Abstract
Purpose
The aim of this study was to determine the physiological and pathophysiological biodistribution of [68Ga]PSMA-HBED-CC (PSMA-11) ([68Ga]PSMA) in patients with prostate cancer (PCA) to establish the range of normal uptake in relevant organs and primary prostate tumours, locally recurrent PCA, lymph and bone metastases and other metastatic lesions. Additionally, we aimed to determine a cut-off uptake value for differentiation of primary tumours from normal prostate tissue.
Procedures
Overall, [68Ga]PSMA positron emission tomography/x-ray computed tomography (PET/CT) of 101 patients (mean age 69.1 years) with PCA was analysed retrospectively. For assessment of tracer biodistribution, maximum standardized uptake values (SUVmax) were calculated for various normal organs, as well as for primary tumours (PT) and/or metastases. Results are presented as median, interquartile range (IQR; 25th quantil–75th quantil) and range (minimum–maximum).
Results
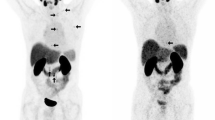
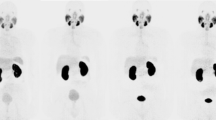
[68Ga]PSMA PET/CT was performed 50 min (range 30–126) after injection of 109 MBq (range 84–158). Regarding biodistribution, highest uptake (median/IQR/range) of the tracer was found in the kidneys (49.6/40.7–57.6/2.7–97.0) followed by the submandibular glands (17.3/13.7–21.2/7.5–30.4), parotid glands (16.1/12.2–19.8/5.5–30.9) and duodenum (13.8/10.5–17.2/5.8–26.9). The best cut-off value for differentiating physiological uptake in the primary tumour from that in the prostate was found to be an SUVmax of 3.2. The median SUVmax in the PT (n = 35), locally recurrent PCA (n = 8), lymph node (n = 166), bone (n = 157) and other metastases (n = 3) were 10.2, 5.9, 6.2, 7.4 and 3.8, respectively. The best cut-off values for differentiating non-pathological uptake in lymph nodes and bones from tumour uptake were found to be SUVmax of 3.2 and 1.9, respectively. Patients with PSA <2 had significantly lower SUVmax in bone metastases as compared to patients with PSA ≥2 (p < 0.01).
Conclusions
This biodistribution study provided a broad range of uptake data of [68Ga]PSMA-11 for normal organs/tissues, primary prostate tumours and metastatic lesions based on a large patient cohort. Both PT and small metastatic lesions were detectable due to their high tracer uptake. Four-times-higher median uptake in PT in comparison to normal prostate stroma resulted in a high diagnostic accuracy that could potentially be used for multimodal image-guided biopsy with dedicated reconstruction software.






Similar content being viewed by others
References
Jemal A, Siegel R, Ward E et al (2009) Cancer statistics, 2009. CA Cancer J Clin 59:225–249
Draisma G, Etzioni R, Tsodikov A et al (2009) Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst 101:374–383
Etzioni R, Penson DF, Legler JM et al (2002) Overdiagnosis due to prostate-specific antigen screening: lessons from U.S. prostate cancer incidence trends. J Natl Cancer Inst 94:981–990
Schwarzenbock S, Souvatzoglou M, Krause BJ (2012) Choline PET and PET/CT in primary diagnosis and staging of prostate cancer. Theranostics 2:318–330
Ackerstaff E, Glunde K, Bhujwalla ZM (2003) Choline phospholipid metabolism: a target in cancer cells? J Cell Biochem 90:525–533
Casciani E, Gualdi GF (2006) Prostate cancer: value of magnetic resonance spectroscopy 3D chemical shift imaging. Abdom Imaging 31:490–499
von Eyben FE, Kairemo K (2014) Meta-analysis of (11)C-choline and (18)F-choline PET/CT for management of patients with prostate cancer. Nucl Med Comm 35:221–230
Silver DA, Pellicer I, Fair WR et al (1997) Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res 3:81–85
Afshar-Oromieh A, Malcher A, Eder M et al (2013) PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging 40:486–495
Bandekar A, Zhu C, Jindal R et al (2014) Anti-prostate-specific membrane antigen liposomes loaded with 225Ac for potential targeted antivascular alpha-particle therapy of cancer. J Nucl Med 55:107–114
Banerjee SR, Pullambhatla M, Foss CA et al (2014) 64Cu-labeled inhibitors of prostate-specific membrane antigen for PET imaging of prostate cancer. J Med Chem 57:2657–2669
Tagawa ST, Milowsky MI, Morris M et al (2013) Phase II study of Lutetium-177-labeled anti-prostate-specific membrane antigen monoclonal antibody J591 for metastatic castration-resistant prostate cancer. Clin Cancer Res 19:5182–5191
