Abstract
Purpose
This meta-analytic review aimed to estimate the magnitude of health-related quality of life (HrQoL) impairments, as assessed by the KIDSCREEN questionnaires, both self- and parent-reported, in 8- to 18-years-old children/adolescents with chronic health conditions.
Methods
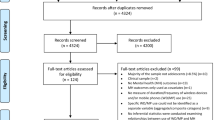
To identify studies using the KIDSCREEN questionnaires, three electronic databases (PubMed, PsycINFO, EBSCOhost Psychology & Behavioral Sciences) were searched. The final search (February 14–15, 2018) revealed 528 non-duplicated articles, of which 23 papers (21 studies) directly compared the HrQoL of pediatric patients to community/healthy controls and were included in the meta-analysis. Pooled mean differences (MD) with 95% CIs were estimated using the inverse-variance random-effects method.
Results
Of the 21 studies, 16 used self-reports, one used parent-reports and four adopted a multi-informant approach. Self-reported data were retrieved from 20 studies (4852 cases/28,578 controls), and parent-reported data were retrieved from four studies (511 cases/433 controls). Pediatric patients presented significant HrQoL impairments in the domains of physical well-being (MD = − 4.84, 95% CI − 6.44/− 3.24 for self-reports; MD = − 6.86, 95% CI − 10.42/− 3.29 for parent-reports) and peers and social support (MD = − 1.29, 95% CI − 2.25/− 0.34 for self-reports; MD = − 3.90, 95% CI − 5.28/− 2.52 for parent-reports), compared to community/healthy peers. Between-studies heterogeneity was explained by diagnostic categories, instrument version and informants.
Conclusions
The identification of significant HrQoL impairments among pediatric patients, specifically in the physical and social domains, highlights the importance of routine psychosocial assessment and intervention in primary pediatric healthcare services. Specific recommendations include the use of profile measures, both self- and parent-reports, and the prioritization of oncology, endocrinology and neurology services.









Similar content being viewed by others
References
References have been highlighted as: *Papers included in the meta-analysis
Newacheck, P. W., & Taylor, W. R. (1992). Childhood chronic illness: Prevalence, severity, and impact. American Journal of Public Health, 82(3), 364–371.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). Impaired health-related quality of life in children and adolescents with chronic conditions: A comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-5-43.
Asher, M. I., Montefort, S., Björkstén, B., Lai, C. K., Strachan, D. P., Weiland, S. K., et al. (2006). Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. https://doi.org/10.1016/S0140-6736(06)69283-0.
Hruby, A., & Hu, F. B. (2015). The epidemiology of obesity: A big picture. PharmacoEconomics. https://doi.org/10.1007/s40273-014-0243-x.
Suris, J., Michaud, P., & Viner, R. (2004). The adolescent with a chronic condition. Part I: Developmental issues. Archives of Disease in Childhood. https://doi.org/10.1136/adc.2003.045369.
Silver, J., Westbrook, L., & Stein, R. (1998). Relationship of parental psychological distress to consequences of chronic health conditions in children. Journal of Pediatric Psychology. https://doi.org/10.1093/jpepsy/23.1.5.
Newacheck, P. W., & Halfon, N. (1998). Prevalence and impact of disabling chronic conditions in childhood. American Journal of Public Health, 88(4), 610–617.
Stein, R. E., & Jessop, D. J. (1989). What diagnosis does not tell: The case for a noncategorical approach to chronic illness in childhood. Social Science and Medicine. https://doi.org/10.1016/0277-9536(89)90157-3.
Stein, R. E., & Silver, E. J. (1999). Operationalizing a conceptually based noncategorical definition: A first look at US children with chronic conditions. Archives of Pediatrics and Adolescent Medicine. https://doi.org/10.1001/archpedi.153.1.68.
Grootenhuis, M. A., Koopman, H. M., Verrips, E. G., Vogels, A. G., & Last, B. F. (2007). Health-related quality of life problems of children aged 8-11 years with a chronic disease. Developmental Neurorehabilitation. https://doi.org/10.1080/13682820600691017.
Bullinger, M., Schmidt, S., Peterson, C., & Ravens-Sieberer, U. (2006). Quality of life—Evaluation criteria for children with chronic conditions in medical care. Journal of Public Health. https://doi.org/10.1007/s10389-006-0066-0.
de Civita, M., Regier, D., Alamgir, A. H., Anis, A. H., Fitzgerald, M. J., & Marra, C. A. (2005). Evaluating health-related quality-of-life studies in paediatric populations: Some conceptual, methodological and developmental considerations and recent applications. Pharmacoeconomics. https://doi.org/10.2165/00019053-200523070-00003.
