Abstract
Purpose
To provide a simplified dosing schedule and potentially reduce side effects associated to peak plasma concentrations, an in situ-forming oleogel implant was studied for the sustained-release of rivastigmine.
Materials and methods
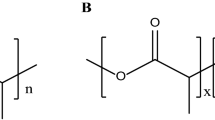
The gel was prepared by dissolving 5–10% (w/w) N-stearoyl l-alanine methyl ester (SAM) organogelator in safflower oil containing either dissolved rivastigmine or its dispersed hydrogen tartrate salt. Rheological analysis, differential scanning calorimetry, and infrared spectroscopy were carried out to assess the impact of drug incorporation on the oleogel; this was followed by in vitro and in vivo release studies.
Results
A weakening of intermolecular interactions was suggested by gel-sol transition temperature drops of 10–15°C upon incorporation of dissolved drug. Meanwhile, the dispersed drug salt induced minimal or no changes in transition temperature. Gels containing dispersed rivastigmine had the lowest burst in vitro (<15% in 24 h). In vivo, the 10% SAM formulation containing dispersed rivastigmine provided prolonged drug release within the therapeutic range for 11 days, with peak plasma levels well below the toxic threshold and up to five times lower than for the control formulation.
Conclusions
This study established SAM gels to be a promising option for sustained-release formulations in the treatment of Alzheimer’s Disease.






Similar content being viewed by others
References
C. Mount and C. Downton. Alzheimer disease: progress or profit? Nat. Med. 12:780–784 (2006).
R. Katzman. Alzheimer’s disease. NEJM 314:964–973 (1986).
C. G. Ballard. Advances in the treatment of Alzheimer’s disease: benefits of dual cholinesterase inhibition. Eur. Neurol. 47:64–70 (2002).
A. Lleo, S. M. Greenberg, and J. H. Growdon. Current pharmacotherapy for Alzheimer’s disease. Ann. Rev. Med. 57:513–533 (2006).
S. Gauthier. Long-term efficacy of cholinesterase inhibitors. Brain Aging 2:9–22 (2002).
V. W. DeLaGarza. Pharmacologic treatment of Alzheimer’s disease: an update. Am. Fam. Physician. 68:1365–1372 (2003).
V. Cotrell, K. Wild, and T. Bader. Medication management and adherence among cognitively impaired older adults. J. Gerontol. Soc. Work 47:31–46 (2006).
D. G. Wilkinson, A. P. Passmore, R. Bullock, S. W. Hopter, R. P. Smith, F. C. Protocnik, C. M. Maud, I. Engelbrecht, C. Hock, J. R. Ieni, and R. S. Bahra. A mutinational, randomised, 12-week, comparative study of donepezil and rivastigmine in patients with mild to moderate Alzheimer’s disease. Int. J. Clin. Pract. 56:441–446 (2002).
G. Singh, S. K. Thomas, S. Arcona, V. Lingala, and A. Mithal. Treatment persistency with rivastigmine and donepezil in a large state medicaid program. J. Am. Geriatr. Soc. 53:1269–1270 (2005).
K. L. Lanctôt, N. Herrmann, K. K. Yau, L. R. Khan, B. A. Liu, M. M. Loulou, and T. R. Einarson. Efficacy and safety of choliesterase inhibitors in Alzheimer’s disease: a meta-analysis. Can. Med. Assoc. J. 169:557–564 (2003).
J. Birks, J. Grimley Evans, V. Iakovidou, and M. Tsolaki. Rivastigmine for Alzheimer’s disease. Cochrane Database Syst. Rev. 4:CD001191 (2000).
W. H. Liu, J. L. Song, K. Liu, D. F. Chu, and Y. X. Li. Preparation and in vitro and in vivo release studies of huperzine A loaded microspheres for the treatment of Alzheimer’s disease. J. Control Release 107:417–427 (2005).
X. Fu, Q. Ping, and Y. Gao. Effects of formulation factors on encapsulation efficiency and release behaviour in vitro of huperzine A-PLGA microspheres. J. Microencapsul. 22:705–714 (2005).
P. Gao, P. Ding, H. Xu, Z. Yuan, D. Chen, J. Wei, and D. Chen. In vitro and in vivo characterization of huperzine A loaded microspheres made from end-group uncapped poly(d,l-lactide acid) and poly(d,l-lactide-co-glycolide acid). Chem. Pharm. Bull. 54:89–93 (2006).
