Abstract
It is reported that defects exist in the small intestinal epithelial barrier of inflammatory bowel disease, which might be associated with increased intestinal permeability at a very early stage. Our study aims to investigate the role of Lactobacillus plantarum on the decrease of epithelial permeability and the further protective effects on the intestinal epithelial barrier using the IL-10-deficient mouse model. Our study showed that tight junction associated proteins were increased after the pre-treatment of L. plantarum by fluorescence staining, western blot, real-time PCR and transmission electron microscope. Oral gavage of milk containing L. plantarum was effective in decreasing small intestinal permeability using methods of Ussing chamber assay and sugar probe. Assay of pro-inflammatory cytokines IFN-γ, TNF-α, MPO, and colonic histology by ELISA showed protective effects of L. plantarum on the intestinal epithelial barrier. Therefore, L. plantarum may prevent the development of colitis in IL-10-deficient mice by blocking changes in the expression of TJ proteins, TJ structure and intestinal permeability.





Similar content being viewed by others
References
Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI (2005) Host-bacterial mutualism in the human intestine. Science 307(5717):1915–1920
Zhang M, Wang XQ, Zhou YK et al (2009) Effects of oral Lactobacillus plantarum on hepatocyte tight junction structure and function in rats with obstructive jaundice. Mol Biol Rep [Epub ahead of print]
Nuding S, Fellermann K, Wehkamp J, Stange EF (2007) Reduced mucosal antimicrobial activity in Crohn’s disease of the colon. Gut 56(9):1240–1247
Rhodes JM (2007) The role of Escherichia coli in inflammatory bowel disease. Gut 56(5):610–612
Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R (2004) Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell 118(2):229–241
Fiocchi C (2005) One commensal bacterial molecule—all we need for health? N Engl J Med 353(19):2078–2080
Alverdy JC, Laughlin RS, Wu L (2003) Influence of the critically ill state on host–pathogen interactions within the intestine: gut-derived sepsis redefined. Crit Care Med 31(2):598–607
Sartor RB (2004) Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: antibiotics, probiotics, and prebiotics. Gastroenterology 126(6):1620–1633
Ewaschuk J, Endersby R, Thiel D et al (2007) Probiotic bacteria prevent hepatic damage and maintain colonic barrier function in a mouse model of sepsis. Hepatology 46(3):841–850
Surendran S (2009) Upregulation of N-acetylaspartic acid alters inflammation, transcription and contractile associated protein levels in the stomach and smooth muscle contractility. Mol Biol Rep 36(1):201–206
Matsuzaki T, Takagi A, Ikemura H, Matsuguchi T, Yokokura T (2007) Intestinal microflora: probiotics and autoimmunity. J Nutr 137(3 Suppl 2):798S–802S
Madsen K, Cornish A, Soper P et al (2001) Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 121(3):580–591
Arrieta MC, Madsen K, Doyle J, Meddings J (2009) Reducing small intestinal permeability attenuates colitis in the IL10 gene-deficient mouse. Gut 58(1):41–48
Song XM, Wang YL, Li JG et al (2009) Effects of propofol on pro-inflammatory cytokines and nuclear factor kappaB during polymicrobial sepsis in rats. Mol Biol Rep 36(8):2345–2351
Tao GH, Yang LQ, Gong CM et al (2009) Effect of PARP-1 deficiency on DNA damage and repair in human bronchial epithelial cells exposed to Benzo(a)pyrene. Mol Biol Rep 36(8):2413–2422
Sibartie S, Scully P, Keohane J et al (2010) Mycobacterium avium subsp. Paratuberculosis (MAP) as a modifying factor in Crohn’s disease. Inflamm Bowel Dis 16(2):296–304