World Health Organization (WHO). (1993). Measurement of quality of life in children: Report of a WHO/IACAPAP working party. Geneva: World Health Organization.
Ravens-Sieberer, U., Gosch, A., Abel, T., Auquier, P., Bellach, B. M., Bruil, J., et al. (2001). Quality of life in children and adolescents: A European public health perspective. Sozial- und Präventivmedizin. https://doi.org/10.1007/BF01321080.
The WHOQOL Group. (1995). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science and Medicine. https://doi.org/10.1016/0277-9536(95)00112-K.
Herdman, M., Rajmil, L., Ravens-Sieberer, U., Bullinger, M., Power, M., Alonso, J., et al. (2002). Expert consensus in the development of a European health-related quality of life measure for children and adolescents: A Delphi study. Acta Paediatrica. https://doi.org/10.1111/j.1651-2227.2002.tb02838.x.
Detmar, S. B., Bruil, J., Ravens-Sieberer, U., Gosch, A., & Bisegger, C. (2006). The use of focus groups in the development of the KIDSCREEN HRQL questionnaire. Quality of Life Research. https://doi.org/10.1007/s11136-006-0022-z.
Guillemin, F., Bombardier, C., & Beaton, D. (1993). Cross-cultural adaption of health-related quality of life measures: Literature review and proposed guidelines. Journal of Clinical Epidemiology. https://doi.org/10.1016/0895-4356(93)90142-N.
The KIDSCREEN Group Europe. (2006). The KIDSCREEN questionnaires: Quality of life for children and adolescents – Handbook. Lengerich: Pabst Science Publishers.
Dickinson, H. O., Parkinson, K. N., Ravens-Sieberer, U., Schirripa, G., Thyen, U., Arnaud, C., et al. (2007). Self-reported quality of life of 8–12-year-old children with cerebral palsy: A cross-sectional European study. Lancet. https://doi.org/10.1016/S0140-6736(07)61013-7.
Erhart, M., Ravens-Sieberer, U., Dickinson, H. O., & Colver, A. (2009). Rasch measurement properties of the KIDSCREEN quality of life instrument in children with cerebral palsy and differential item functioning between children with and without cerebral palsy. Value in Health. https://doi.org/10.1111/j.1524-4733.2009.00508.x.
Roberts, C., Freeman, J., Schnohr, C. W., Looze, M. E., Nic Gabhainn, S., Rasmussen, M., et al. (2009). The health behaviour in school-aged children (HBSC) study: Methodological developments and current tensions. International Journal of Public Health. https://doi.org/10.1007/s00038-009-5405-9.
Currie, C., Nic Gabhainn, S., & Godeau, E. (2009). The health behaviour in school-aged children: WHO collaborative crossnational (HBSC) study: Origins, concept, history and development 1982–2008. International Journal of Public Health. https://doi.org/10.1007/s00038-009-5404-x.
Liberati, A., Altman, D., Tetzlaff, J., Mulrow, C., Gøtzsche, P., Ioannidis, J., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. British Medical Journal. https://doi.org/10.1136/bmj.b2700.
Ravens-Sieberer, U., Erhart, M., Wille, N., Wetzel, R., Nickel, J., & Bullinger, M. (2006). Generic health-related quality-of-life assessment in children and adolescents: Methodological considerations. Pharmacoeconomics. https://doi.org/10.2165/00019053-200624120-00005.
Mokkink, L. B., van der Lee, J. H., Grootenhuis, M. A., Offringa, M., Heymans, H. S., & Dutch National Consensus Committee Chronic Diseases Health Conditions in Childhood. (2008). Defining chronic diseases and health conditions in childhood (0-18 years of age): National consensus in the Netherlands. European Journal of Pediatrics. https://doi.org/10.1007/s00431-008-0697-y.
World Health Organization (WHO). (2016). International Statistical Classification of Diseases and Related Health Problems 10th Revision. Geneva: World Health Organization.
Sawyer, G., Whaites, L., Rey, M., Hazell, L., Graetz, W., & Baghurst, P. (2002). Health-related quality of life of children and adolescents with mental disorders. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1097/00004583-200205000-00010.
Chen, H., Cohen, P., Kasen, S., Johnson, G., Berenson, K., & Gordon, K. (2006). Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Archives of Pediatrics and Adolescent Medicine. https://doi.org/10.1001/archpedi.160.1.93.
Gerharz, E. W., Eiser, C., & Woodhouse, C. R. (2003). Current approaches to assessing the quality of life in children and adolescents. BJU International. https://doi.org/10.1046/j.1464-410X.2003.04001.x.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174.