Q. Yang, D. Williams, G. Owusu-Ababio, N. K. Ebube, and M. J. Habib. Controlled release tacrine delivery system for the treatment of Alzheimer’s disease. Drug Deliv. 8:93–98 (2001).
F. L. Tse, and R. Laplanche. Absorption, metabolism, and disposition of [14C]SDZ ENA 713, an acetylcholinesterase inhibitor, in minipigs following oral, intravenous, and dermal administration. Pharm. Res. 15:1614–1620 (1998).
V. R. Sinha, and A. Trehan. Biodegradable microspheres for protein delivery. J. Control Release 90:261–280 (2003).
C. B. Packhaeuser, J. Schnieders, C. G. Oster, and T. Kissel. In situ forming parenteral drug delivery systems: an overview. Eur. J. Pharm. Biopharm. 58:445–455 (2004).
S. Bhattacharya, and Y. Krishnan-Gosh. First report of phase selective gelation of oil from oil/water mixture. Possible implications toward containing oil spills. Chem. Commun. 2:185–186 (2001).
A. C. Couffin-Hoarau, A. Motulsky, P. Delmas, and J. C. Leroux. In situ-forming pharmaceutical organogels based on the self assembly of l-alanine derivatives. Pharm. Res. 21:454–457 (2004).
A. Motulsky, M. Lafleur, A. C. Couffin-Hoarau, D. Hoarau, F. Boury, J. P. Benoit, and J. C. Leroux. Characterization and biocompatibility of organogels based on l-alanine for parenteral drug delivery implants. Biomaterials 26:6242–6253 (2005).
F. Plourde, A. Motulsky, A. C. Couffin-Hoarau, D. Hoarau, H. Ong, and J. C. Leroux. First report on the efficacy of l-alanine-based in situ-forming implants for the long-term parenteral delivery of drugs. J. Control Release 108:433–441 (2005).
K. Fredholt, D. H. Larsen, and C. Larsen. Modification of in vitro drug release rate from oily parenteral depots using a formulation approach. Eur. J. Pharm. Sci. 11:231–237 (2000).
B. M. Rao, M. K. Srinivasu, K. P. Kumar, N. Bhradwaj, R. Ravi, P. K. Mohakhud, G. O. Reddy, and P. R. Kumar. A stability indicating LC method for rivastigmine hydrogen tartrate. J. Pharm. Biomed. Anal. 37:57–63 (2005).
S. M. Nuno-Donlucas, J. C. Sanchez-Diaz, M. Rabelero, J. Cortes-Ortega, C.C. Luhrs-Olmos, V. V. Fernandez-Escamilla, E. Mendizabal, and J. E. Puig. Microstructured polyacrylamide hydrogels made with hydrophobic nanoparticles. J. Colloid. Interface Sci. 270:94–98 (2004).
R. Schmidt, M. Schmutz, M. Michel, G. Decher, and P. J. Mesini. Organogelation properties of a series of oligoamides. Langmuir 18:5668–5672 (2001).
M. R. Farlow. Update on rivastigmine. Neurology 9:230–234 (2003).
Novartis. Exelon TM: Rivastigmine hydrogen tartrate, cholinesterase inhibitor, Compendium of pharmaceutical specialties (CPS), Canadian Pharmacists Association, Ottawa, pp 835–840 (2004).
S. W. Coppack, T. J. Yost, R. M. Fisher, R. H. Eckel, and J. M. Miles. Periprandial systemic and regional lipase activity in normal humans. Am. J. Physiol. 270:E718–E722 (1996).
B. Jeong, Y. K. Choi, Y. H. Bae, G. Zentner, and S. W. Kim. New biodegradable polymers for injectable drug delivery systems. J. Control Release 62:109–114 (1999).
L. Appel, K. Engle, J. Jensen, L. Rajewski, and G. Zentner. An in vitro model to mimic in vivo subcutaneous monoolein degradation. Pharm. Res. 11:S-217 (1994).
Acknowledgements
The authors wish to thank François Plourde for his extensive help with animal studies and Gregoire Leclair for the particle size measurement. Funding for this project was provided by the Canadian Institutes for Health Research (CIHR).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the linked to the electronic supplementary material
Supporting information
(DOC 122 KB)
Rights and permissions
About this article
Cite this article
Vintiloiu, A., Lafleur, M., Bastiat, G. et al. In Situ-Forming Oleogel Implant for Rivastigmine Delivery. Pharm Res 25, 845–852 (2008). https://doi.org/10.1007/s11095-007-9384-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-007-9384-3