Summary
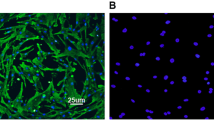
The main pathogenesis of saphenous vein graft neointimal hyperplasia after coronary artery bypass grafting (CABG) is inflammation-caused migration and proliferation of vascular smooth muscle cells (VSMCs). Janus kinase 2/signal transducer and activators of transcription 3 (JAK2/STAT3) pathway is an important signaling pathway through which VSMCs phenotype conversion occurs. Suppressor of cytokine signaling 3 (SOCS3) is the classic negative feedback inhibitor of JAK2/STAT3 pathway. Growing studies show that SOCS3 plays an important anti-inflammatory role in numerous autoimmune diseases, inflammatory diseases and inflammation-related tumors. However, the effect and mechanism of SOCS3 on vein graft disease is unclear. The purpose of this study was to investigate the effects of SOCS3 on the inflammation, migration and proliferation of VSMCs in vitro and the mechanism. The small interference RNA plasmid targeting rat SOCS3 (SiRNA-rSOCS3) and the recombinant adenovirus vector carrying rat SOCS3 gene (pYrAd-rSOCS3) were constructed, and the empty plamid (SiRNA-control) and vector (pYrAd-GFP) only carrying GFP reported gene were constructed as control. The rat VSMCs were cultured. There were two large groups of A (SOCS3 up-regulated): control group, IL-6/IFN-γ group, IL-6/IFN-γ+pYrAd-rSOCS3 group, IL-6/IFN-γ+pYrAd-GFP group; and B (SOCS3 down-regulated): control group, IL-6/IFN-γ group, IL-6/IFN-γ+SiRNA-rSOCS3 group and IL-6/ IFN -γ+SiRNA-control group. The pYrAd-rSOCS3 and SiRNA-rSOCS3 were transfected into VSMCs induced by IL-6/IFN-γ. After 24 h, real-time reverse transcription polymerase chain reaction (RT-PCR) and Western blotting were used to detect the mRNA and protein expression of SOCS3, STAT3 (only by Western blotting), P-STAT3 (only by Western blotting), IL-1β, IL-6, TNF-α, MCP-1 and ICAM-1. The MTT, Transwell assay and flow cytometry were used to examine VSMCs proliferation, migration and cell cycle progression, respectively. As compared with control group, the mRNA and protein expression of SOCS3, STAT3, P-STAT3, IL-1β, IL-6, TNF-α, MCP-1 and ICAM-1 was significantly up-regulated in VSMCs stimulated by IL-6/IFN-γ. However, in VSMCs transfected with pYrAd-rSOCS3 before stimulation with IL-6/IFN-γ, the expression of SOCS3 mRNA and protein was further up-regulated, and that of STAT3, P-STAT3, IL-1β, IL-6, TNF-α, MCP-1 and ICAM-1 was significantly down-regulated as compared with IL-6/IFN-γ group and IL-6/IFN-γ+pYrAd-GFP group. The expression of those related-cytokines in IL-6/IFN-γ+SiRNA-rSOCS3 group was markedly increased as compared with IL-6/IFN-γ group and IL-6/IFN-γ+SiRNA-control group. The absorbance (A) values, the number of cells migrating to the lower chamber, and percentage of cells in the G2/M+S phase were increased in VSMCs stimulated by IL-6/IFN-γ. In VSMCs incubated with pYrAd-rSOCS3 or SiRNA-rSOCS3 before IL-6/IFN-γ stimulation, the A values, the number of cells migrating to the lower chamber, and the percentage of cells in the G2/M+S phase were significantly decreased, and increased respectively. These results imply that IL-6/IFN-γ, strong inflammatory stimulators, can promote transformation of VSMCs phenotype form a quiescent contractile state to a synthetic state by activating JAK2/STAT3 pathway. Over-expresssed SOCS3 might inhibit pro-inflammatory effect, migration and growth of VSMCs by blocking STAT3 activation and phosphorylation. These data in vitro confirm that SOCS3 may play a negatively regulatory role in development and progression of vein graft failure. These conclusions can provide a novel strategy for clinical treatment of vein graft diseases and a new theoretic clue for related drug development.
