Abstract
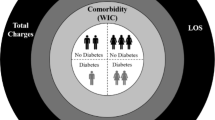
The objective of this paper is to model the impact of comorbidity on breast cancer patient outcomes (e.g., length of stay and disposition). Previous studies suggest that comorbidities may significantly affect mortality risks for breast cancer patients. The 2006 AHRQ Nationwide Inpatient Sample (NIS) is used to analyze the relationships among comorbidities (e.g., hypertension, diabetes, obesity, and mental disorder), total charges, length of stay, and patient disposition as a function of age and race. A multifaceted approach is used to quantify these relationships. A causal study is performed to explore the effect of various comorbidities on patient outcomes. Least squares regression models are developed to evaluate and compare significant factors that influence total charges and length of stay. Logistic regression is used to study the factors that may cause patient mortality or transferring. In addition, different survival models are developed to study the impact of comorbidity on length of stay with censoring information. This study shows the interactions and relationship among various comorbidities and breast cancer. It shows that certain hypertension may not increase length of stay and total charges; diabetes behaves differently among general population and breast cancer patients; mental disorder has an impact on patient disposition that affects true length of stay and charges, and obesity may have limited effect on patient outcomes. Moreover, this study will help to better understand the expenditure patterns for population subgroups with several chronic conditions and to quantify the impact of comorbidities on patient outcomes. Lastly, it also provides insight for breast cancer patients with comorbidities as a function of age and race.
Similar content being viewed by others
References
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Medical Care 36(1):8–27
Chronic Disease Prevention and Health Promotion (2009) Chronic disease—the power to prevent, the call to control: at a glance. National Center for Chronic Disease Prevention and Health Promotion and Department of Health and Human Services, Editors: Atlanta
Centers for Disease Control and Prevention (2009) Chronic Disease Overview. Available via: http://www.cdc.gov/NCCdphp/overview.htm. Accessed 10 March 2009
Suthummanon S, Omachonu VK (2004) DRG-based cost minimization models: Applications in a hospital environment. Health Care Manag Sci 7:197–205
Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP (2003) Comorbidity: Implications for the importance of primary care in 'case' management. Ann Fam Med 1(1):8–14
CDC. United States Cancer Statistics Working Group: 1999–2005 Incidence and Mortality Web-based Report. Available from: http://www.cdc.gov/uscs. Accessed 11 March 2009
Jamel A et al (2007) Cancer Statistics, 2007. CA-Cancer J Clin 57:43–66
Komen (2006) Facts of Life. Komen Foundation
Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D (2005) Comorbidity and survival disparities among black and white patients with breast cancer. JAMA-J Am Med Assoc 294(14):1765–1772
Brandeau ML, Zaric GS (2009) Optimal investment in HIV prevention programs: More is not always better. Health Care Manag Sci 12:27–37
Zhao SZ, Wong JM, Arguelles LM (1999) Hospitalization costs associated with leiomyoma. Clin Ther 21(3):563–575
Livingston EH, Langert J (2006) The impact of age and medicare status on bariatric surgical outcomes. Arch Surg 141(11):1115–1120
Meguid RD, Brooke BS, Chang DC, Sherwood JT, Brock MV, Yang SC (2008) Are surgical outcomes for lung cancer resections improved at teaching hospitals? Ann Thorac Surg 85:1015–1025
Newschaffer CJ, Bush TL, Penberthy LE et al (1998) Does comorbid disease interact with cancer? An epidemiologic analysis of mortality in a cohort of elderly breast cancer patients. J Gerontol A Biol Sci Med Sci 53(5):M372–378
Yancik R, Wesley MN, Ries LA, Havlik RJ, Edwards BK, Yates JW (2001) Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. JAMA 285(7):885–892
Lash TL, Fox MP, Buist DSM et al (2007) Mammography surveillance and mortality in older breast cancer survivors. J Clin Oncol 25(21):3001–3006
Farley JF, Harley CR, Devine JW (2006) A comparison of comorbidity measurements to predict healthcare expenditures. Am J Manag Care 12:110–117
Garis RI, Farmer K (2002) Examining costs of chronic conditions in a Medicaid population. Manag Care 11:43–50
Dominick KL, Dudley TK, Coffman CJ, Bosworth HB (2005) Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthrit Care Res 53(5):666–672
Piccirillo JF, Tierney RN, Costas I, Grove L, Spitznagel EL (2004) Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA 291:2441–2447
De Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity: A critical review of available methods. J Clin Epidemiol 56(3):221–229
Li J (1999) An application of lifetime models in estimation of expected length of stay of patients in hospital with complexity and age adjustment. Stat Med 18(23):3337–3344
Sá C, Dismuke CE, Guimaraes P (2007) Survival analysis and competing risk models of hospital length of stay and discharge destination: The effect of distributional assumptions. Health Serv Outcomes Res Method 7:109–124
Roehrig C, Miller G, Lake C, Bryant J (2009) National health spending by medical condition, 1996–2005. Health Affair 28(2):358–367
HCUP (2008) Healthcare Cost and Utilization Project (HCUP) Databases. Agency for Healthcare Research and Quality. Editor: Rockville, MD
ICD-9 Codes for Breast Cancer. Available from: www.fortherecordmag.com/archives/ftr_021405p33.shtml. Accessed 23 Feb 2009
ICD-9 Codes for Hypertension. Available from: http://www.fortherecordmag.com/archives/ftr_01232006p44.shtml. Accessed 23 Feb 2009
ICD-9 Codes for Obesity. Available from: http://www.fortherecordmag.com/archives/ftr_012604p39.shtml. Accessed 23 Feb 2009
Klemi PJ, Parvinen I, Pylkkänen L et al (2003) Significant improvement in breast cancer survival through population-based mammography screening. Breast 12(5):308–313
Holmes CE, Muss HB (2003) Diagnosis and treatment of breast cancer in the elderly. CA-Cancer J Clin 53(4):227–244
Rovera F, Dionigi G, Riva C, Chiaravallib A et al (2008) Identifying factors contributing to reduced breast tumor size: a longitudinal study. Int J Surg 6(Suppl 1):S97–S100
Acknowledgement
We would like to thank the three anonymous referees for their valuable and constructive comments and suggestions which have helped us greatly improve this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, S., Ivy, J.S., Payton, F.C. et al. Modeling the impact of comorbidity on breast cancer patient outcomes. Health Care Manag Sci 13, 137–154 (2010). https://doi.org/10.1007/s10729-009-9119-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-009-9119-6