Abstract
The epidemic characteristics of human immunodeficiency virus type 1 (HIV-1) in Zhejiang Province have not been systematically identified. This study presented a dynamic analysis of HIV-1 subtype variation in Zhejiang from 2004 to 2008, based on the surveillance of molecular epidemiology or drug resistance. CRF01_AE was the major strain (43.5 %) spreading across the province, second by B/B′ (17.9 %), CRF07_BC (17.1 %), and CRF08_BC (13.7 %). The strains were mainly transmitted by heterosexual contact. Novel recombinant strains and vertical transmission were occasionally reported. Floating population from other provinces accounted for a significant number of HIV-1 cases in Zhejiang. These data may provide us rational intervention strategy for further control of HIV dissemination.
Similar content being viewed by others
Introduction
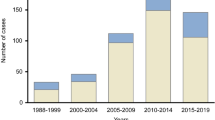
Zhejiang Province, located on the southeastern coast of China, is one of the first provinces to report a human immunodeficiency virus (HIV) cases in the mid-1980s, with four hemophiliacs infected with HIV-1 by contaminated Factor VIII [1]. From 1985 to 1996, 22 infections were identified among international travelers or commercial blood donors [2]. The initial local epidemic was confirmed in intravenous drug users (IDUs) and heterosexual contact population from 1997 to 2003. During that period, 479 HIV-1 infected individuals were reported covering more than 60 % of the cities in Zhejiang. The HIV-1 epidemic rapidly increased in the following years, which covered all of the cities in Zhejiang [3]. According to the statistics from Zhejiang Health Department, the accumulative numbers of identified HIV-infected individuals reached 10,355, and 3,853 of them progressed to acquired immunodeficiency syndromes (AIDS) by late 2013, with a mortality of 11.9 out of 100 patients per year. Despite the rapid spread of HIV-1, the dynamic changes of subtype variation remain unknown in Zhejiang.
In the present study, we reported a molecular epidemiological investigation in a subset of 451 HIV-1 seropositive individuals during 2004 to 2008 in Zhejiang. We tried to elucidate the characteristics of HIV-1 subtype and transmission here, for the purpose of disease control and epidemiology surveillance.
Materials and methods
Ethics statement
The study was reviewed and approved by the ethical review committee at Zhejiang Provincial Center of Disease Control and Prevention (Zhejiang CDC). All participants participated voluntarily in this study. Written informed consents were obtained from all involved participants in the study.
Participants and specimens
The study was conducted in a cross-sectional and anonymous manner in all 11 cities, based on the surveillance of molecular epidemiology or drug resistance. A total of 451 HIV-1-positive patient samples were collected by local CDC staff from 2004 to 2008 (Table 1). Data were collected using an interviewer-administered questionnaire [4]. Every participant was assigned a unique and confidential identifier code for the questionnaire and specimens. Demographic variables were collected including age, gender, ethnicity, transmission route, education, birth place, and current residence, etc. [5].
All blood samples originally tested by HIV antibody ELISA (Bio-Mérieux, France) at the local CDC were confirmed using Western-blot (Genelabs Diagnostics, Singapore) at Zhejiang CDC. 5 ml of EDTA-treated whole blood was taken from HIV-1 patient, and all samples were transferred to Zhejiang CDC in less than 12 h. The blood samples were separated into plasma and peripheral blood monocular cells (PBMC) and stored at −80 °C until use according to standard procedures.
Sequencing HIV-1 gag and pol gene fragments
Viral RNA was extracted from patient plasma (140 μl) using QIAamp Viral RNA Mini kit (Qiagen, USA). HIV-1 cDNA was obtained through RT-PCR using the Takara One Step RNA PCR kit (Takara, China) and then subjected to nested polymerase chain reaction (PCR) for the amplification of gag and pol gene fragments, as described previously [6, 7]. The portion of the gag gene p17–p24 region (HXB2, 836–1507 nt) [8–10] and the pol gene fragment (HXB2, 2147–3462 nt) [11, 12] were selected for PCR amplification and phylogenetic analyses. This study was based on the different surveillance of molecular epidemiology and drug resistance. PCR products were purified using Qiagen gel extraction kit, and sequenced using an automated ABI 377 DNA Sequencer (Applied Biosystems).
