ABSTRACT
BACKGROUND
Not all primary care clinics are prepared to implement care coordination services for chronic conditions, such as diabetes. Understanding true capacity to coordinate care is an important first-step toward establishing effective and efficient care coordination. Yet, we could identify no diabetes-specific instruments to systematically assess readiness and/or status of primary care clinics to engage in diabetes care coordination.
OBJECTIVE
This report describes the development and initial validation of the Diabetes Care Coordination Readiness Assessment (DCCRA), which is intended to measure primary care clinic readiness to coordinate care for adult patients with diabetes.
DESIGN
The instrument was developed through iterative item generation within a framework of five domains of care coordination: Organizational Capacity, Care Coordination, Clinical Management, Quality Improvement, and Technical Infrastructure.
PARTICIPANTS
Validation data was collected on 39 primary care clinics.
MAIN MEASURES
Content validity, inter-rater reliability, internal consistency, and construct validity of the 49-item instrument were assessed.
KEY RESULTS
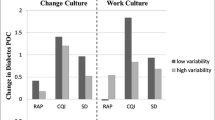
Inter-rater agreement indices per item ranged from 0.50 to 1.0. Cronbach’s alpha of the entire instrument was 0.964, and for the five domain scales ranged from 0.688 to 0.961. Clinics with existing care coordinators were rated as more ready to support care coordination than clinics without care coordinators for the entire DCCRA and for each domain, supporting construct validity.
CONCLUSIONS
As providers increasingly attempt to adopt patient-centered approaches, introduction of the DCCRA is timely and appropriate for assisting clinics with identifying gaps in provision of care coordination services. The DCCRA’s strengths include promising psychometric properties. A valid measure of diabetes care coordination readiness should be useful in diabetes program evaluation, assistance with quality improvement initiatives, and measurement of patient-centered care in research.
Similar content being viewed by others
REFERENCES
National Priorities Partnership. National Priorities and Goals: aligning our Efforts to Transform America’s Healthcare. Washington, DC: National Quality Forum; 2008
McDonald KM, Sundaram V, Bravata DM, et al. Care coordination. In: Shojania KG, McDonald KM, Wachter RM, Owens DK, eds. Closing the Quality Gap: a Critical Analysis of Quality Improvement Strategies. Technical Review 9 (Prepared by Stanford-UCSF Evidence-Based Practice Center under contract No. 290020017). Vol. 7. Rockville, MD: Agency for Healthcare Research and Quality, June 2007. AHRQ Publication No. 04(07)00517
Cornu P, Steurbaut S, Leysen T, et al. Discrepancies in medication information for the primary care physician and the geriatric patient at discharge. Ann Pharmacother. 2012;46:983–90.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28.
Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–70.
Stewart BA, Fernandes S, Rodriguez-Huertas E, Landzberg M. A preliminary look at duplicate testing associated with lack of electronic health record interoperability for transferred patients. J Am Med Inform Assoc. 2010;17:341–4.
Antonelli RC, McAllister JW, Popp J. Making Care Coordination a Critical Component of the Pediatric Healthcare System: a Multidisciplinary Framework. New York: The Commonwealth Fund; 2009.
Hess BJ, Lynn LA, Holmboe ES, Lipner RS. Toward better care coordination through improved communication with referring physicians. Acad Med. 2009;84:S109–12.
O’Malley AS, Tynan A, Cohen GR, Kemper N, Davis MM. Coordination of care by primary care practices: strategies, lessons and implications. Res Briefs. 2009;12:1–16.
Shetty G, Brownson CA. Characteristics of organizational resources and supports for self management in primary care. Diabetes Educ. 2007;33:185S–92S.
Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary care physicians’ links to other physicians through Medicare patients: the scope of care coordination. Ann Intern Med. 2009;150:236–42.
MacPhail LH, Neuwirth EB, Bellows J. Coordination of diabetes care in four delivery models using an electronic health record. Med Care. 2009;47:993–9.
Stellefson M, Dipnarine K, Stopka C. The Chronic Care Model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:120180.
McDonald KM, Schultz E, Albin L, et al. Care Coordination Atlas Version 3 (Prepared by Stanford University under subcontract to Battelle on Contract No. 290040020). AHRQ Publication No. 110023EF. Rockville, MD: Agency for Healthcare Research and Quality; 2010
National Quality Forum (NQF). Preferred Practices and Performance Measures for Measuring and Reporting Care Coordination: a Consensus Report. Washington: NQF; 2010.
Cooley WC, McAllister JW, Sherrieb K, Clark RE. The Medical Home Index: development and validation of a new practice-level measure of implementation of the Medical Home model. Ambul Pediatr. 2003;3:173–80.
Bonomi AE, Wagner EH, Glasgow RE, VonKorff M. Assessment of chronic illness care (ACIC): a practical tool to measure quality improvement. Health Serv Res. 2002;37:791–820.
Weiner BJ, Amick H, Lee SY. Conceptualization and measurement of organizational readiness for change: a review of the literature in health services research and other fields. Med Care Res Rev. 2008;65:379–436.
California Healthcare Foundation and Community Clinics Initiative of Tides. Community Clinic EHR Readiness Assessment. http://www.careinnovations.org/knowledge-center/ehr-readiness-assessment/ (accessed July 12, 2013)
Safety Net Medical Home Initiative, Horner K, Schaefer S, Wagner E. Care Coordination: reducing Care Fragmentation in Primary Care. 1st ed. Phillips KE, ed. Seattle, WA: The MacColl Institute for Healthcare Innovation at the Group Health Research Institute and Qualis Health; 2011
Birnberg JM, Drum ML, Huang ES, et al. Development of a safety net medical home scale for clinics. J Gen Intern Med. 2011;26:1418–25.
Brownson CA, Miller D, Crespo R, et al. Development and use of a quality improvement tool to assess self-management support in primary care. Jt Comm J Qual Saf. 2007;33:408–16.
Gwet K. Handbook of Inter-Rater Reliability: how to Measure the Level of Agreement Between Two or Multiple Raters. Gaithersburg: Stataxis Publishing Company; 2001.
Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61:29–48.
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46.
Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43:543–9.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314:572.
Kline P. The Handbook of Psychological Testing. 2nd ed. London: Routledge; 1999.
Hattie J, Cooksey RW. Procedures for assessing the validities of tests using the “known-groups” method. Appl Psychol Meas. 1984;8:295–305.
Acknowledgements
This work was supported by Grant Number 90BC001101 from the Office of the National Coordinator for Health Information Technology (ONC), Department of Health and Human Services (DHHS), awarded to Inland Northwest Health Services. Article contents are solely the responsibility of the authors and do not necessarily represent the official views of ONC or DHHS.
Portions of the data in this manuscript were presented at American Public Health Association 139th Annual Meeting and Exposition, October 31 to November 2, 2011, Washington, DC, and the AcademyHealth Annual Research Meeting, June 12–14, 2011, Seattle, WA.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 104 kb)
Rights and permissions
About this article
Cite this article
Weeks, D.L., Polello, J.M., Hansen, D.T. et al. Measuring Primary Care Organizational Capacity for Diabetes Care Coordination: The Diabetes Care Coordination Readiness Assessment. J GEN INTERN MED 29, 98–103 (2014). https://doi.org/10.1007/s11606-013-2566-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2566-2