Cochrane Consumers & Communication Review Group (2016). Data extraction template for included studies, Version 1.8. Resource document. Retrieved From http://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/det_2015_revised_final_june_20_2016_nov_29_revised.doc. Accessed 15 April 2018.
Higgins, J. P. T., & Green, S. (2008). Cochrane handbook for systematic reviews of interventions. West Sussex: John Wiley & Sons Ltd.
Hozo, S. P., Djulbegovic, B., & Hozo, I. (2005). Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology. https://doi.org/10.1186/1471-2288-5-13.
Wells, G. A., Shea, B., O’Connell, D., Peterson, J., Welch, V., Losos, M., et al. (2010). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa: The Ottawa Health Research Institute.
The Cochrane Collaboration (2014). Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre.
Altman, D. G., & Bland, J. M. (1996). Detecting skewness from summary information. BMJ British Medical Journal, 313(7066), 1200.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care. https://doi.org/10.1097/01.MLR.0000062554.74615.4C.
Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. West Sussex: John Wiley & Sons Ltd.
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ British Medical Journal. https://doi.org/10.1136/bmj.327.7414.557.
*van Riel, C. A., Meijer-van den Bergh, E. E., Kemps, H. L., Feuth, T., Schreuder, H. W., Hoogerbrugge, P. M., et al. (2014). Self-perception and quality of life in adolescents during treatment for a primary malignant bone tumour. European Journal of Oncology Nursing. https://doi.org/10.1016/j.ejon.2014.01.005.
*Hijmans, C. T., Fijnvandraat, K., Oosterlaan, J., Heijboer, H., Peters, M., & Grootenhuis, M. A. (2010). Double disadvantage: A case control study on health-related quality of life in children with sickle cell disease. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-8-121.
*Morales, P. F., Sánchez-López, M., Moya-Martínez, P., García-Prieto, J. C., Martínez-Andrés, M., García, N. L., et al. (2013). Health-related quality of life, obesity, and fitness in schoolchildren: The Cuenca study. Quality of Life Research. https://doi.org/10.1007/s11136-012-0282-8.
*Moreira, H., Carona, C., Silva, N., Frontini, R., Bullinger, M., & Canavarro, M. C. (2013). Psychological and quality of life outcomes in pediatric populations: A parent-child perspective. The Journal of Pediatrics. https://doi.org/10.1016/j.jpeds.2013.06.028.
*Moreira, H., Frontini, R., Bullinger, M., & Canavarro, M. C. (2014). Family cohesion and health-related quality of life of children with type 1 diabetes: The mediating role of parental adjustment. Journal of Child and Family Studies. https://doi.org/10.1007/s10826-013-9758-6.
*Gouveia, M. J., Frontini, R., Canavarro, M. C., & Moreira, H. (2014). Quality of life and psychological functioning in pediatric obesity: The role of body image dissatisfaction between girls and boys of different ages. Quality of Life Research. https://doi.org/10.1007/s11136-014-0711-y.
*Muros, J. J., Salvador Pérez, F., Zurita Ortega, F., Gámez Sánchez, V. M., & Knox, E. (2017). The association between healthy lifestyle behaviors and health-related quality of life among adolescents. Jornal de Pediatria. https://doi.org/10.1016/j.jped.2016.10.005.
*Olaya Contreras, P., Bastidas, M., & Arvidsson, D. (2015). Colombian children with overweight and obesity need additional motivational support at school to perform health-enhancing physical activity. Journal of Physical Activity and Health. https://doi.org/10.1123/jpah.2014-0024.
*Ottova, V., Erhart, M., Rajmil, L., Dettenborn-Betz, L., & Ravens-Sieberer, U. (2012). Overweight and its impact on the health-related quality of life in children and adolescents: Results from the European KIDSCREEN survey. Quality of Life Research. https://doi.org/10.1007/s11136-011-9922-7.
*Bompori, E., Niakas, D., Nakou, I., Siamopoulou-Mavridou, A., & Tzoufi, M. S. (2014). Comparative study of the health-related quality of life of children with epilepsy and their parents. Epilepsy & Behavior. https://doi.org/10.1016/j.yebeh.2014.09.009.
*Zamani, G., Heidari, M., Azizi Malamiri, R., Ashrafi, M. R., Mohammadi, M., Shervin Badv, R., et al. (2016). The quality of life in boys with Duchenne muscular dystrophy. Neuromuscular Disorders. https://doi.org/10.1016/j.nmd.2016.05.004.