Phylogenetic analysis of HIV-1 sequences
The resulting gag or pol gene fragments were aligned with subtype reference sequences from the Los Alamos HIV database. Multiple alignments were made automatically using software BioEdit 7.0 with minor manual adjustments. Phylogenetic analysis of the aligned sequences was performed using MEGA 6.0 with maximum likelihood model and bootstrap testing (1000 replicates) [13]. Clusters of the sequences with bootstrap values above 70 % were considered significant for defining a subtype. The subtype of the sequences was proved by the online tool COMET HIV-1(http://comet.retrovirology.lu/index.php). Otherwise, we utilized online tool RIP 3.0 from LANL HIV database, or software Simplot 3.0 to check and ascertain the scattered or alien sequences for subtype or novel recombinant forms.
Results
Sociodemographic characteristics of HIV-1 patients in Zhejiang
The 451 HIV-1-seropositive individuals were followed up by Zhejiang CDC during 2004–2008. As shown in Table 1, the demographic characteristics of the cases are as follows: male (n = 287, 63.6 %), 30–49 years old (n = 236, 52.3 %), Han ethnicity (n = 393, 87.1 %), men who have sex with men (MSM, n = 47, 16.4 %), and less education (equal to or lower than middle school level, n = 343, 76.1 %). Among the 287 male patients, those that had heterosexual contact (n = 163, 56.8 %) or homosexual (n = 47, 16.4 %), or using intravenous drugs (n = 46, 16.0 %) accounted for the majority of the group. According to Table 1, a majority of female cases were infected through heterosexual contact (119 out of 164, 72.5 %), higher than the male ones.
Although using intravenous drugs was second to heterosexual contact, causing female infections, only 16 patients were in the drug user category. Five cases were diagnosed as infection through vertical and mother-to-child (MTC) transmission.
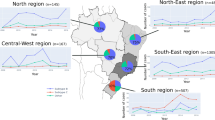
Geographically, 57.6 % (n = 260) of the HIV-1-positive patients were local residents from all 11 cities of the province. Except for the seven unknown cases, the remaining 40.8 % (n = 184) originally came from the other 23 provinces of China, including Yunnan (7.8 %, 35), Guangxi (7.3 %, 33), Sichuan (5.6 %, 25), Guizhou (5.3 %, 24), Henan (4.9 %, 22), Chongqing (3.3 %, 15), Anhui (4.2 %, 19), Jiangxi (2.4 %, 11), and others.
Distributions of HIV-1 subtypes in Zhejiang
During our molecular epidemiology study, the gag or env gene sequences were obtained. In drug resistance surveillance, only pol gene was harvested. Totally, 332 gag and 229 pol gene fragments were amplified and sequenced from the 451 individual samples, respectively (Supplementary files 1 and 2). Sequence analyses indicated that three HIV-1 subtypes (B/B’, C, and G), five circulating recombination forms (CRF01_AE, CRF07_BC, CRF08_BC, CRF02_AG, and CRF06_CPX), and some novel recombinant strains were detected. It was reported that the sensitivity and specificity among various subtyping tools might be different [14], all the sequences were checked again by the statistical-based tool COMET HIV. In consistence with Pineda-Pena’s results, we found only one sequence (2007_ZheJiang_HZ07ZJ191) which was evidence of CRF01_AE-CRF08_BC recombination, suggesting that the sensitivity and specificity were high for CRF01_AE subtyping between statistical-based and phylogenetic-based tools.
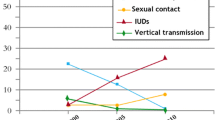
CRF01_AE was the major strain, infecting 196 cases (43.5 %), and it was mainly distributed through heterosexual contact. Then, subtype B/B’ (Thai-B) took second place, accounting for 17.9 %, dominant in blood transfusion. The CRF07_BC and CRF08_BC strains accounted for 17.1 and 13.7 % infections, respectively, mainly infecting patients through IDU (Figs. 1, 2). The rest strains (35 cases, 7.8 %) included CRF02_AG (8 cases), CRF06_CPX (2 case), subtype G (2 case), subtype C (10 cases), and 13 potentially novel recombinant strains (CRF07-CRF08, CRF01-C, and CRF01-B). With the epidemic progress, the population of CRF01_AE infection was prone to be expanded (Fig. 3).
