S. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg [Br]. 2000;82-B:1170–3.
Moritz JD, Berthold LD, Soenksen SF, et al. Ultrasound in diagnosis of fractures in children: unnecessary harassment or useful addition to X-ray? Ultraschall Med. 2008;29:267–74.
Moritz JD, Hoffmann B, Meuser SH, et al. Is ultrasound equal to X-Ray in pediatric fracture diagnosis? Fortschr Röntgenstr. 2010;182:706–14.
Patel DD, Blumberg SM, Crain EF. The utility of bedside ultrasonography in identifying fractures and guiding fracture reduction in children. Pediatr Emerg Care. 2009;25:221–5.
Rathfelder FJ, Paar O. Ultrasound as an alternative diagnostic measure for fractures during the growth phase. Unfallchirurg. 1995;98:645–9.
Ackermann O, Liedgens P, Eckert K, et al. Sonographische Diagnostik von metaphysären Wulstbrüchen. Der Unfallchirurg. 2009;112:706–11.
Ackermann O, Sesia S, Berberich T, et al. Sonographische Diagnostik der subcapitalen Humerusfraktur im Wachstumsalter. Der Unfallchirurg. 2010;113:839–44.
Ackermann O, Sesia S, Berberich T, et al. Evaluation of proximal humerus fractures in children with ultrasonography a prospective multicenter study. Eur J Trauma Emerg Surg. 2011;37:322.
Chaar-Alvarez FM, Warkentine F, Keith Cross K. Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27:1027–32.
Chien M, Bulloch B, Garcia-Filion P. Bedside ultrasound in the diagnosis of pediatric clavicle fractures. Pediatr Emerg Care. 2011;27:1038–41.
Eckert K, Ackermann O, Schweiger B, et al. Ultrasound as a viable alternative to standard X-rays for the diagnosis of distal forearm fractures in children. Z Orthop Unfall. 2012;150:409–14.
Eckert K, Ackermann O, Schweiger B, et al. Sonographic diagnosis of metaphyseal forearm fractures in children: a safe and applicable alternative to standard X-rays. Pediatr Emerg Care. 2012;28:851–4.
Pountos I, Clegg J, Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: a prospective randomised single blind study. J Child Orthop. 2010;4:321–6.
Williamson D, Watura R, Cobby M. Ultrasound imaging of forearm fractures in children: a viable alternative? J Accid Emerg Med. 2000;17:22–4.
Davidson RS, Markowitz RI, Dormans J, et al. Ultrasonographic evaluation of the elbow in infants and young children after suspected trauma. J Bone Joint Surg Am. 1994;76:1804–13.
Eckert K, Ackermann O, Schweiger B, et al. Ultrasound evaluation of elbow fractures in children. J Med Ultrason. 2013;40:443–51.
Grechenig W, Clement HG, Schatz B, et al. Sonographic examination of trauma to the elbow and hand. Orthopäde. 2002;31:271–7.
Markowitz RI, Davidson RS, Harty MP, et al. Sonography of the elbow in infants and children. AJR. 1992;159:829–33.
Martinoli C, Bianchi S, Zamorani MP, et al. Ultrasound of the elbow. Eur J Ultrasound. 2001;14:21–7.
Pistor G, Graffstädt H. Sonographic diagnosis of supracondylar fractures of the humerus—retrospective and prospective studies in children. Ultraschall Med. 2003;24:331–9.
Tran N, Chow K. Ultrasonography of the elbow. Semin Musculoskelet Radiol. 2007;11:105–16.
Zhang JD, Chen H. Ultrasonography for non-displaced and mini-displaced humeral lateral condyle fractures in children. Chin J Traumatol. 2008;11:297–300.
Zuazo I, Bonnefoy O, Tauzin C, et al. Acute elbow trauma in children: role of ultrasonography. Pediatr Radiol. 2008;38:982–8.
De Maeseneer M, Jacobson JA, Jaovisidha S, et al. Elbow effusions: distribution of joint fluid with flexion and extension and imaging implications. Invest Radiol. 1998;33:117–25.
Conflict of interest
None.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, revised in 2008. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Eckert, K., Ackermann, O., Janssen, N. et al. Accuracy of the sonographic fat pad sign for primary screening of pediatric elbow fractures: a preliminary study. J Med Ultrasonics 41, 473–480 (2014). https://doi.org/10.1007/s10396-014-0525-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-014-0525-0