*Duarte, I., Santos, C. C., Rego, G., & Nunes, R. (2014). Health-related quality of life in children and adolescents with cochlear implants: Self and proxy reports. Acta Oto-Laryngologica. https://doi.org/10.3109/00016489.2014.930968.
*Janiec, I., Werner, B., Sieminska, J., & Ravens-Sieberer, U. (2011). Quality of life of children with mitral valve prolapse. Quality of Life Research. https://doi.org/10.1007/s11136-010-9780-8.
*Hedman, L., Stridsman, C., Andersson, M., Backman, H., Jansson, S. A., & Rönmark, E. (2017). Population-based study shows that teenage girls with asthma had impaired health-related quality of life. Acta Paediatrica. https://doi.org/10.1111/apa.13847.
*Jelenova, D., Prasko, J., Ociskova, M., Karaskova, E., Hunkova, M., Kolarova, J., et al. (2015). Quality of life in adolescents with inflammatory bowel disease and their parents: Comparison with healthy controls. Neuroendocrinology Letters, 36(8), 787–792.
*Myléus, A., Petersen, S., Carlsson, A., Hammarroth, S., Högberg, L., & Ivarsson, A. (2014). Health-related quality of life is not impaired in children with undetected as well as diagnosed celiac disease: A large population based cross-sectional study. BMC Public Health. https://doi.org/10.1186/1471-2458-14-425.
*Strinnholm, Å., Hedman, L., Winberg, A., Jansson, S. A., Lindh, V., & Rönmark, E. (2017). Health related quality of life among schoolchildren aged 12-13 years in relation to food hypersensitivity phenotypes: A population-based study. Clinical and Translational Allergy. https://doi.org/10.1186/s13601-017-0156-9.
*Fontecha, C. G., Balagué, F., Pellisé, F., Rajmil, L., Aguirre, M., Pasarín, M., et al. (2011). Low back pain in adolescents: Is quality of life poorer in those seeking medical attention? Spine. https://doi.org/10.1097/BRS.0b013e318203ed5b.
*Palmen, N. K., Zilkens, C., Rosenthal, D., Krauspe, R., Hefter, H., & Westhoff, B. (2014). Post-operative quality of life in children with severe perthes disease: Differences to matched controls and correlation with clinical function. Orthopedic Reviews. https://doi.org/10.4081/or.2014.5567.
*Dotis, J., Pavlaki, A., Printza, N., Stabouli, S., Antoniou, S., Gkogka, C., et al. (2016). Quality of life in children with chronic kidney disease. Pediatric Nephrology. https://doi.org/10.1007/s00467-016-3457-7.
*Amedro, P., Dorka, R., Moniotte, S., Guillaumont, S., Fraisse, A., Kreitmann, B., et al. (2015). Quality of life of children with congenital heart diseases: A multicenter controlled cross-sectional study. Pediatric Cardiology. https://doi.org/10.1007/s00246-015-1201-x.
*Sundell, A. L., Törnhage, C. J., & Marcusson, A. (2017). A comparison of health-related quality of life in 5- and 10-year-old Swedish children with and without cleft lip and/or palate. International Journal of Paediatric Dentistry. https://doi.org/10.1111/ipd.12253.
*Haraldstad, K., Christophersen, K. A., Eide, H., Nativg, G. K., & Helseth, S. (2011). Predictors of health-related quality of life in a sample of children and adolescents: A school survey. Journal of Clinical Nursing. https://doi.org/10.1111/j.1365-2702.2010.03693.x.
Schulte, F., Russell, K. B., Cullen, P., Embry, L., Fay-McClymont, T., Johnston, D., et al. (2017). Systematic review and meta-analysis of health-related quality of life in pediatric CNS tumor survivors. Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.26442.
Randa, H., Todberg, T., Skov, L., Larsen, L. S., & Zachariae, R. (2017). Health-related quality of life in children and adolescents with psoriasis: A systematic review and meta-analysis. Acta Dermato-Venereologica. https://doi.org/10.2340/00015555-2600.
Ul-Haq, Z., Mackay, D. F., Fenwick, E., & Pell, J. P. (2013). Meta-analysis of the association between body mass index and health-related quality of life among children and adolescents, assessed using the pediatric quality of life inventory index. The Journal of Pediatrics. https://doi.org/10.1016/j.jpeds.2012.07.049.
Silva, N., Carona, C., Crespo, C., & Canavarro, M. C. (2015). Quality of life in pediatric asthma patients and their parents: A meta-analysis on 20 years of research. Expert Review of Pharmacoeconomics & Outcomes. https://doi.org/10.1586/14737167.2015.1008459.
