Abstract
Advanced imaging has become essential for recognition of clinically suspected early spondyloarthritis. This report summarizes recent progress towards a data-driven comprehensive definition of a positive sacroiliac joint MRI in axial spondyloarthritis, which incorporates contextual information provided by structural lesions alongside with active changes. A focus is on emerging limitations and challenges with increasing use of imaging in spondyloarthritis. We discuss the ongoing controversy as to whether sacroiliac joint MRI due to its superior reliability and ability to depict both structural and active lesions should be the preferred imaging modality in early disease over the traditional approach with pelvic radiographs. Another challenge is transferring the expanding knowledge about imaging evaluation in spondyloarthritis to the community of rheumatologists and radiologists. Advanced imaging modalities will not become the gold standard for diagnosis of spondyloarthritis, which remains a process of composite deduction based on complementary information obtained from clinical, laboratory, and imaging assessment.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Weber U, Lambert RGW, Østergaard M, Hodler J, Pedersen SJ, Maksymowych WP. The diagnostic utility of magnetic resonance imaging in spondylarthritis. An international multicenter evaluation of one hundred eighty-seven subjects. Arthritis Rheum. 2010;62:3048–58.
Althoff CE, Sieper J, Song IH, Haibel H, Weiss A, Diekhoff T, et al. Active inflammation and structural change in early active axial spondyloarthritis as detected by whole-body MRI. Ann Rheum Dis. 2013;72:967–73.
Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777–83.
Sepriano A, Landewé R, van der Heijde D, Sieper J, Akkoc N, Brandt J, et al. Predictive validity of the ASAS classification criteria for axial and peripheral spondyloarthritis after follow-up in the ASAS-cohort: a final analysis. Ann Rheum Dis. 2016;75:1034–42.
Rudwaleit M, Jurik AG, Hermann KGA, Landewé R, van der Heijde D, Baraliakos X, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI Group. Ann Rheum Dis. 2009;68:1520–7.
Deodhar A. Sacroiliac joint magnetic resonance imaging in the diagnosis of axial spondyloarthritis: “a tiny bit of white on two consecutive slices” may be objective, but not specific. Arthritis Rheum. 2016;68:775–8. This topical editorial reviews controversies in imaging of early SpA and recommends that the definition of a positive MRI in SpA should be highly specific and developed by a data-driven process.
Weber U, Maksymowych WP. Advances and challenges in spondyloarthritis imaging for diagnosis and assessment of disease. Curr Rheumatol Rep. 2013;15:345.
Arnbak B, Jurik AG, Hørslev-Petersen K, Hendricks O, Hermansen LT, Loft AG, et al. Associations between spondyloarthritis and MRI findings: a cross-sectional analysis of 1020 patients with persistent low back pain. Arthritis Rheum. 2016;68:892–900. In this Danish cohort study, 21% of 1020 consecutive young back pain patients showed SIJ BME meeting the ASAS definition of a positive MRI for SpA, 42% of whom had low grade BME.
Jaremko JL, Liu L, Winn NJ, Ellsworth JE, Lambert RGW. Diagnostic utility of magnetic resonance imaging and radiography in juvenile spondyloarthritis: evaluation of the sacroiliac joints in controls and affected subjects. J Rheumatol. 2014;41:963–70. This retrospective controlled cohort study in juvenile SpA showed high diagnostic utility of SIJ MRI and a prevalence of non-specific SIJ BME in 20% of the controls having a mean age of 15.1 years.
Prassopoulos PK, Faflia CP, Voloudaki AE, Gourtsoyiannis NC. Sacroiliac joints: anatomical variants on CT. J Comput Assist Tomogr. 1999;23:323–7.
Egund N, Jurik AG. Anatomy and histology of the sacroiliac joints. Semin Musculoskelet Radiol. 2014;18:332–40. This review describes the normal anatomy and histology of the SIJ to facilitate detection of the anatomical site of disease-specific lesions and of normal variants simulating disease.
Kellgren JH, Jeffrey MR. The epidemiology of chronic rheumatism. Volume 2: Atlas of Standard Radiographs of Arthritis. Oxford, UK: Blackwell Scientific Publications;1963:36–40.
Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27:361–8.
Weiss PF, Xiao R, Biko DM, Chauvin NA. Assessment of sacroiliitis at diagnosis of juvenile spondyloarthritis by radiography, magnetic resonance imaging, and clinical examination. Arthritis Care Res. 2016;68:187–94.
