Abstract
Purpose
In obstructive sleep apnea (OSA), severity of individual obstruction events is connected to increased mortality rate and it can be significantly different in patients with similar apnea-hypopnea index (AHI). However, possible gender-dependent variation in severity of obstruction events in different OSA categories is unknown. We investigated whether the severity of obstruction events differs between genders with similar AHI and if this difference varies between OSA categories.
Methods
Polygraphic recordings of 2057 consecutive patients with suspected OSA were reanalyzed and those with AHI ≥5/h were included for further analysis (n male = 893 and n female = 197). Statistical significance of differences in AHI, apnea index, hypopnea index, oxygen desaturation index, obstruction severity parameter, and severity of individual obstruction events between genders were evaluated using the Mann-Whitney U (MWU) test as well as the general linear model (GLM) univariate analysis adjusted for age, BMI, smoking, daytime sleepiness, snoring, and heart failure.
Results
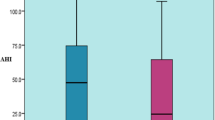
Apneas were 16.9 and 19.6% longer (MWU p ≤ 0.015, GLM p ≤ 0.036) and desaturation areas were 15.4 and 23.7% larger (MWU p ≤ 0.024, GLM p ≤ 0.053) in males compared to females with moderate and severe OSA, respectively. In contrast, hypopneas were 9.1% shorter (MWU p = 0.001, GLM p ≤ 0.001) and desaturation areas were 6.0% smaller (MWU p = 0.114, GLM p = 0.025) in men with mild OSA. The apnea index was 433.3 and 313.1% higher (MWU p ≤ 0.001, GLM p ≤ 0.043) and the hypopnea index was 12.2 and 17.8% lower (MWU p ≤ 0.001, GLM p = 0.002, p = 0.083) in males with mild and moderate OSA, respectively.
Conclusion
As severity of individual obstruction events was significantly different in males and females, the overall severity of OSA may not be similar despite the similarity in AHI.


Similar content being viewed by others
References
AASM (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22(5):667–689
Muraja-Murro A, Kulkas A, Hiltunen M, Kupari S, Hukkanen T, Tiihonen P, Mervaala E, Töyräs J (2013a) The severity of individual obstruction events is related to increased mortality rate in severe obstructive sleep apnea. J Sleep Res 22(6):663–669
Muraja-Murro A, Nurkkala J, Tiihonen P, Hukkanen T, Tuomilehto H, Kokkarinen J, Mervaala E, Töyräs J (2012) Total duration of apnea and hypopnea events and average desaturation show significant variation in patients with a similar apnea-hypopnea index. J Med Eng Technol 36(8):393–398
Mohsenin V (2001) Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest Journal 120(5):1442–1447
Leech JA, Onal E, Dulberg C, Lopata M (1988) A comparison of men and women with occlusive sleep apnea syndrome. CHEST Journal 94(5):983–988
Vagiakis E, Kapsimalis F, Lagogianni I, Perraki H, Minaritzoglou A, Alexandropoulou K, Roussos C, Kryger M (2006) Gender differences on polysomnographic findings in Greek subjects with obstructive sleep apnea syndrome. Sleep Med 7(5):424–430
Ware JC, McBrayer RH, Scott JA (2000) Influence of sex and age on duration and frequency of sleep apnea events. Sleep 23(2):165–170
Santos-Silva R, Sartori D, Truksinas V, Truksinas E, Alonso F, Tufik S, Bittencourt LRA (2009) Validation of a portable monitoring system for the diagnosis of obstructive sleep apnea syndrome. Sleep 32(5):629–636
Kulkas A, Tiihonen P, Eskola K, Julkunen P, Mervaala E, Töyräs J (2013a) Novel parameters for evaluating severity of sleep disordered breathing and for supporting diagnosis of sleep apnea-hypopnea syndrome. J Med Eng Technol 37(2):135–143
Leppänen T, Särkkä M, Kulkas A, Muraja-Murro A, Kupari S, Anttonen M, Tiihonen P, Mervaala E, Töyräs J (2016a) RemLogic plug-in enables clinical application of apnea-hypopnea index adjusted for severity of individual obstruction events. J Med Eng Technol 40(3):119–126
Muraja-Murro A, Eskola K, Kolari T, Tiihonen P, Hukkanen T, Tuomilehto H, Peltonen M, Mervaala E, Töyräs J (2013b) Mortality in middle-aged men with obstructive sleep apnea in Finland. Sleep and Breathing 17(3):1047–1053
Iber C, Ancoli-Israel S, Chesson A, Quan S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. American Academy of Sleep Medicine, Westchester Il, pp. 17–59
Kulkas A, Tiihonen P, Julkunen P, Mervaala E, Töyräs J (2013b) Novel parameters indicate significant differences in severity of obstructive sleep apnea with patients having similar apnea–hypopnea index. Med Biol Eng Comput 51(6):697–708
Leppänen T, Töyräs J, Muraja-Murro A, Kupari S, Tiihonen P, Mervaala E, Kulkas A (2016b) Length of individual apnea events is increased by supine position and modulated by severity of obstructive sleep apnea. Sleep Disorders 2016:9645347
Quintana-Gallego E, Carmona-Bernal C, Capote F, Sánchez-Armengol Á, Botebol-Benhamou G, Polo-Padillo J, Castillo-Gómez J (2004) Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med 98(10):984–989
Pickett CK, Regensteiner JG, Woodard WD, Hagerman DD, Weil JV, Moore LG (1989) Progestin and estrogen reduce sleep-disordered breathing in postmenopausal women. J Appl Physiol 66(4):1656–1661
Kimura H, Tatsumi K, Kunitomo F, Okita S, Tojima H, Kouchiyama S, Masuyama S, Shinozaki T, Honda Y, Kuriyama T (1989) Progesterone therapy for sleep apnea syndrome evaluated by occlusion pressure responses to exogenous loading. Am Rev Respir Dis 139(5):1198–1206
McArdle N, King S, Shepherd K, Baker V, Ramanan D, Ketheeswaran S, Bateman P, Wimms A, Armitstead J, Richards G, Hillman D, Eastwood P (2015) Study of a novel APAP algorithm for the treatment of obstructive sleep apnea in women. Sleep 38(11):1775–1781
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, Kales A (2001) Prevalence of sleep-disordered breathing in women: effects of gender. An J Respir Crit Care Med 163(3):608–613
Tiitinen A (2008) Vaihdevuosioireet. Duodecim 124(21):2479–2480
Farre R, Montserrat JM, Navajas D (2004) Noninvasive monitoring of respiratory mechanics during sleep. Eur Respir J 24(6):1052–1060
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Financial support for this study was provided by the Kuopio University Hospital, the Committee State Research Financing of the Research Committee of the Kuopio University Hospital Catchment Area (projects 5041754 and 5041755), by the Tampere Tuberculosis Foundation, by the Seinäjoki Central Hospital, the Competitive State Research Financing of Expert Responsibility Area of Tampere University Hospital (Grant VTR3114), and by the Emil Aaltonen Foundation.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Research Ethics Committee of the Hospital District of Northern Savo, Kuopio, Finland, has reviewed and given a favorable statement on the study protocol (decision numbers 127/2004 and 24/2013). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent by the patients was not required.
Rights and permissions
About this article
Cite this article
Leppänen, T., Kulkas, A., Duce, B. et al. Severity of individual obstruction events is gender dependent in sleep apnea. Sleep Breath 21, 397–404 (2017). https://doi.org/10.1007/s11325-016-1430-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1430-0