Abstract
Purpose
The primary objectives of this study were to assess the safety of [18F]flutemetamol injection and determine the level of association between the quantitative estimates of brain uptake of [18F]flutemetamol and the quantitative immunohistochemical (IHC) estimates of amyloid levels in cerebral cortex biopsies obtained during shunt placement in patients with normal pressure hydrocephalus (NPH).
Procedures
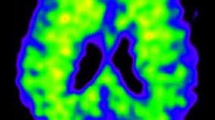
Parietal lobe biopsies were obtained from 12 subjects (mean (SD), 71 (8.1) years), during shunt placement for NPH. Shunt procedures and biopsies were performed within 8 weeks after the positron emission tomography (PET) imaging, and followed by a computed tomography scan.
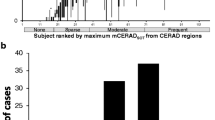
The quantitative estimates of the brain uptake of [18F]flutemetamol (standard uptake value ratios (SUVRs)) from the biopsy site, contralateral to the biopsy site, and composite were made from the analysis of PET images. The quantitative IHC levels of amyloid load were estimated using a monoclonal antiamyloid β antibody, 4 G8 (in percent area), as the standard of truth (N = 8, of which 5 had full histopathology staining). The primary analysis determined the level of association between the SUVR (with cerebellum as the reference region) from the biopsy site, and the level of amyloid was determined from IHC estimates of amyloid in the biopsy sample.
Results
[18F]Flutemetamol injection was found to be well tolerated. The biopsied area well represented the amyloid deposition throughout the cortex in this small sample. The biopsy site SUVR was significantly correlated with the biopsy specimen amyloid β level (expressed as percent of biopsy specimen area staining with 4 G8). The full model was significant (p = 0.0174). In the secondary efficacy analyses, contralateral (to biopsy site) and composite SUVR values correlated significantly with the percent of biopsy specimen staining for amyloid β based on 4 G8. Blinded visual [18F]flutemetamol image interpretations showed a sensitivity of 100 % and a specificity of 100 % with pathology reads staining for amyloid plaque with Bielschowsky and thioflavin S and overall pathology read. The results of the blinded reader agreement for [18F]flutemetamol PET showed full agreement among three readers.
Conclusions
PET imaging of NPH patients following the administration of [18F]flutemetamol injection was highly correlated with the presence of fibrillar amyloid β in subsequent cortical biopsy samples in this small sample. Administration of [18F]flutemetamol injection was well tolerated.



Similar content being viewed by others
References
Chong MS, Sahadevan S (2005) Preclinical Alzheimer's disease: diagnosis and prediction of progression. Lancet Neurol 4:576–579
Grober E, Dickson D, Sliwinski MJ et al (1999) Memory and mental status correlates of modified Braak staging. Neurobiol Aging 20:573–579
Braak H, Braak E (1991) Neuropathological staging of Alzheimer's disease. Acta Neuropathol (Berl) 82:239–259
Gómez-Isla T, Hollister R, West H et al (1997) Neuronal loss correlates with but exceeds neurofibrillary tangles in Alzheimer's disease. Ann Neurol 41:17–24
Arriagada PV, Growdon JH, Hedley-Whyte ET et al (1992) Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer's disease. Neurology 42:631–639
Cotran RS, Kumar V, Robbins SL (1989) Alzheimer's disease in: the nervous system. In: Cotran RS, Kumar V, Robbins SL (eds) Robbins pathologic basis of disease. 4th Edn. chapter 29. Saunders, Philadelphia. pp 1427–1429.
Vallet PG, Guntern R, Hof PR (1992) A comparative study of histological and immunohistochemical methods for neurofibrillary tangles and senile plaques in Alzheimer's disease. Acta Neuropahol 83(2):170–178
DeGrado TR, Turkington TG, Williams JJ et al (1994) Performance characteristics of a whole-body PET scanner. J Nucl Med 35(8):1398–1406
Yamamoto T, Hirano A (1986) A comparative study of modified Bielschowsky, Bodian and thioflavin S stains on Alzheimer's neurofibrillary tangles. Neuropathol Appl Neurobiol 12:3–9
Mirra SS, Heyman A, McKeel D et al (1991) The consortium to establish a registry for Alzheimer's disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer's disease. Neurology 41(4):479–486
Jack CR Jr, Lowe VJ, Senjem ML et al (2008) 11 C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment. Brain 131:665–680
Jack CR Jr, Wiste HJ, Vemuri P et al (2010) Brain beta-amyloid measures and magnetic resonance imaging atrophy both predict time-to-progression from mild cognitive impairment to Alzheimer's disease. Brain 133(11):3336–3348
Raji CA, Backer JT, Nicholas D et al (2008) Characterizing regional correlation, laterality and symmetry of amyloid deposition in mild cognitive impairment and Alzheimer's disease with Pittsburgh compound B. J Neurosci Methods 172:277–282
Menon KV, Gomez D, Smith AM, et al. (2009) Impact of margin status on survival following pancreatoduodenectomy for cancer: the Leeds pathology protocol (LEEPP) 11(1): 18–24.
Rossetti HC, Munro CC, Hynan LS et al (2010) The CERAD neuropsychologic battery total score and the progression of Alzheimer disease. Alzheimer Dis Assoc Disord 24(2):138–142
Leinonen V, Alafuzoff I, Aalto S et al (2008) Assessment of β-amyloid in a frontal cortical brain biopsy specimen and by positron emission tomography with carbon 11-labeled Pittsburgh compound B. Arch Neurol 65(10):1304–1309
Wolk DA, Grachev ID, Buckley C et al (2011) Association between in vivo fluorine 18-labeled flutemetamol amyloid positron emission tomography imaging and in vivo cerebral cortical histopathology. Arch Neurol 68(11):1398–1403
Price JL, Morris JC (1999) Tangles and plaques in nondemented aging and preclinical Alzheimer's disease. Ann Neurol 45:358–368
Clark CM, Schneider JA, Bedell BJ, AV45–A07 Study Group et al (2011) Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA 305(3):275–283
Wong DF, Rosenberg PB, Zhou Y, et al. (2010) In vivo imaging of amyloid deposition in Alzheimer disease using the radioligand 18F-AV-45 (florbetapir F 18). J Nucl Med. 2010 Jun;51(6):913–20. Erratum in: J Nucl Med. 2010 51(8):1327.
Acknowledgments
We thank all the patients and their relatives for their participation in the study. The referring physicians and the staff of Johns Hopkins Medical Institution are gratefully acknowledged. We acknowledge the staff of the i3 Statprobe, USA, for the biometric services, programming, and statistical analyses (funded by GE Healthcare). The authors wish to thank all involved GE Healthcare study team members for the operational support, data programming, and statistical management and to Andrew Crabb and Emily Gean, PhD of JHU SOM for their technical assistance with the manuscript preparation.
Funding
The study was entirely sponsored by GE Healthcare.
Conflict of interest
Igor D. Grachev and Paul Sherwin work for GE Healthcare, Princeton, NJ and Chris Buckley and Adrian Smith work for GE Healthcare, Amersham, UK. Chris Buckley, Adrian Smith, Paul Sherwin, and Igor D Grachev are employees of GE Healthcare. There are no other conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, D.F., Moghekar, A.R., Rigamonti, D. et al. An In Vivo Evaluation of Cerebral Cortical Amyloid with [18F]Flutemetamol Using Positron Emission Tomography Compared with Parietal Biopsy Samples in Living Normal Pressure Hydrocephalus Patients. Mol Imaging Biol 15, 230–237 (2013). https://doi.org/10.1007/s11307-012-0583-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-012-0583-x