Constitutes of HIV-1 subtypes or CRFs in Zhejiang from 2004 to 2008. The gag or pol gene fragments of 451 HIV-1 patients were amplified and sequenced. These sequences were then aligned to the subtyping reference sequences in the HIV databases (www.lanl.hiv.gov/index) and determined the HIV subtypes. The distribution of HIV-1 subtypes was shown in pie chart (Color figure online)
In other words, the results indicated that the major prevalent strains from 2004 to 2008 in Zhejiang Province were CRF01_AE, B/B’, CRF07_BC, and CRF08_BC, which comprised 92.2 % of the 451 total cases.
Dynamics of HIV-1 transmission in Zhejiang during 2004–2008
The study participants were mainly infected through heterosexual contact (n = 282, 62.5 %). Infections caused by intravenous drug use, MSM, blood transfusion, and MTC transmission accounted for only 62 (13.7 %), 47 (10.4 %), 30 (6.7 %), and 5 (1.1 %) cases, respectively. The transmission routes of other 25 cases could not be confirmed (Fig. 2). These results were consistent with the observations of our previous surveys, which indicated that the main transmission route was heterosexual contact in Zhejiang from 2004 to 2008 [15]. In recent years, with the increase of sexually transmitted cases, the disease raised awareness among MSM [16, 17]. Only two cases (2/25, 8.0 %) of MSM were reported for the first time in 2004. By 2008, the numbers of infection via homosexual individuals had slightly increased (14/116, 12.1 %), suggesting the possibility of expanded prevalence in the MSM population. Therefore, effective intervention measures should be taken to control the spread of HIV in this population.
The phylogenetic inference of HIV sequence
The phylogenetic tree was constructed according to the gag gene sequences in Zhejiang. The tree of CRF01_AE gag gene indicated that there was no obvious regional or time correlation, regardless of the original residence, sampling time or transmission routes (Fig. 4). And the distributions of CRF01_AE strains intermingled, which could be associated with the high population mobility in Zhejiang. Similar results were obtained with phylogenetic analysis of gag gene sequences of other subtypes, and pol gene sequences. Based on these observations, we speculated that imported HIV-1 infection cases played a significant role in the epidemic in Zhejiang, and more necessary attention should be paid to provide a rational intervention strategy against HIV dissemination.
Phylogenetic analysis of CRF01_AE gag gene sequences in Zhejiang. Total 149 of CRF01_AE gag sequences were analyzed with maximum likelihood method using MEGA 6.0. The statistical robustness of the tree and the reliability of the branching patterns are confirmed by bootstrapping (1000 replicates). Bootstrap values higher than 70 % are shown at branch node. CRF01_AE gag reference sequences. Sequences obtained from the immigrants to Zhejiang are in red color (Color figure online)
Discussion
After the first reported HIV-1 case in China in the mid-1980s, various subtypes and high diversity were reported in Zhejiang gradually. To date, eight subtypes or CRFs were identified in our study, and these strains were also reported to be circulating elsewhere [18–24].
CRF01_AE in our study was the dominant strain circulating in Zhejiang accounting for 43.5 % infection, across all transmission routes and with the trend of expansion. The CRF01_AE, which was originally identified in Thailand in 1989, appears to in major parts of Asia, particularly Southeast Asia [25, 26]. In China, CRF01_AE strains were first identified among persons at risk of sexual transmission and IDUs in the southwest provinces of Yunnan and Guangxi in the early 1990s [27–29].The Subsequent nationwide molecular epidemiological surveys in 1996–2002 indicated that the early spread of CRF01_AE was limited to the eastern coastal areas and southwest border provinces, predominantly in heterosexual populations [30, 31]. Phylogenetic analyses in Fig. 4 indicated the CRF01_AE sequences were intermingled, irrespective of the sampling regions, sampling years and transmission routes, and there were no close relationships or large sub-clusters with sequences. Therefore, it might be possible that the initial of CRF01_AE in Zhejiang could be the result of vastly increased international travel to and from China, starting in the early 1990s when the Chinese government began relaxing border restrictions to Chinese citizens for unofficial international travel. Meanwhile, we noticed that imported HIV infections outside Zhejiang and floating population comprised a significant percentage of the epidemic in the province. Local residents of Zhejiang accounted for approximately 57.6 % individuals, and floating population contributed to 40.8 % infections from other 23 provinces of China. Most cases (n = 282, 62.5 %) were infected through heterosexual contact in Zhejiang. Among them, 96 were diagnosed as residents outside Zhejiang, such as Yunnan, Guangxi, Guangdong where HIV-1 CRF01_AE has a high prevalence [32–34]. So there is another possibility that the floating population may function great to the epidemic increase, bringing strains to or from Zhejiang. However, the rare strains like CRF02_AG, G and CRF06_CPX mainly appeared in Zhoushan City, the settlement of native ocean-going fishermen who have traveled abroad for work.