Arrieta MC, Bistritz L, Meddings JB (2006) Alterations in intestinal permeability. Gut 55(10):1512–1520
Madsen KL, Lewis SA, Tavernini MM, Hibbard J, Fedorak RN (1997) Interleukin 10 prevents cytokine-induced disruption of T84 monolayer barrier integrity and limits chloride secretion. Gastroenterology 113(1):151–159
Kim SC, Tonkonogy SL, Albright CA et al (2005) Variable phenotypes of enterocolitis in interleukin 10-deficient mice monoassociated with two different commensal bacteria. Gastroenterology 128(4):891–906
Sydora BC, Macfarlane SM, Walker JW et al (2007) Epithelial barrier disruption allows nondisease-causing bacteria to initiate and sustain IBD in the IL-10 gene-deficient mouse. Inflamm Bowel Dis 13(8):947–954
Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W (1993) Interleukin-10-deficient mice develop chronic enterocolitis. Cell 75(2):263–274
Adawi D, Kasravi FB, Molin G, Jeppsson B (1997) Effect of Lactobacillus supplementation with and without arginine on liver damage and bacterial translocation in an acute liver injury model in the rat. Hepatology 25(3):642–647
Mao Y, Nobaek S, Kasravi B et al (1996) The effects of Lactobacillus strains and oat fiber on methotrexate-induced enterocolitis in rats. Gastroenterology 111(2):334–344
Wang B, Li J, Li Q, Zhang H, Li N (2009) Isolation of adhesive strains and evaluation of the colonization and immune response by Lactobacillus plantarum L2 in the rat gastrointestinal tract. Int J Food Microbiol 132(1):59–66
Suzuki T, Seth A, Rao R (2008) Role of phospholipase Cgamma-induced activation of protein kinase Cepsilon (PKCepsilon) and PKCbetaI in epidermal growth factor-mediated protection of tight junctions from acetaldehyde in Caco-2 cell monolayers. J Biol Chem 283(6):3574–3583
Lelievre V, Hu Z, Byun JY, Ioffe Y, Waschek JA (2002) Fibroblast growth factor-2 converts PACAP growth action on embryonic hindbrain precursors from stimulation to inhibition. J Neurosci Res 67(5):566–573
Meddings JB, Gibbons I (1998) Discrimination of site-specific alterations in gastrointestinal permeability in the rat. Gastroenterology 114(1):83–92
Saverymuttu SH, Camilleri M, Rees H et al (1986) Indium 111-granulocyte scanning in the assessment of disease extent and disease activity in inflammatory bowel disease. A comparison with colonoscopy, histology, and fecal indium 111-granulocyte excretion. Gastroenterology 90(5 Pt 1):1121–1128
Reid G, Jass J, Sebulsky MT, McCormick JK (2003) Potential uses of probiotics in clinical practice. Clin Microbiol Rev 16(4):658–672
Rutgeerts P, Sandborn WJ, Feagan BG et al (2005) Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med 353(23):2462–2476
Schultz M (2008) Clinical use of E. coli Nissle 1917 in inflammatory bowel disease. Inflamm Bowel Dis 14(7):1012–1018
Miele E, Pascarella F, Giannetti E et al (2009) Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol 104(2):437–443
Santosa S, Farnworth E, Jones PJ (2006) Probiotics and their potential health claims. Nutr Rev 64(6):265–274
Olson TS, Reuter BK, Scott KG et al (2006) The primary defect in experimental ileitis originates from a nonhematopoietic source. J Exp Med 203(3):541–552
Mannon P (2009) Gut permeability and colitis. Gastroenterology 137(2):732–734
Balda MS, Matter K (2008) Tight junctions at a glance. J Cell Sci 121(Pt 22):3677–3682
Suzuki T, Elias BC, Seth A et al (2009) PKC eta regulates occludin phosphorylation and epithelial tight junction integrity. Proc Natl Acad Sci USA 106(1):61–66
Isolauri E, Majamaa H, Arvola T et al (1993) Lactobacillus casei strain GG reverses increased intestinal permeability induced by cow milk in suckling rats. Gastroenterology 105(6):1643–1650
