Abstract
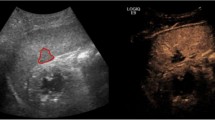
The double-line sign (DLS) is a wedge-shaped hypoechoic area in Morison’s pouch bounded on both sides by echogenic lines. It represents a false-positive finding for free intraperitoneal fluid when performing focused assessment with sonography in trauma examinations. The purpose of this study was to determine the prevalence of DLS. Secondarily, the study will further investigate the relationship between the presence of a DLS and body mass index (BMI). This was a prospective study that enrolled patients over a 7-month period. Inclusion criteria were patients ≥18 years of age presenting to the Emergency Department (ED) requiring a FAST examination as part of the patient’s standard medical care. Each examination was performed by one of six experienced ultrasonographers. Presence or absence of the DLS was established in real time and gender, height, weight, and BMI were recorded for each patient. The overall prevalence rate of DLS and the corresponding 95 % confidence interval were calculated, as well as the prevalence rates broken down by BMI characterized as underweight, normal weight, overweight, and obese; and age category (18–29, 30–64, and 65+). The Chi-square test and a Fisher’s exact test for BMI category were used to compare the prevalence rates of positive DLS among the different demographic groups. 100 patients were enrolled in the study; the overall prevalence was 27 %. There was no statistical significance among the different demographic groups or BMI. The DLS is a prevalent finding. We believe this sign has become more apparent due to improved imaging technology and resolution.


Similar content being viewed by others
References
Becker Alexander (2010) Is the FAST exam reliable in severely injured patients? Injury. Int J Care Inj 41:479–483
Jang Timothy (2004) Residents should not independently perform focused abdominal sonography for trauma after 10 training examinations. J Ultrasound Med 23:793–797
Kendall JL, Ramos JP (2003) Fluid-filled bowel mimicking hemoperitoneum a false-positive finding during sonographic evaluation for trauma. J Emerg Med 25:79–82
Nagdev A, Racht J (2008) The “gastric fluid” sign: an unrecognized false-positive finding during focused assessment for trauma examinations. Am J Emerg Med 26:630.e5–630.e7
Sierzenski Paul R, Sign The Double-Line (2011) A false positive finding on the focused assessment with sonography for trauma (FAST) examination. J Emerg Med 40(2):188–189
Conflict of interest
The Authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human and animals performed by any of the authors.
Informed consent
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patwa, A.S., Cipot, S., Lomibao, A. et al. Prevalence of the “double-line” sign when performing focused assessment with sonography in trauma (FAST) examinations. Intern Emerg Med 10, 721–724 (2015). https://doi.org/10.1007/s11739-015-1264-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-015-1264-y