Abstract
Background
Several endocrine abnormalities, including hypothyroidism and Cushing’s syndrome (CS), are considered as causative factors of obesity. The aim of this study was to evaluate the prevalence of endocrine disorders and obesity-associated co-morbidities, as well as the impact of substantial weight loss.
Methods
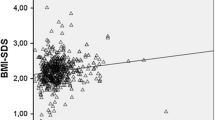
Screening was performed in 433 consecutive morbidly obese patients (age 41 ± 12 years; BMI 47 ± 6.9 kg/m2; women 76%). A 1-mg dexamethasone suppression test (1-mg DST) was conducted to exclude CS, and thyrotropin (TSH) was measured to exclude hypothyroidism. Insulin sensitivity was estimated from oral glucose tolerance tests employing the Clamp-like index. Examinations were carried out at baseline, as well as at 6 and 12 months postoperatively.
Results
The prevalence of CS was below 0.6%. Before surgery, TSH was elevated compared to an age- and sex-matched normal weight control group (2.4 ± 1.2 vs. 1.5 ± 0.7 μU/ml; p < 0.001). The NCEP criteria of metabolic syndrome (MetS) were fulfilled by 39.5% of the patients. Impaired glucose tolerance and diabetes mellitus were observed in 23.5% and 22.6%, respectively. Seventy-two percent were insulin resistant. During follow-up, weight (BMI 47 ± 6.9 vs. 36 ± 6.4 vs. 32 ± 6.6 kg/m2; p < 0.001) and TSH decreased significantly (2.4 ± 1.2 vs. 1.8 ± 1.0 vs. 1.8 ± 1.0 μU/ml; p < 0.001). Serum cortisol was higher in the MetS+-group compared to the MetS--group (15.0 ± 6.3 vs. 13.5 ± 6.3 μg/dl; p = 0.003).
Conclusions
CS appears to be a rare cause of morbid obesity. Normalization of slightly elevated thyrotropin after weight loss suggests that obesity causes TSH elevation rather than the reverse.



Similar content being viewed by others
References
Kokkoris P, Pi-Sunyer FX. Obesity and endocrine disease. Endocrinol Metab Clin North Am. 2003;32:895–914.
Maddox GL, Liederman V. Overweight as a social disability with medical implications. J Med Educ. 1969;44:214–20.
Price JH, Desmond SM, Krol RA, et al. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45.
Michalaki MA, Vagenakis AG, Leonardou AS, et al. Thyroid function in humans with morbid obesity. Thyroid. 2006;16:73–8.
Sari R, Balci MK, Altunbas H, et al. The effect of body weight and weight loss on thyroid volume and function in obese women. Clin Endocrinol (Oxf). 2003;59:258–62.
Raftopoulos Y, Gagne DJ, Papasavas P, et al. Improvement of hypothyroidism after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2004;14:509–13.
Fazylov R, Soto E, Cohen S, et al. Laparoscopic Roux-en-Y gastric bypass surgery on morbidly obese patients with hypothyroidism. Obes Surg. 2008;18:644–7.
Alagna S, Cossu ML, Masala A, et al. Evaluation of serum leptin levels and thyroid function in morbidly obese patients treated with bariatric surgery. Eat Weight Disord. 2003;8:95–9.
Buscemi S, Verga S, Maneri R, et al. Influences of obesity and weight loss on thyroid hormones. A 3–3.5-year follow-up study on obese subjects with surgical bilio-pancreatic by-pass. J Endocrinol Invest. 1997;20:276–81.
Catargi B, Rigalleau V, Poussin A, et al. Occult Cushing’s syndrome in type-2 diabetes. J Clin Endocrinol Metab. 2003;88:5808–13.
Omura M, Saito J, Yamaguchi K, et al. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res. 2004;27:193–202.
Anderson Jr GH, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens. 1994;12:609–15.
Tiryakioglu O, Ugurlu S, Yalin S, et al. Screening for Cushing’s syndrome in obese patients. Clinics (Sao Paulo). 2010;65:9–13.
Anderwald C, Anderwald-Stadler M, Promintzer M, et al. The Clamp-like index: a novel and highly sensitive insulin sensitivity index to calculate hyperinsulinemic clamp glucose infusion rates from oral glucose tolerance tests in nondiabetic subjects. Diabetes Care. 2007;30:2374–80.
Promintzer M, Krebs M, Todoric J, et al. Insulin resistance is unrelated to circulating retinol binding protein and protein C inhibitor. J Clin Endocrinol Metab. 2007;92:4306–12.
Chiodini I. Diagnosis and treatment of subclinical hypercortisolism. J Clin Endocrinol Metab. 2011.
Nickelsen T, Lissner W, Schoffling K. The dexamethasone suppression test and long-term contraceptive treatment: measurement of ACTH or salivary cortisol does not improve the reliability of the test. Exp Clin Endocrinol. 1989;94:275–80.
Qureshi AC, Bahri A, Breen LA, et al. The influence of the route of oestrogen administration on serum levels of cortisol-binding globulin and total cortisol. Clin Endocrinol (Oxf). 2007;66:632–5.
Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93:1526–40.
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421.
Baid SK, Rubino D, Sinaii N, et al. Specificity of screening tests for Cushing’s syndrome in an overweight and obese population. J Clin Endocrinol Metab. 2009;94:3857–64.
Cooper DS. Clinical practice. Subclinical hypothyroidism. N Engl J Med. 2001;345:260–5.