Zeller, M. H., & Modi, A. C. (2006). Predictors of health-related quality of life in obese youth. Obesity. https://doi.org/10.1038/oby.2006.15.
Barlow, J. H., & Ellard, D. R. (2006). The psychosocial well-being of children with chronic disease, their parents and siblings: An overview of the research evidence base. Child: Care, Health and Development. https://doi.org/10.1111/j.1365-2214.2006.00591.x.
Austin, J. K., Smith, M. S., Risinger, M. W., & McNelis, A. M. (1994). Childhood epilepsy and asthma: Comparison of quality of life. Epilepsia. https://doi.org/10.1111/j.1528-1157.1994.tb02481.x.
Pinquart, M., & Shen, Y. (2011). Behavior problems in children and adolescents with chronic physical illness: A meta-analysis. Journal of Pediatric Psychology. https://doi.org/10.1093/jpepsy/jsr042.
Silva, N., Bullinger, M., Moreira, H., Canavarro, M. C., & Carona, C. (2018). Establishing priorities for psychological interventions in pediatric settings: A decision-tree approach using the DISABKIDS-10 Index as a screening instrument. PLoS ONE. https://doi.org/10.1371/journal.pone.0198402.
Sattoe, J. N. T., van Staa, A., & Moll, H. A. (2012). The proxy problem anatomized: Child-parent disagreement in health related quality of life reports of chronically ill adolescents. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-10-10.
White-Koning, M., Arnaud, C., Dickinson, H. O., Thyen, U., Beckung, E., Fauconnier, J., et al. (2007). Determinants of child-parent agreement in quality-of-life reports: A European study of children with cerebral palsy. Pediatrics. https://doi.org/10.1542/peds.2006-3272.
Quitmann, J., Rohenkohl, A., Sommer, R., Bullinger, M., & Silva, N. (2016). Explaining parent-child (dis)agreement in generic and short stature-specific health-related quality of life reports: Do family and social relationships matter? Health and Quality of Life Outcomes. https://doi.org/10.1186/s12955-016-0553-0.
Silva, N., Crespo, C., Carona, C., Bullinger, M., & Canavarro, M. C. (2015). Why the (dis)agreement? Family context and child-parent perspectives on health-related quality of life and psychological problems in pediatric asthma. Child: Care, Health and Development. https://doi.org/10.1111/cch.12147.
Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ : British Medical Journal, 315(7109), 629–634.
Macaskill, P., Walter, S. D., & Irwig, L. (2001). A comparison of methods to detect publication bias in meta-analysis. Statistics in Medicine. https://doi.org/10.1002/sim.698.
Puhan, M. A., Soesilo, I., Guyatt, G. H., & Schünemann, H. J. (2006). Combining scores from different patient reported outcome measures in meta-analyses: When is it justified? Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-4-94.
Varni, J. W., Burwinkle, T. M., & Lane, M. M. (2005). Health-related quality of life measurement in pediatric clinical practice: An appraisal and precept for future research and application. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-3-34.
Acknowledgements
We would like to thank the authors of the original articles included in this meta-analysis, specifically to those who kindly supplied additional data upon our request: H. Moreira (Faculty of Psychology and Education Sciences, University of Coimbra, Portugal); L. Hedman (Department of Public Health and Clinical Medicine, Occupational and Environmental Medicine, The OLIN Unit, Umeå University; Department of Health Sciences, Division of Nursing, Luleå University of Technology, Sweden), and I. Duarte (Department of Community Medicine, Information and Health Decision Sciences, Faculty of Medicine, University of Porto, Portugal).
Funding
This study was funded by a Post-doctoral Fellowship (Grant No. SFRH/BPD/116841/2016) from the Portuguese Foundation for Science and Technology, and conducted at the Centre for Research in Neuropsychology and Cognitive Behavioral Intervention (CINEICC), Faculty of Psychology and Education Sciences of the University of Coimbra, and at the Department of Medical Psychology, University Medical Center Hamburg-Eppendorf.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was approved by the Scientific Council of the Faculty of Psychology and Education Sciences of the University of Coimbra. All studies included in this meta-analytic review were approved by their institutional and/or national ethical committees and were in accordance with the 1964 Helsinki Declaration and its subsequent amendments and with their national ethical and legal requirements, including parental informed consent and, for some studies, additional assent from the children.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Silva, N., Pereira, M., Otto, C. et al. Do 8- to 18-year-old children/adolescents with chronic physical health conditions have worse health-related quality of life than their healthy peers? a meta-analysis of studies using the KIDSCREEN questionnaires. Qual Life Res 28, 1725–1750 (2019). https://doi.org/10.1007/s11136-019-02189-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02189-7