Abstract
Background
Identifying the sites of obstruction of the upper airway in patients with obstructive sleep apnea-hypopnea syndrome (OSAHS) is paramount for surgical planning. The aim of this study is to compare wake physical exam findings to the ones obtained during drug-induced sedation endoscopy (DISE) in the diagnosis of severe collapse of the upper airway in OSAHS patients.
Methods
A retrospective chart review of OSAHS patients who underwent DISE at our institution during the 2006–2010 period was conducted. All the patients had previously undergone a physical examination that included modified Mallampati index (MMI), the Müller maneuver (MM), and the Friedman staging system. Level and severity of airway collapse were evaluated. A severe collapse was attributed to obstructions equal or greater than 75 % of the airway.
Results
A total of 138 patients were included in the study. The incidence of severe airway collapse was compared between DISE and MM; at retropalatal level, no significant difference was found. At retrolingual level, 69 % of patients had severe collapse with DISE in comparison to a 28 % with the MM (p < 0.05). No relationship was found either with the MMI or with the Friedman staging system when compared to the incidence of severe retrolingual collapse diagnosed by DISE. Concordance was low between awake and DISE exploration in both retropalatal and retroglossal level.
Conclusion
The Müller maneuver underestimates tongue base severe obstruction diagnosis when compared to that obtained after DISE in OSAHS patients. The wake patient exploration does not accurately correlate to DISE exploration.


Similar content being viewed by others
References
Young T, Finn L (1998) Epidemiological insights into the public health burden of sleep disordered breathing: sex differences in survival among sleep clinic patients. Thorax 53(Suppl 3):S16–S19
Peppard PE, Young T, Barnet JH et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. doi:10.1093/aje/kws342
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90:47–112. doi:10.1152/physrev.00043.2008
Young T, Finn L, Peppard PE et al (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Young T, Palta M, Dempsey J et al (2009) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ Off Publ State Med Soc Wisconsin 108:246–249
Weaver TE (2013) Don’t start celebrating—CPAP adherence remains a problem. J Clin Sleep Med 9:551–552. doi:10.5664/jcsm.2746
Weaver TE, Maislin G, Dinges DF et al (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30:711–719
Pieters T, Collard P, Aubert G et al (1996) Acceptance and long-term compliance with nCPAP in patients with obstructive sleep apnoea syndrome. Eur Respir J 9:939–944
Richard W, Venker J, den Herder C et al (2007) Acceptance and long-term compliance of nCPAP in obstructive sleep apnea. Eur Arch Otorhinolaryngol 264:1081–1086. doi:10.1007/s00405-007-0311-3
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Caples SM, Rowley JA, Prinsell JR et al (2010) Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep 33:1396–1407
Sundaram S, Lim J, TJ L (2005) Surgery for obstructive sleep apnoea in adults. Cochrane Database Syst Rev Art. No.: CD001004. doi: 10.1002/14651858.CD001004.pub2
Friedman M, Tanyeri H, La Rosa M et al (1999) Clinical predictors of obstructive sleep apnea. Laryngoscope 109:1901–1907. doi:10.1097/00005537-199912000-00002
Friedman M, Ibrahim H, Joseph NJ (2004) Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope 114:454–459. doi:10.1097/00005537-200403000-00013
Pang KP, Terris DJ, Podolsky R (2006) Severity of obstructive sleep apnea: correlation with clinical examination and patient perception. Otolaryngol Head Neck Surg 135:555–560. doi:10.1016/j.otohns.2006.03.044
Ko M-T, Su C-Y (2008) Computer-assisted quantitative evaluation of obstructive sleep apnea using digitalized endoscopic imaging with Muller maneuver. Laryngoscope 118:909–914. doi:10.1097/MLG.0b013e3181638187
Gregório MG, Jacomelli M, Figueiredo AC et al (2007) Evaluation of airway obstruction by nasopharyngoscopy: comparison of the Müller maneuver versus induced sleep. Braz J Otorhinolaryngol 73:618–622
Croft CB, Pringle M (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 16:504–509
De Vito A, Carrasco Llatas M, Vanni A et al (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18:453–465. doi:10.1007/s11325-014-0989-6
Rabelo FAW, Braga A, Küpper DS et al (2010) Propofol-induced sleep: polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol Head Neck Surg 142:218–224. doi:10.1016/j.otohns.2009.11.002
Abdullah VJ, Lee DLY, Ha SCN, van Hasselt CA (2013) Sleep endoscopy with midazolam: sedation level evaluation with bispectral analysis. Otolaryngol Head Neck Surg 148:331–337. doi:10.1177/0194599812464865
Berry S, Roblin G, Williams A et al (2005) Validity of sleep nasendoscopy in the investigation of sleep related breathing disorders. Laryngoscope 115:538–540. doi:10.1097/01.mlg.0000157849.16649.6e
Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ (2009) Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 140:646–651. doi:10.1016/j.otohns.2009.01.012
Kezirian EJ, White DP, Malhotra A et al (2010) Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg 136:393–397. doi:10.1001/archoto.2010.26