Douyon L, Schteingart DE. Effect of obesity and starvation on thyroid hormone, growth hormone, and cortisol secretion. Endocrinol Metab Clin North Am. 2002;31:173–89.
al-Adsani H, Hoffer LJ, Silva JE. Resting energy expenditure is sensitive to small dose changes in patients on chronic thyroid hormone replacement. J Clin Endocrinol Metab. 1997;82:1118–25.
Sorisky A, Bell A, Gagnon A. TSH receptor in adipose cells. Horm Metab Res. 2000;32:468–74.
Valyasevi RW, Harteneck DA, Dutton CM, et al. Stimulation of adipogenesis, peroxisome proliferator-activated receptor-gamma (PPARgamma), and thyrotropin receptor by PPARgamma agonist in human orbital preadipocyte fibroblasts. J Clin Endocrinol Metab. 2002;87:2352–8.
Guo F, Bakal K, Minokoshi Y, et al. Leptin signaling targets the thyrotropin-releasing hormone gene promoter in vivo. Endocrinology. 2004;145:2221–7.
Kok P, Roelfsema F, Langendonk JG, et al. High circulating thyrotropin levels in obese women are reduced after body weight loss induced by caloric restriction. J Clin Endocrinol Metab. 2005;90:4659–63.
de Moraes CM Moulin, Mancini MC, de Melo ME, et al. Prevalence of subclinical hypothyroidism in a morbidly obese population and improvement after weight loss induced by Roux-en-Y gastric bypass. Obes Surg. 2005;15:1287–91.
Reinehr T. Obesity and thyroid function. Mol Cell Endocrinol. 2010;316:165–71.
Stewart PM, Boulton A, Kumar S, et al. Cortisol metabolism in human obesity: impaired cortisone– > cortisol conversion in subjects with central adiposity. J Clin Endocrinol Metab. 1999;84:1022–7.
Hautanen A, Raikkonen K, Adlercreutz H. Associations between pituitary-adrenocortical function and abdominal obesity, hyperinsulinaemia and dyslipidaemia in normotensive males. J Intern Med. 1997;241:451–61.
Manco M, Fernandez-Real JM, Valera-Mora ME, et al. Massive weight loss decreases corticosteroid-binding globulin levels and increases free cortisol in healthy obese patients: an adaptive phenomenon? Diabetes Care. 2007;30:1494–500.
Lambillotte C, Gilon P, Henquin JC. Direct glucocorticoid inhibition of insulin secretion. An in vitro study of dexamethasone effects in mouse islets. J Clin Invest. 1997;99:414–23.
Mariniello B, Ronconi V, Rilli S, et al. Adipose tissue 11beta-hydroxysteroid dehydrogenase type 1 expression in obesity and Cushing’s syndrome. Eur J Endocrinol. 2006;155:435–41.
Desbriere R, Vuaroqueaux V, Achard V, et al. 11beta-hydroxysteroid dehydrogenase type 1 mRNA is increased in both visceral and subcutaneous adipose tissue of obese patients. Obesity (Silver Spring). 2006;14:794–8.
Ricketts ML, Verhaeg JM, Bujalska I, et al. Immunohistochemical localization of type 1 11beta-hydroxysteroid dehydrogenase in human tissues. J Clin Endocrinol Metab. 1998;83:1325–35.
Freeman L, Hewison M, Hughes SV, et al. Expression of 11beta-hydroxysteroid dehydrogenase type 1 permits regulation of glucocorticoid bioavailability by human dendritic cells. Blood. 2005;106:2042–9.
Munoz R, Carvajal C, Escalona A, et al. 11beta-hydroxysteroid dehydrogenase type 1 is overexpressed in subcutaneous adipose tissue of morbidly obese patients. Obes Surg. 2009;19:764–70.
Anagnostis P, Athyros VG, Tziomalos K, et al. Clinical review: the pathogenetic role of cortisol in the metabolic syndrome: a hypothesis. J Clin Endocrinol Metab. 2009;94:2692–701.
Ward AM, Fall CH, Stein CE, et al. Cortisol and the metabolic syndrome in South Asians. Clin Endocrinol (Oxf). 2003;58:500–5.
Ravaja N, Keltikangas-Jarvinen L, Viikari J. Life changes, locus of control and metabolic syndrome precursors in adolescents and young adults: a three-year follow-up. Soc Sci Med. 1996;43:51–61.
Karelis AD, Brochu M, Rabasa-Lhoret R. Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab. 2004;30:569–72.
Karelis AD, Faraj M, Bastard JP, et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J Clin Endocrinol Metab. 2005;90:4145–50.
Primeau V, Coderre L, Karelis AD, et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes (Lond). 2010.
Bonora E, Kiechl S, Willeit J, et al. Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Diabetes. 1998;47:1643–9.
Ferrannini E, Natali A, Bell P, et al. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J Clin Invest. 1997;100:1166–73.
Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008;168:1617–24.
Conflict of interest disclosure
DJ, PW, CHA, YW, MPS, AH, FL, GP, BL, AG, AL and MK declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Janković, D., Wolf, P., Anderwald, CH. et al. Prevalence of Endocrine Disorders in Morbidly Obese Patients and the Effects of Bariatric Surgery on Endocrine and Metabolic Parameters. OBES SURG 22, 62–69 (2012). https://doi.org/10.1007/s11695-011-0545-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0545-4