Johnson-Henry KC, Donato KA, Shen-Tu G, Gordanpour M, Sherman PM (2008) Lactobacillus rhamnosus strain GG prevents enterohemorrhagic Escherichia coli O157:H7-induced changes in epithelial barrier function. Infect Immun 76(4):1340–1348
Gareau MG, Jury J, MacQueen G, Sherman PM, Perdue MH (2007) Probiotic treatment of rat pups normalises corticosterone release and ameliorates colonic dysfunction induced by maternal separation. Gut 56(11):1522–1528
Mangell P, Nejdfors P, Wang M et al (2002) Lactobacillus plantarum 299v inhibits Escherichia coli-induced intestinal permeability. Dig Dis Sci 47(3):511–516
Kumar A, Singh NK, Sinha PR (2010) Inhibition of 1,2-dimethylhydrazine induced colon genotoxicity in rats by the administration of probiotic curd. Mol Biol Rep 37(3):1373–1376
Acknowledgments
The authors thank Dr. Hang Xiaomin (Institute of Science Life of Only, Shanghai Jiao Tong University, Shanghai, China) for generous provision of Lactobacillus plantarum CGMCC 1258. The authors thank Shanghai Jiao Tong University Affiliated Sixth People’s Hospital for technical assistance during this study. This work was financially supported by National Natural Science Foundation of China (No. 30672044), and the National Basic Research Program of China (No. 2008CB517403).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11033_2010_237_MOESM2_ESM.tif
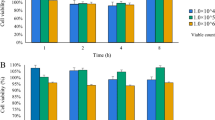
Fig. S1 L. plantarum prevented the injury of tight junction (TJ) and F-actin by fluorescence staining. Line 1 In milk group of IL-10-deficient mice, the fluorescence of F-actin and TJ associated proteins, including occludin, Claudin-1, JAM-1 and ZO-1, was faint, with the fluorescence distributed dispersedly. Lines 2, 3 In the L. plantarum group and AT-1001 group, the intensity of fluorescence and distribution of TJ and F-actin were improved obviously. Line 4 In the group of wild-type mice, TJ and F-actin were continuously distributed with bright green spots along membrane of the cells in the tissue. Original magnification ×2,400 (TIFF 8101 kb)
11033_2010_237_MOESM3_ESM.tif
Fig. S2 L. plantarum protected the ultra-structural of tight junction (TJ) by transmission electron microscope (TEM). A In milk group of IL-10-deficient mice, ultra-structural of TJ was showed as irregular. B, C In the L. plantarum group and AT-1001 group, ultra-structural of TJ was improved obviously. D In the group of wild-type mice, ultra-structural of TJ was shown to be normal (TIFF 4808 kb)
11033_2010_237_MOESM4_ESM.tif
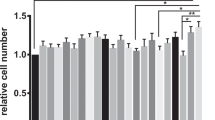
Fig. S3 Small intestinal and colonic permeability were reduced by L. plantarum. A Small intestinal permeability was decreased after given oral gavage of L. plantarum and AT-1001 from 4 weeks and more significant after 8 weeks of age when the small intestinal permeability of IL-10-deficient mice returned to the normal level. B Colonic permeability of IL-10-deficient mice was increased significantly compared with the wild-type; while L. plantarum and AT-1001 had an ameliorating effect after week 10. * P < 0.05. One-way ANOVA was performed with Tukey–Kramer post-hoc comparison. Values were calculated by Student’s t-test. All data are given as mean ± standard deviation (SD) (TIFF 624 kb)
Rights and permissions
About this article
Cite this article
Liu, Z., Zhang, P., Ma, Y. et al. Lactobacillus plantarum prevents the development of colitis in IL-10-deficient mouse by reducing the intestinal permeability. Mol Biol Rep 38, 1353–1361 (2011). https://doi.org/10.1007/s11033-010-0237-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-010-0237-5