Abstract
Purpose
The pressures delivered by autotitrating continuous positive airways pressure (CPAP) devices not only treat obstructive sleep apnoea (OSA) effectively but also give potentially interesting physiological information about the forces impinging on the pharynx. In earlier work from this unit, we used correlations between autoCPAP pressure and both OSA severity and obesity, to construct an algorithm to estimate the fixed CPAP pressure a patient required for subsequent clinical use. We wished to discover if these relationships could be reliably extended to a much more obese group.
Methods
We performed a prospective cohort study in an obese population. Measurements of obesity were made, OSA severity was recorded, and the 95th centile autoCPAP pressure was recorded during 1 week of autoCPAP. Spearman’s rank correlation was performed between measurements of obesity and autoCPAP pressure, and between OSA severity and autoCPAP pressure.
Results
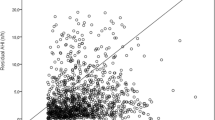
Fifty-four obese individuals (median body mass index (BMI) 43.0 kg/m2), 52 % of whom had OSA (apnoea-hypopnoea index (AHI) ≥ 15), had a median 95th centile autoCPAP pressure of 11.8 cmH2O. We found no significant correlation between autoCPAP pressure and neck circumference, waist circumference or BMI. There was a moderate correlation between autoCPAP pressure and OSA severity (AHI r = 0.34, p = 0.02; oxygen desaturation index (ODI) r = 0.48, p < 0.001).
Conclusions
In this population, neither BMI nor neck circumference nor waist circumference is predictive of autoCPAP pressure. Therefore, the previously derived algorithm does not adequately predict the fixed CPAP pressure for subsequent clinical use in these obese individuals. In addition, some subjects without OSA generated high autoCPAP pressures, and thus, the correlation between OSA severity and autoCPAP pressure was only moderate.

Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 29:328(17):1230–1235
Davies CW, Crosby JH, Mullins RL, Barbour C, Davies RJ, Stradling JR (2000) Case-control study of 24 hour ambulatory blood pressure in patients with obstructive sleep apnoea and normal matched control subjects. Thorax 55(9):736–740
Marin JM, Carrizo SJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 19:365(9464):1046–1053
Barbé F, Pericás J, Muñoz A, Findley L, Antó JM, Agustí AG (1998) Automobile accidents in patients with sleep apnea syndrome. An epidemiological and mechanistic study. Am J Respir Crit Care Med 158(1):18–22
Miljeteig H, Hoffstein V (1993) Determinants of continuous positive airway pressure level for treatment of obstructive sleep apnea. Am Rev Respir Dis 147(6 Pt 1):1526–1530
Hoffstein V, Mateika S (1994) Predicting nasal continuous positive airway pressure. Am J Respir Crit Care Med 150(2):486–488
Stradling JR, Hardinge M, Paxton J, Smith DM (2004) Relative accuracy of algorithm-based prescription of nasal CPAP in OSA. Respir Med 98(2):152–154
Hailey D, Jacobs P, Mayers I, Mensinkai S (2005) The current status of autotitrating continuous positive airway pressure systems in the management of obstructive sleep apnea. Can Respir J 12(5):271–276
Cilli A, Uzun R, Bilge U (2013) The accuracy of autotitrating CPAP-determined residual apnea-hypopnea index. Sleep Breath Schlaf Atm 17(1):189–193
Farré R, Rotger M, Montserrat JM, Navajas D (1997) A system to generate simultaneous forced oscillation and continuous positive airway pressure. Eur Respir J 10(6):1349–1353
Teschler H, Berthon-Jones M, Thompson AB, Henkel A, Henry J, Konietzko N (1996) Automated continuous positive airway pressure titration for obstructive sleep apnea syndrome. Am J Respir Crit Care Med 154(3 Pt 1):734–740
Jenkinson C, Davies RJ, Mullins R, Stradling JR (1999) Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised prospective parallel trial. Lancet 19:353(9170):2100–2105
Katz I, Stradling J, Slutsky AS, Zamel N, Hoffstein V (1990) Do patients with obstructive sleep apnea have thick necks? Am Rev Respir Dis 141(5 Pt 1):1228–1231
Mortimore IL, Marshall I, Wraith PK, Sellar RJ, Douglas NJ (1998) Neck and total body fat deposition in nonobese and obese patients with sleep apnea compared with that in control subjects. Am J Respir Crit Care Med 157(1):280–283
Kim AM, Keenan BT, Jackson N, Chan EL, Staley B, Poptani H et al (2014) Tongue fat and its relationship to obstructive sleep apnea. Sleep 37(10):1639–1648
Owens RL, Malhotra A, Eckert DJ, White DP, Jordan AS (2010) The influence of end-expiratory lung volume on measurements of pharyngeal collapsibility. J Appl Physiol 108(2):445–451
Manuel AR, Hart N, Stradling JR (2015) Is a raised bicarbonate, without hypercapnia, part of the physiological spectrum of obesity-related hypoventilation? Chest 147(2):362–368
Gold AR, Marcus CL, Dipalo F, Gold MS (2002) Upper airway collapsibility during sleep in upper airway resistance syndrome. Chest 121(5):1531–1540
Sands SA, Eckert DJ, Jordan AS, Edwards BA, Owens RL, Butler JP et al (2014) Enhanced upper-airway muscle responsiveness is a distinct feature of overweight/obese individuals without sleep apnea. Am J Respir Crit Care Med 15:190(8):930–937
Deegan PC, Nolan P, Carey M, McNicholas WT (1996) Effects of positive airway pressure on upper airway dilator muscle activity and ventilatory timing. J Appl Physiol 81(1):470–479
Jordan AS, Wellman A, Heinzer RC, Lo Y-L, Schory K, Dover L et al (2007) Mechanisms used to restore ventilation after partial upper airway collapse during sleep in humans. Thorax 62(10):861–867
Rees K, Kingshott RN, Wraith PK, Douglas NJ (2000) Frequency and significance of increased upper airway resistance during sleep. Am J Respir Crit Care Med 162(4 Pt 1):1210–1214
Acknowledgments
This work was supported by the Oxford Health Services Research Committee, the National Institute of Health Research Oxford Biomedical Research Centre and the Oxford Radcliffe Hospital Charitable Funds. We would like to thank the trial nurses Debby Nicoll, Tara Harris and Barbara Winter.
Authors’ contributions
All authors agree to be accountable for all aspects of the work. They have approved this final version. They have been involved in drafting the work and revising it for important intellectual content. AM and JS made substantial contributions to the conception and design of the study. AM was responsible for data acquisition; AM, CT and JS are responsible for the analysis and interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the intuitional and national research committee and with the 1964 Helsinki declaration and its later amendments. The article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
JS has done consulting work for ResMed UK. AM and CT declare that they have no conflicts of interest.
Additional information
ClinicalTrials.gov, NCT01380418
Rights and permissions
About this article
Cite this article
Turnbull, C.D., Manuel, A.R. & Stradling, J.R. Does either obesity or OSA severity influence the response of autotitrating CPAP machines in very obese subjects?. Sleep Breath 20, 647–652 (2016). https://doi.org/10.1007/s11325-015-1267-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1267-y