In this study, we observed 13 novel recombinant strains including CRF07-CRF08, CRF01-B, and CRF01-C. So many different strains were co-circulating here, and some strains shuffled among different population or transmission routes. All these brought an ideal platform for super-infection and the descendants of novel recombinant strains.
Interestingly, we observed several vertical or transmission events were reported during these years. The population infected through MSM was gradually increased from 2004 to 2008 in Zhejiang. Otherwise, we observed some novel recombinant strains there. The newly expanded epidemic should be paid more attention and efficient measures should be taken to control the transmission.
Overall, the recent 5-years HIV-1 epidemic in Zhejiang was summarized in this study. The results revealed that CRF01_AE became the current major circulating strain and heterosexual contact was the major transmission route. High HIV-1 diversity was noted, which could be a factor that could accelerate this pandemic. The floating population contributed a great deal to the epidemic; therefore, intervention for this group should be a new focus of HIV prevention and control strategies. These data may be significant in further clarifying the AIDS epidemic.
References
D. Tang, G. Qu, X. Pang, Y. Lang, Y. Liang, Y. Yu, Y. Zeng, Y. Shao, Chin. Med. Sci. J. 8, 41–43 (1993)
J. Yao, J. Yang, J Chin AlDS/STD Prev Cont 6, 35–36 (2000)
Y. Xu, X. Pan, J. Yang, J. Zheng, L. Chen, Disease Surveillance 25, 877–890 (2010)
T. Zhang, J. Zhang, M. Gao, N. He, R. Detels, Eur J Public Health 22, 192–197 (2012)
X. Sun, N. Wang, D. Li, X. Zheng, S. Qu, L. Wang, F. Lu, K. Poundstone, L. Wang, Aids 21(Suppl 8), S33–S38 (2007)
L. Liao, H. Xing, X. Li, Y. Ruan, Y. Zhang, G. Qin, Y. Shao, AIDS Res. Hum. Retroviruses 23, 1062–1065 (2007)
Y.H. Song, Z.F. Meng, H. Xing, Y.H. Ruan, X.P. Li, R.L. Xin, P.F. Ma, H. Peng, Y. Shao, Arch. Virol. 152, 1553–1558 (2007)
H.A. Baird, R. Galetto, Y. Gao, E. Simon-Loriere, M. Abreha, J. Archer, J. Fan, D.L. Robertson, E.J. Arts, M. Negroni, Nucleic Acids Res. 34, 5203–5216 (2006)
A.E. Jetzt, H. Yu, G.J. Klarmann, Y. Ron, B.D. Preston, J.P. Dougherty, J. Virol. 74, 1234–1240 (2000)
K.S. Kemal, K. Anastos, B. Weiser, C.M. Ramirez, Q. Shi, H. Burger, AIDS Res. Hum. Retroviruses 29, 957–962 (2013)
Y. Zhang, L. Lu, L. Ba, L. Liu, L. Yang, M. Jia, H. Wang, Q. Fang, Y. Shi, W. Yan, G. Chang, L. Zhang, D.D. Ho, Z. Chen, PLoS Med 3, e443 (2006)
J. Zhuang, A.E. Jetzt, G. Sun, H. Yu, G. Klarmann, Y. Ron, B.D. Preston, J.P. Dougherty, J. Virol. 76, 11273–11282 (2002)
K. Tamura, D. Peterson, N. Peterson, G. Stecher, M. Nei, S. Kumar, Mol. Biol. Evol. 28, 2731–2739 (2011)
A.C. Pineda-Pena, N.R. Faria, S. Imbrechts, P. Libin, A.B. Abecasis, K. Deforche, A. Gomez-Lopez, R.J. Camacho, T. de Oliveira, A.M. Vandamme, Infect Genet Evol 19, 337–348 (2013)
X. Pan, Y. Yao, S. Xia, J. Yang, Z. Guo, Chin J AIDS STD 13, 308–310 (2007)