Similar content being viewed by others
References
Kim FY, Marhefka G, Ruggiero NJ, et al. Saphenous vein graft disease: review of pathophysiology, prevention, and treatment. Cardiol Rev, 2013,21(2):101–109
O’Sullivan LA, Liongue C, Lewis RS, et al. Cytokine receptor signaling through the Jak-Stat-Socs pathway in disease. Mol Immunol, 2007,44(10):2497–2506
Kile BT, Nicola NA, Alexander WS. Negative regulators of cytokine signaling. Int J Hematol, 2001,73(3):292–298
Babon JJ, McManus EJ, Yao S, et al. The structure of SOCS3 reveals the basis of the extended SH2 domain function and identifies an unstructured insertion that regulates stability. Mol Cell, 2006,22(2):205–216
Zhao J, Zhang M, Li W, et al. Suppression of JAK2/STAT3 signaling reduces end-to-end arterial anastomosis induced cell proliferation in common carotid arteries of rats. PLoS ONE, 2013,8(3):e58730
Yoshimura A, Suzuki M, Sakaguchi R, et al. SOCS, inflammation, and autoimmunity. Front Immunol, 2012, 3:20
Yoshimura A, Naka T, Kubo M. SOCS proteins, cytokine signalling and immune regulation. Nat Rev Immunol, 2007,7(6):454–465
Hiwatashi K, Tamiya T, Hasegawa E, et al. Suppression of SOCS3 in macrophages prevents cancer metastasis by modifying macrophage phase and MCP2/CCL8 induction. Cancer Lett, 2011,308(2):172–180
Liu X, Qu X, Chen Y, et al. Mesenchymal stem/stromal cells induce the generation of novel IL-10-dependent regulatory dendritic cells by SOCS3 activation. J Immunol, 2012,189(3):1182–1192
Ortiz-Munoz G, Martin-Ventura JL, Hernandez-Vargas P, et al. Suppressors of cytokine signaling modulate JAK/STAT-mediated cell responses during atherosclerosis. Arterioscler Thromb Vasc Biol, 2009,29(4):525–531
Xiang S, Dong NG, Liu JP, et al. Construction of rat SOCS3 recombinant adenovirus vector and its expression in rat primary vascular smooth muscle cells. Acta Med Univ Sci Technol Huazhong (Chinese), 2012,41(5):161–166
Xiang S, Dong NG, Liu JP, et al. Expression of suppressor of cytokine signaling 1/3 in peripheral blood mononuclear cells of patients with coronary artery disease. Acta Med Unvi Sci Technol Huazhong (Chinese), 2012,41(2):152–155
Muto A, Model L, Ziegler K, et al. Mechanisms of vein graft adaptation to the arterial circulation: insights into the neointimal algorithm and management strategies. Circ J, 2010,74(8):1501–1512
Wainwright CL, Miller AM, Wadsworth RM. Inflammation as a key event in the development of neointima following vascular balloon injury. Clin Exp Pharmacol Physiol, 2001,28(11):891–895
Neeli I. An essential role of the Jak-2/STAT-3/cytosolic phospholipase A2 axis in platelet-derived growth factor BB-induced vascular smooth muscle cell motility. J Biol Chem, 2004,279(44):46 122–46 128
White GE, Cotterill A, Addley MR, et al. Suppressor of cytokine signalling protein SOCS3 expression is increased at sites of acute and chronic inflammation. J Mol Histol, 2011,42(2):137–151
Tischoff I, Hengge UR, Vieth M, et al. Methylation of SOCS-3 and SOCS-1 in the carcinogenesis of Barrett’s adenocarcinoma. Gut, 2007,56(8):1047–1053
Niwa Y, Kanda H, Shikauchi Y, et al. Methylation silencing of SOCS-3 promotes cell growth and migration by enhancing JAK/STAT and FAK signalings in human hepatocellular carcinoma. Oncogene, 2005,24(42):6406–6417
Wei RC, Cao X, Gui JH, et al. Augmenting the antitumor effect of TRAIL by SOCS3 with double-regulated replicating oncolytic adenovirus in hepatocellular carcinoma. Hum Gene Ther, 2011,22(9):1109–1119
Liang X, He M, Chen T, et al. 17beta-estradiol suppresses the macrophage foam cell formation associated with SOCS3. Horm Metab Res, 2013,45(6):423–429
Yajima T, Murofushi Y, Zhou H, et al. Absence of SOCS3 in the cardiomyocyte increases mortality in a gp130-dependent manner accompanied by contractile dysfunction and ventricular arrhythmias. Circulation, 2011,124(24):2690–2701
Croker BA, Kiu H, Pellegrini M, et al. IL-6 promotes acute and chronic inflammatory disease in the absence of SOCS3. Immunol Cell Biol, 2012,90(1):124–129
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xiang, S., Dong, Ng., Liu, Jp. et al. Inhibitory effects of suppressor of cytokine signaling 3 on inflammatory cytokine expression and migration and proliferation of IL-6/IFN-γ-induced vascular smooth muscle cells. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 33, 615–622 (2013). https://doi.org/10.1007/s11596-013-1168-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-013-1168-x