Abstract
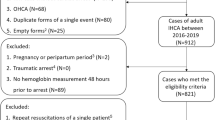
In addition to cardiac output, oxygen delivery is determined by the amount of oxygen carried by hemoglobin, which is estimated by the product of hemoglobin level and peripheral hemoglobin oxygen saturation (SpO2). Optimal hemoglobin concentration for post-cardiac arrest syndrome (PCAS) has not yet been investigated thoroughly. We conducted a retrospective observational study in a single medical center. We included adult patients between 2006 and 2012 who experienced in-hospital cardiac arrest, and achieved sustained return of spontaneous circulation (ROSC). We used multivariable logistic regression analysis to identify factors associated with favorable neurological status at hospital discharge, defined as a score of 1 or 2 on the Cerebral Performance Category scale. Minimum hemoglobin concentration and SpO2 during the initial 24 h after ROSC were used for analysis. Anemia was defined by the World Health Organization criteria as a hemoglobin concentration <12 g/dL in women and <13 g/dL in men. Of the 426 patients included in our analysis, 387 patients (90.8 %) met the criteria for anemia. The mean minimum hemoglobin concentration among all the patients was 9.2 g/dL. The product of hemoglobin × SpO2 was correlated with a favorable neurological outcome (odds ratio 1.003, 95 % confidence interval 1.002–1.004). According to recommended SpO2 by resuscitation guidelines (94–98 %), we calculated the corresponding range of minimum required hemoglobin concentration to be 8.6–9.0 g/dL for a favorable neurological outcome. Anemia common among PCAS patients. Neurological outcome in PCAS might be correlated with hemoglobin concentration following resuscitation.





Similar content being viewed by others
References
Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, American Heart Association Get with the Guidelines–Resuscitation Investigators (2012) Trends in survival after in-hospital cardiac arrest. N Engl J Med 367:1912–1920. doi:10.1056/NEJMoa1109148
Sasson C, Rogers MA, Dahl J, Kellermann AL (2010) Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 3:63–81. doi:10.1161/CIRCOUTCOMES.109.889576
Nolan JP, Neumar RW, Adrie C et al (2008) Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation 79:350–379. doi:10.1016/j.resuscitation.2008.09.017
Vallet B, Robin E, Lebuffe G (2010) Venous oxygen saturation as a physiologic transfusion trigger. Crit Care 14:213. doi:10.1186/cc8854
Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL, Association AmericanHeart (2010) Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122:S768–S786. doi:10.1161/CIRCULATIONAHA.110.971002
Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, Perkins GD (2010) European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation 81:1305–1352. doi:10.1016/j.resuscitation.2010.08.017
Hao Z, Wu B, Wang D, Lin S, Tao W, Liu M (2013) A cohort study of patients with anemia on admission and fatality after acute ischemic stroke. J Clin Neurosci 20:37–42. doi:10.1016/j.jocn.2012.05.020
Kellert L, Martin E, Sykora M, Bauer H, Gussmann P, Diedler J, Herweh C, Ringleb PA, Hacke W, Steiner T, Bösel J (2011) Cerebral oxygen transport failure?: decreasing hemoglobin and hematocrit levels after ischemic stroke predict poor outcome and mortality: STroke: RelevAnt Impact of hemoGlobin, Hematocrit and Transfusion (STRAIGHT)—an observational study. Stroke 42:2832–2837. doi:10.1161/STROKEAHA.110.606665
Tanne D, Molshatzki N, Merzeliak O, Tsabari R, Toashi M, Schwammenthal Y (2010) Anemia status, hemoglobin concentration and outcome after acute stroke: a cohort study. BMC Neurol 10:22. doi:10.1186/1471-2377-10-22
Diamond PT, Gale SD, Evans BA (2003) Relationship of initial hematocrit level to discharge destination and resource utilization after ischemic stroke: a pilot study. Arch Phys Med Rehabil 84:964–967. doi:10.1016/S0003-9993(03)00009-1