M.D. Durham, K. Buchacz, J. Richardson, D. Yang, K. Wood, B. Yangco, J.T. Brooks, J. Acquir. Immune Defic. Syndr. 63, 372–378 (2013)
Klavs I., Bergant N., Kastelic Z., Lamut A., and Kustec T., Euro Surveill 14, 2009
J.H. Chen, K.H. Wong, Z. Chen, K. Chan, H.Y. Lam, S.W. To, V.C. Cheng, K.Y. Yuen, W.C. Yam, PLoS ONE 5, e12198 (2010)
S. Kanwal, T. Mahmood, ScientificWorldJournal 2012, 978917 (2012)
H.F. Njai, Y. Gali, G. Vanham, C. Clybergh, W. Jennes, N. Vidal, C. Butel, E. Mpoudi-Ngolle, M. Peeters, K.K. Arien, Retrovirology 3, 40 (2006)
P. Seth, Indian J. Virol. 21, 3–7 (2010)
K.K. Tee, O.G. Pybus, X.J. Li, X. Han, H. Shang, A. Kamarulzaman, Y. Takebe, J. Virol. 82, 9206–9215 (2008)
U. Neogi, I. Bontell, A. Shet, A. De Costa, S. Gupta, V. Diwan, R.S. Laishram, A. Wanchu, U. Ranga, A.C. Banerjea, A. Sonnerborg, PLoS ONE 7, e39819 (2012)
J. Yan, S. Xiao, L. Zhou, Y. Tang, G. Xu, D. Luo, Q. Yi, AIDS Care 25, 302–308 (2013)
C.Y. Ou, Y. Takebe, B.G. Weniger, C.C. Luo, M.L. Kalish, W. Auwanit, S. Yamazaki, H.D. Gayle, N.L. Young, G. Schochetman, Lancet 341, 1171–1174 (1993)
K.A. Lau, B. Wang, N.K. Saksena, AIDS Rev 9, 218–229 (2007)
H. Liao, K.K. Tee, S. Hase, R. Uenishi, X.J. Li, S. Kusagawa, P.H. Thang, N.T. Hien, O.G. Pybus, Y. Takebe, Virology 391, 51–56 (2009)
J. Chen, N.L. Young, S. Subbarao, P. Warachit, S. Saguanwongse, S. Wongsheree, C. Jayavasu, C.C. Luo, T.D. Mastro, AIDS Res. Hum. Retroviruses 15, 81–84 (1999)
H. Cheng, J. Zhang, J. Capizzi, N.L. Young, T.D. Mastro, Lancet 344, 953–954 (1994)
H. Xing, P. Pan, L. Su, X. Fan, Y. Feng, L. Qiang, Y. Shao, Zhongguo Xing Bing Ai Zi Bing Fang Zhi 8, 200–203 (2002)
Xing H., Liang H., Wan Z., Chen X., Wei M., Ma P., and Shao Y., Zhonghua Yu Fang Yi Xue Za Zhi, 300-304, 2004
J.T. Lau, H.Y. Tsui, J. Gu, J. Zhang, L. Zhang, Y. Zhang, F. Cheng, N. Wang, AIDS Behav. 15, 86–94 (2011)
L. Li, G. Sun, S. Liang, J. Li, T. Li, Z. Wang, W. Liu, S. Yang, Y. Liu, X. Wang, PLoS ONE 8, e75777 (2013)
W. Ma, R. Detels, Y. Feng, Z. Wu, L. Shen, Y. Li, Z. Li, F. Chen, A. Wang, T. Liu, AIDS 21(8), S129–S135 (2007)
Acknowledgments
We gratefully acknowledge the contributions of the HIV-1 patients who participated in this study and also thank the staff of Zhejiang and the local CDC for recruiting participants, collecting the samples, and technical assistance. The HIV sequences are accessible in GenBank from KJ613998 to KJ614226 (Pol) and from KJ613666to KJ613997 (Gag).
Funding
This work was supported by the foundation of The Health Department of Zhejiang Province (2012KYB054) and in part by NSFC Grant (81101257). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interests
The authors have declared that no competing interests exist.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yao, Y., Xin, R., Yang, J. et al. Trends of subtype variation of human immunodeficiency virus type 1 in Zhejiang Province, China. Virus Genes 50, 22–28 (2015). https://doi.org/10.1007/s11262-014-1136-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11262-014-1136-y