Zechmann CM, Afshar-Oromieh A, Armor T et al (2014) Radiation dosimetry and first therapy results with a 124I/ 131I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur J Nucl Med Mol Imaging 41:1280–1292
Eder M, Eisenhut M, Babich J, Haberkorn U (2013) PSMA as a target for radiolabelled small molecules. Eur J Nucl Med Mol Imaging 40:819–823
Afshar-Oromieh A, Zechmann CM, Malcher A et al (2014) Comparison of PET imaging with a 68Ga-labelled PSMA ligand and 18F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 41:11–20
Dietlein M, Kobe C, Kuhnert G et al (2015) Comparison of [18F]DCFPyL and [68Ga]Ga-PSMA-HBED-CC for PSMA-PET imaging in patients with relapsed prostate cancer. Mol Imaging Biol 17:575–584
Szabo Z, Mena E, Rowe SP et al (2015) Initial evaluation of [18F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol 17:565–574
Surti S, Kuhn A, Werner ME et al (2007) Performance of Philips Gemini TF PET/CT scanner with special consideration for its time-of-flight imaging capabilities. J Nucl Med 48:471–480
Yao V, Berkman CE, Choi JK et al (2010) Expression of prostate-specific membrane antigen (PSMA), increases cell folate uptake and proliferation and suggests a novel role for PSMA in the uptake of the non-polyglutamated folate, folic acid. Prostate 70:305–316
Bostwick DG, Pacelli A, Blute M et al (1998) Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer 82:2256–2261
Su SL, Huang IP, Fair WR et al (1995) Alternatively spliced variants of prostate-specific membrane antigen RNA: ratio of expression as a potential measurement of progression. Cancer Res 55:1441–1443
Human protein atlas FOLH1. http://www.proteinatlas.org/ENSG00000086205-FOLH1/tissue
Kawakami M, Nakayama J (1997) Enhanced expression of prostate-specific membrane antigen gene in prostate cancer as revealed by in situ hybridization. Cancer Res 57:2321–2324
Carter RE, Feldman AR, Coyle JT (1996) Prostate-specific membrane antigen is a hydrolase with substrate and pharmacologic characteristics of a neuropeptidase. Proc Natl Acad Sci U S A 93:749–753
Pinto JT, Suffoletto BP, Berzin TM et al (1996) Prostate-specific membrane antigen: a novel folate hydrolase in human prostatic carcinoma cells. Clin Cancer Res 2:1445–1451
Tiffany CW, Lapidus RG, Merion A et al (1999) Characterization of the enzymatic activity of PSM: comparison with brain NAALADase. Prostate 39:28–35
Lapidus RG, Tiffany CW, Isaacs JT, Slusher BS (2000) Prostate-specific membrane antigen (PSMA) enzyme activity is elevated in prostate cancer cells. Prostate 45:350–354
Durmus T, Baur A, Hamm B (2014) Multiparametric magnetic resonance imaging in the detection of prostate cancer. RöFo 186:238–246
Pasoglou V, Larbi A, Collette L et al (2014) One-step TNM staging of high-risk prostate cancer using magnetic resonance imaging (MRI): toward an upfront simplified "all-in-one" imaging approach? Prostate 74:469–477
Afshar-Oromieh A, Haberkorn U, Schlemmer HP et al (2014) Comparison of PET/CT and PET/MRI hybrid systems using a 68Ga-labelled PSMA ligand for the diagnosis of recurrent prostate cancer: initial experience. Eur J Nucl Med Mol Imaging 41:887–897
Kuhner G, Boellaard R, Sterzer S et al (2016) Impact of PET/CT image reconstruction methods and liver uptake normalization strategies on quantitative image analysis. Eur J Nucl Med Mol Imaging 43:249–258
Authors’ Contribution
Vikas Prasad and Ingo G. Steffen contributed equally in writing, conceptualizing, editing and analysing the results. Gerd Diederichs, Marcus M. Makowski and Peter Wust wrote part of the manuscript and also edited it. Winfried Brenner helped in writing and editing as well as in analysing the results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The retrospective analyses were performed in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed Consent
Informed consent was obtained from all the patients.
Rights and permissions
About this article
Cite this article
Prasad, V., Steffen, I.G., Diederichs, G. et al. Biodistribution of [68Ga]PSMA-HBED-CC in Patients with Prostate Cancer: Characterization of Uptake in Normal Organs and Tumour Lesions. Mol Imaging Biol 18, 428–436 (2016). https://doi.org/10.1007/s11307-016-0945-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-016-0945-x