Lee PC, Kini AS, Ahsan C, Fisher E, Sharma SK (2004) Anemia is an independent predictor of mortality after percutaneous coronary intervention. J Am Coll Cardiol 44:541–546. doi:10.1016/j.jacc.2004.04.047
Nikolsky E, Aymong ED, Halkin A, Grines CL, Cox DA, Garcia E, Mehran R, Tcheng JE, Griffin JJ, Guagliumi G, Stuckey T, Turco M, Cohen DA, Negoita M, Lansky AJ, Stone GW (2004) Impact of anemia in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention: analysis from the controlled abciximab and device investigation to lower late angioplasty complications (CADILLAC) trial. J Am Coll Cardiol 44:547–553. doi:10.1016/j.jacc.2004.03.080
Sabatine MS, Morrow DA, Giugliano RP, Burton PB, Murphy SA, McCabe CH, Gibson CM, Braunwald E (2005) Association of hemoglobin levels with clinical outcomes in acute coronary syndromes. Circulation 111:2042–2049. doi:10.1161/01.CIR.0000162477.70955.5F
Go AS, Yang J, Ackerson LM, Lepper K, Robbins S, Massie BM, Shlipak MG (2006) Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: the anemia in chronic heart failure: outcomes and resource utilization (ANCHOR) study. Circulation 113:2713–2723. doi:10.1161/CIRCULATIONAHA.105.577577
Anand I, McMurray JJ, Whitmore J, Warren M, Pham A, McCamish MA, Burton PB (2004) Anemia and its relationship to clinical outcome in heart failure. Circulation 110:149–154. doi:10.1161/01.CIR.0000134279.79571.73
SOS-KANTO study group (2012) Relationship between the hemoglobin level at hospital arrival and post-cardiac arrest neurologic outcome. Am J Emerg Med 30:770–774. doi:10.1016/j.ajem.2011.03.031
Karimova A, Pinsky DJ (2001) The endothelial response to oxygen deprivation: biology and clinical implications. Intensive Care Med 27:19–31. doi:10.1007/s001340000790
Shoemaker WC, Appel PL, Kram HB (1992) Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest 102:208–215. doi:10.1378/chest.102.1.208
Shoemaker WC, Appel PL, Kram HB (1988) Tissue oxygen debt as a determinant of lethal and nonlethal postoperative organ failure. Crit Care Med 16:1117–1120. doi:10.1097/00003246-198811000-00007
Jacobs I, Nadkarni V, Bahr J et al (2004) Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 110:3385–3397. doi:10.1161/01.CIR.0000147236.85306.15
Report of a WHO Scientific Group (1968) World Health Organisation technical report ser. no. 405. World Health Organization, Geneva, pp 5–37
Edgren E, Hedstrand U, Kelsey S, Sutton-Tyrrell K, Safar P (1994) Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I Study Group. Lancet 343:1055–1059
Hamilton LC (1992) Regression with graphics: a second course in applied statistics. Duxbury Press, Belmont, pp 158–161
Corwin HL, Gettinger A, Rodriguez RM, Pearl RG, Gubler KD, Enny C, Colton T, Corwin MJ (1999) Efficacy of recombinant human erythropoietin in the critically ill patient: a randomized, double-blind, placebo-controlled trial. Crit Care Med 27:2346–2350. doi:10.1097/00003246-199911000-00004
Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG (2001) Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness. J Crit Care 16:36–41. doi:10.1053/jcrc.2001.21795
Thomas J, Jensen L, Nahirniak S, Gibney RT (2010) Anemia and blood transfusion practices in the critically ill: a prospective cohort review. Heart Lung 39:217–225. doi:10.1016/j.hrtlng.2009.07.002
Smoller BR, Kruskall MS (1986) Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med 314:1233–1235. doi:10.1056/NEJM198605083141906
Corwin HL, Krantz SB (2000) Anemia of the critically ill: “acute” anemia of chronic disease. Crit Care Med 28:3098–3099. doi:10.1097/00003246-200008000-00079
Grotta J, Ackerman R, Correia J, Fallick G, Chang J (1982) Whole blood viscosity parameters and cerebral blood flow. Stroke 13:296–301. doi:10.1161/01.STR.13.3.296
Kershenovich S, Modiano M, Ewy GA (1992) Markedly decreased coronary blood flow in secondary polycythemia. Am Heart J 123:521–523. doi:10.1016/0002-8703(92)90671-H
Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E, Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 340:409–417. doi:10.1056/NEJM199902113400601
Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, Holcomb JB, Illoh O, Kaplan LJ, Katz LM, Rao SV, Roback JD, Shander A, Tobian AA, Weinstein R, Swinton McLaughlin LG, Djulbegovic B, Clinical Transfusion Medicine Committee of the AABB (2012) Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med 157:49–58. doi:10.7326/0003-4819-157-1-201206190-00429
Johnston AJ, Steiner LA, Gupta AK, Menon DK (2003) Cerebral oxygen vasoreactivity and cerebral tissue oxygen reactivity. Br J Anaesth 90:774–786. doi:10.1093/bja/aeg104
Farquhar H, Weatherall M, Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Beasley R (2009) Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 158:371–377. doi:10.1016/j.ahj.2009.05.037
Zwemer CF, Whitesall SE, D’Alecy LG (1994) Cardiopulmonary-cerebral resuscitation with 100% oxygen exacerbates neurological dysfunction following nine minutes of normothermic cardiac arrest in dogs. Resuscitation 27:159–170. doi:10.1016/0300-9572(94)90009-4
Liu Y, Rosenthal RE, Haywood Y, Miljkovic-Lolic M, Vanderhoek JY, Fiskum G (1998) Normoxic ventilation after cardiac arrest reduces oxidation of brain lipids and improves neurological outcome. Stroke 29:1679–1686. doi:10.1161/01.STR.29.8.1679
Vereczki V, Martin E, Rosenthal RE, Hof PR, Hoffman GE, Fiskum G (2006) Normoxic resuscitation after cardiac arrest protects against hippocampal oxidative stress, metabolic dysfunction, and neuronal death. J Cereb Blood Flow Metab 26:821–835. doi:10.1038/sj.jcbfm.9600234
Richards EM, Fiskum G, Rosenthal RE, Hopkins I, McKenna MC (2007) Hyperoxic reperfusion after global ischemia decreases hippocampal energy metabolism. Stroke 38:1578–1584. doi:10.1161/STROKEAHA.106.473967
Wang CH, Chang WT, Huang CH, Tsai MS, Yu PH, Wang AY, Chen NC, Chen WJ (2014) The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and meta-analysis of observational studies. Resuscitation 85:1142–1148. doi:10.1016/j.resuscitation.2014.05.021
Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, Parrillo JE, Trzeciak S, Emergency Medicine Shock Research Network (EMShockNet) Investigators (2010) Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 303:2165–2171. doi:10.1001/jama.2010.707
Acknowledgments
We thank Center of Quality Management of National Taiwan University Hospital for providing the list of patients sustaining in-hospital cardiac arrest. This study was funded by the academic research Grant NTUHYL103.N003 from the National Taiwan University Hospital Yunlin Branch, which was not involved in the study design, in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This study was conducted in accordance with the amended Declaration of Helsinki. The Institutional Review Board of NTUH approved this study (reference number: 201410011RINA) and waived the requirement for written informed consent before data collection.
Informed consent
The Institutional Review Board of National Taiwan University Hospital approved this study and waived the requirement for written informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Fig 1
Generalized additive model plot for nonparametric modelling of the effect of PaO2 on the logit of probability for a favorable neurological outcome at hospital discharge. PaO2, arterial oxygen partial pressure (TIFF 23 kb)
Rights and permissions
About this article
Cite this article
Wang, CH., Huang, CH., Chang, WT. et al. Association between hemoglobin levels and clinical outcomes in adult patients after in-hospital cardiac arrest: a retrospective cohort study. Intern Emerg Med 11, 727–736 (2016). https://doi.org/10.1007/s11739-015-1386-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-015-1386-2