Abstract
Background
A diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) may relieve symptoms of irritable bowel syndrome (IBS). However, nutritional counseling is resource-demanding and not all patients will benefit.
Aims
To explore whether gut microbial composition may identify symptom response to a low-FODMAP diet in patients with IBS.
Methods
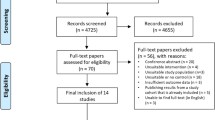
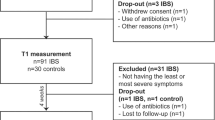
Patients were recruited consecutively to participate in a 4-week FODMAP-restricted diet. Response to diet was defined as ≥ 50% decrease in IBS symptom severity scores (IBS-SSS) compared to baseline. Fecal microbiota were analyzed by a commercially available method (the GA-map™ Dysbiosis Test), assessing 54 bacterial markers targeting more than 300 bacteria at different taxonomic levels.
Results
Sixty-one patients (54 F; 7 M) were included: 32 (29 F; 3 M) classified as responders and 29 (25 F; 4 M) as non-responders. Ten of the 54 bacterial markers differed significantly between responders and non-responders. Based on median values (used as cutoff) of responders for these 10 bacterial markers, we constructed a Response Index (RI): Each patient was given a point when the value for each selected bacterial marker differed from the cutoff. These points were summed up, giving an RI from 0 to 10. Patients with RI > 3 were 5 times more likely to respond (OR = 5.05, 95% CI [1.58; 16.10]), and the probability to respond was 83.4%, 95% CI [61.2–94%].
Conclusions
Gut microbial composition, assessed by using a new RI, may constitute a tool to identify patients that are likely to respond to dietary FODMAP restriction.



Similar content being viewed by others
References
Sperber AD, Dumitrascu D, Fukudo S, et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut 2016.
Enck P, Aziz Q, Barbara G, et al. Irritable bowel syndrome. Nat Rev Dis Primers. 2016;2:16014.
Rajilic-Stojanovic M, Jonkers DM, Salonen A, et al. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol. 2015;110:278–287.
Nanayakkara WS, Skidmore PM, O’Brien L, Wilkinson TJ, Gearry RB. Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date. Clin Exp Gastroenterol. 2016;9:131–142.
Halmos EP, Christophersen CT, Bird AR, Shepherd SJ, Gibson PR, Muir JG. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut. 2015;64:93–100.
Valeur J, Roseth AG, Knudsen T, et al. Fecal fermentation in irritable bowel syndrome: influence of dietary restriction of fermentable oligosaccharides, disaccharides, monosaccharides and polyols. Digestion. 2016;94:50–56.
Yao CK, Muir JG, Gibson PR. Review article: insights into colonic protein fermentation, its modulation and potential health implications. Aliment Pharmacol Ther. 2016;43:181–196.
Daien CI, Pinget GV, Tan JK, Macia L. Detrimental impact of microbiota-accessible carbohydrate-deprived diet on gut and immune homeostasis: an overview. Front Immunol. 2017;8:548.
Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491.
Tveito K, Brunborg C, Bratlie J, et al. Intestinal malabsorption of D-xylose: comparison of test modalities in patients with celiac disease. Scand J Gastroenterol. 2010;45:1289–1294.
Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: the FODMAP approach. J Gastroenterol Hepatol. 2010;25:252–258.
Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402.
Irvine EJ, Whitehead WE, Chey WD, et al. Design of treatment trials for functional gastrointestinal disorders. Gastroenterology. 2006;130:1538–1551.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
Lind R, Berstad A, Hatlebakk J, Valeur J. Chronic fatigue in patients with unexplained self-reported food hypersensitivity and irritable bowel syndrome: validation of a Norwegian translation of the Fatigue Impact Scale. Clin Exp Gastroenterol. 2013;6:101–107.
Casen C, Vebo HC, Sekelja M, et al. Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment Pharmacol Ther. 2015;42:71–83.
Altman DG, Machin D, Bryant TN, Gardner MJ. Statistics with confidence. 2nd ed. New York: BMJ Books; 2000.
James G, Witten D, Hastie T, Tibshirani R. An introduction to statistical learning. New York: Springer; 2013.
Collins SM. A role for the gut microbiota in IBS. Nat Rev Gastroenterol Hepatol. 2014;11:497–505.
Parkes GC, Brostoff J, Whelan K, Sanderson JD. Gastrointestinal microbiota in irritable bowel syndrome: their role in its pathogenesis and treatment. Am J Gastroenterol. 2008;103:1557–1567.
Carroll IM, Ringel-Kulka T, Keku TO, et al. Molecular analysis of the luminal- and mucosal-associated intestinal microbiota in diarrhea-predominant irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2011;301:G799–G807.
Jalanka-Tuovinen J, Salojarvi J, Salonen A, et al. Faecal microbiota composition and host-microbe cross-talk following gastroenteritis and in postinfectious irritable bowel syndrome. Gut. 2014;63:1737–1745.
Hustoft TN, Hausken T, Ystad SO, et al. Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome. Neurogastroenterol Motil 2016.
Chumpitazi BP, Cope JL, Hollister EB, et al. Randomised clinical trial: gut microbiome biomarkers are associated with clinical response to a low FODMAP diet in children with the irritable bowel syndrome. Aliment Pharmacol Ther. 2015;42:418–427.
Vieira-Silva S, Falony G, Darzi Y, et al. Species-function relationships shape ecological properties of the human gut microbiome. Nat Microbiol. 2016;1:16088.
Khanna S, Montassier E, Schmidt B, et al. Gut microbiome predictors of treatment response and recurrence in primary Clostridium difficile infection. Aliment Pharmacol Ther. 2016;44:715–727.
Magnusson MK, Strid H, Sapnara M, et al. Anti-TNF therapy response in patients with ulcerative colitis is associated with colonic antimicrobial peptide expression and microbiota composition. J Crohns Colitis. 2016;10:943–952.
Bennet SMP, Bohn L, Storsrud S, et al. Multivariate modelling of faecal bacterial profiles of patients with IBS predicts responsiveness to a diet low in FODMAPs. Gut 2017.
David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563.
Acknowledgments
The work of the clinical dietician (TK) and the microbial DNA analyses were funded by Genetic Analysis AS, Oslo, Norway. Otherwise, the study was funded by Lovisenberg Diaconal Hospital, Oslo, Norway.
Author information
Authors and Affiliations
Contributions
JV conceived and designed the study, performed the data collection, and wrote the manuscript. MCS performed the statistical analyses and wrote the manuscript. TK guided the patients throughout the dietary intervention. GAL interpreted the data and contributed to critical revision. AR conceived and designed the study, and recruited the patients. All authors reviewed and approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the Regional Committee for Medical Research Ethics (REK Sør-Øst, Reference No. 2013/454) and with the 1964 Helsinki Declaration and its later amendments.
Rights and permissions
About this article
Cite this article
Valeur, J., Småstuen, M.C., Knudsen, T. et al. Exploring Gut Microbiota Composition as an Indicator of Clinical Response to Dietary FODMAP Restriction in Patients with Irritable Bowel Syndrome. Dig Dis Sci 63, 429–436 (2018). https://doi.org/10.1007/s10620-017-4893-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4893-3