Vroegop AVMT, Vanderveken OM, Wouters K et al (2013) Observer variation in drug-induced sleep endoscopy: experienced versus nonexperienced ear, nose, and throat surgeons. Sleep 36:947–953. doi:10.5665/sleep.2732
Hewitt RJD, Dasgupta A, Singh A et al (2009) Is sleep nasendoscopy a valuable adjunct to clinical examination in the evaluation of upper airway obstruction? Eur Arch Otorhinolaryngol 266:691–697. doi:10.1007/s00405-008-0831-5
Hessel NS, de Vries N (2003) Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol 260:91–95. doi:10.1007/s00405-002-0511-9
Vanderveken OM, Maurer JT, Hohenhorst W et al (2013) Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med 9:433–438. doi:10.5664/jcsm.2658
Blumen MB, Latournerie V, Bequignon E et al (2015) Are the obstruction sites visualized on drug-induced sleep endoscopy reliable? Sleep Breath. Sleep Breath 19:1021--6
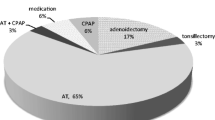
Carrasco Llatas M, Dalmau Galofre J, López Martínez R et al (2005) Our findings in the sleep endoscopy exams. Acta Otorrinolaringol Esp 56:17–21. doi:10.1016/S0001-6519(05)78564-2
Rabelo FAW, Küpper DS, Sander HH et al (2013) A comparison of the Fujita classification of awake and drug-induced sleep endoscopy patients. Braz J Otorhinolaryngol 79:100–105. doi:10.5935/1808-8694.20130017
Soares D, Folbe AJ, Yoo G et al (2013) Drug-induced sleep endoscopy vs awake Müller’s maneuver in the diagnosis of severe upper airway obstruction. Otolaryngol Head Neck Surg 148:151–156. doi:10.1177/0194599812460505
Pringle MB, Croft CB (1991) A comparison of sleep nasendoscopy and the Muller manoeuvre. Clin Otolaryngol Allied Sci 16:559–562
Campanini A, Canzi P, De Vito A et al (2010) Awake versus sleep endoscopy: personal experience in 250 OSAHS patients. Acta Otorhinolaryngol Ital 30:73–77
Cavaliere M, Russo F, Iemma M (2013) Awake versus drug-induced sleep endoscopy: evaluation of airway obstruction in obstructive sleep apnea/hypopnoea syndrome. Laryngoscope 123:2315–2318. doi:10.1002/lary.23881
Den Herder C, van Tinteren H, de Vries N (2005) Sleep endoscopy versus modified Mallampati score in sleep apnea and snoring. Laryngoscope 115:735–739. doi:10.1097/01.mlg.0000161347.07881.6d
Aktas O, Erdur O, Cirik AA, Kayhan FT (2015) The role of drug-induced sleep endoscopy in surgical planning for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 272:2039–2043. doi:10.1007/s00405-014-3162-8
Kavcic P, Koren A, Koritnik B et al (2015) Sleep magnetic resonance imaging with electroencephalogram in obstructive sleep apnea syndrome. Laryngoscope 125:1485–1490. doi:10.1002/lary.25085
Maurer JT (2006) Current diagnostic trends in sleep disordered breathing. GMS Curr Top Otorhinolaryngol Head Neck Surg 5:Doc02
Safiruddin F, Vanderveken OM, de Vries N, et al. (2015) Effect of upper-airway stimulation for obstructive sleep apnoea on airway dimensions. Eur Respir J 45 (1): 129:38. doi: 10.1183/09031936.00059414
Rabelo FAW, Küpper DS, Sander HH et al (2013) Polysomnographic evaluation of propofol-induced sleep in patients with respiratory sleep disorders and controls. Laryngoscope 123:2300–2305. doi:10.1002/lary.23664
Carrasco Llatas M, Dalmau Galofre J, Zerpa Zerpa V et al (2014) Drug-induced sleep videoendoscopy: clinical usefulness and literature review. Acta Otorrinolaringol Esp 65:183–190. doi:10.1016/j.otorri.2013.06.004
Hillman DR, Walsh JH, Maddison KJ et al (2009) Evolution of changes in upper airway collapsibility during slow induction of anesthesia with propofol. Anesthesiology 111:63–71. doi:10.1097/ALN.0b013e3181a7ec68
Hoshino Y, Ayuse T, Kurata S et al (2009) The compensatory responses to upper airway obstruction in normal subjects under propofol anesthesia. Respir Physiol Neurobiol 166:24–31
Genta PR, Eckert DJ, Gregorio MG et al (2011) Critical closing pressure during midazolam-induced sleep. J Appl Physiol 111:1315–1322. doi:10.1152/japplphysiol.00508.2011
Hong SD, Dhong H-JJ, Kim HY et al (2013) Change of obstruction level during drug-induced sleep endoscopy according to sedation depth in obstructive sleep apnea. Laryngoscope 123:2896–2899. doi:10.1002/lary.24045
Heo SJ, Park CM, Kim JS (2014) Time-dependent changes in the obstruction pattern during drug-induced sleep endoscopy. Am J Otolaryngol 35:42–47. doi:10.1016/j.amjoto.2013.08.017
Ravesloot MJL, De Vries N (2011) One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope 121:2710–2716. doi:10.1002/lary.22369
Vroegop AV, Vanderveken OM, Boudewyns AN et al (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope 124:797–802. doi:10.1002/lary.24479
Soares D, Sinawe H, Folbe AJ et al (2012) Lateral oropharyngeal wall and supraglottic airway collapse associated with failure in sleep apnea surgery. Laryngoscope 122:473–479. doi:10.1002/lary.22474
Koutsourelakis I, Safiruddin F, Ravesloot M et al (2012) Surgery for obstructive sleep apnea: sleep endoscopy determinants of outcome. Laryngoscope 122:2587–2591. doi:10.1002/lary.23462
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zerpa Zerpa, V., Carrasco Llatas, M., Agostini Porras, G. et al. Drug-induced sedation endoscopy versus clinical exploration for the diagnosis of severe upper airway obstruction in OSAHS patients. Sleep Breath 19, 1367–1372 (2015). https://doi.org/10.1007/s11325-015-1266-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1266-z