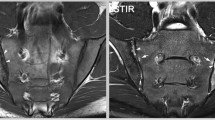
Weber U, Østergaard M, Lambert RGW, Pedersen SJ, Chan SM, Zubler V, et al. Candidate lesion-based criteria for defining a positive sacroiliac joint MRI in two cohorts of patients with axial spondyloarthritis. Ann Rheum Dis. 2015;74:1976–82. In this study in 2 independent SpA inception cohorts, lesion-based criteria for a positive SIJ MRI based on both BME and/or erosion performed best for classification of axial SpA, reflecting the contextual information provided by T1SE and STIR sequences.
De Hooge M, van den Berg R, Navarro-Compán V, Reijnierse M, van Gaalen F, Fagerli K, et al. Patients with chronic back pain of short duration from the SPACE cohort: which MRI structural lesions in the sacroiliac joints and inflammatory and structural lesions in the spine are most specific for axial spondyloarthritis? Ann Rheum Dis. 2016;75:1308–14. This report from a recent-onset back pain cohort focussed on diagnostic utility of structural SIJ lesions only. Patients were enrolled according to the ASAS definition of a positive SIJ MRI, which was available to the rheumatologist formulating the gold standard expert opinion as to the diagnosis of SpA. Control subjects had up to 2 SpA items from the ASAS classification criteria set.
Herregods N, Dehoorne J, Joos R, Jaremko JL, Baraliakos X, Leus A, et al. Diagnostic value of MRI features of sacroiliitis in juvenile spondyloarthritis. Clin Radiol. 2015;70:1428–38.
Weber U, Pedersen SJ, Zubler V, Rufibach K, Chan SM, Lambert RGW, et al. Fat infiltration on magnetic resonance imaging of the sacroiliac joints has limited diagnostic utility in nonradiographic axial spondyloarthritis. J Rheumatol. 2014;41:75–83.
Lambert RGW, Bakker PAC, van der Heijde D, Weber U, Rudwaleit M, Hermann KGA, et al. Defining active sacroiliitis on MRI for classification of axial spondyloarthritis: update by the ASAS MRI working group. Ann Rheum Dis. 2016. doi:10.1136/annrheumdis-2015-208642. This update on the definition of active sacroiliitis on MRI for classification of axial SpA incorporates the simultaneous assessment of MRI sequences designed to identify active and structural lesions taking into account the contextual information contained in both lesion types.
Weber U, Zubler V, Zhao Z, Lambert RGW, Chan SM, Pedersen SJ, et al. Does spinal MRI add incremental diagnostic value to MRI of the sacroiliac joints alone in patients with non-radiographic axial spondyloarthritis? Ann Rheum Dis. 2015;74:985–92. The combination of spine and SIJ MRI in 2 independent SpA inception cohorts added little incremental value compared with SIJ MRI alone for diagnosing patients with early axial SpA. Vertebral corner lesions were the main drivers towards misclassification.
Weber U, Zhao Z, Rufibach K, Zubler V, Lambert RGW, Chan SM, et al. Diagnostic utility of candidate definitions for demonstrating axial spondyloarthritis on magnetic resonance imaging of the spine. Arthritis Rheum. 2015;67:924–33. None of the previous candidate spinal thresholds for a positive spinal MRI in axial SpA showed clinically relevant diagnostic utility in 2 independent SpA inception cohorts.
Hermann KGA, Baraliakos X, van der Heijde DMFM, Jurik AG, Landewé R, Marzo-Ortega H, et al. Descriptions of spinal MR lesions and definition of a positive MRI of the spine in axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI study group. Ann Rheum Dis. 2012;71:1278–88.
Arnbak B, Jensen TS, Egund N, Zejden A, Hørslev-Petersen K, Manniche C, et al. Prevalence of degenerative and spondyloarthritis-related magnetic resonance imaging findings in the spine and sacroiliac joints in patients with persistent low back pain. Eur Radiol. 2016;26:1191–203.
De Bruin F, ter Horst S, Bloem HL, van den Berg R, de Hooge M, van Gaalen F, et al. Prevalence of degenerative changes of the spine on magnetic resonance images and radiographs in patients aged 16–45 years with chronic back pain of short duration in the Spondyloarthritis Caught Early (SPACE) cohort. Rheumatology. 2016;55:56–65.
Weber U, Pedersen SJ, Østergaard M, Rufibach K, Lambert RGW, Maksymowych WP. Can erosions on MRI of the sacroiliac joints be reliably detected in patients with ankylosing spondylitis—a cross-sectional study. Arthritis Res Ther. 2012;14:R124.
Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ. Development and preliminary validation of the spondyloarthritis research consortium of Canada magnetic resonance imaging sacroiliac joint structural score. J Rheumatol. 2015;42:79–86.
Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ. Fat metaplasia and backfill are key intermediaries in the development of sacroiliac joint ankylosis in patients with ankylosing spondylitis. Arthritis Rheum. 2014;66:2958–67. The findings in this prospective observational cohort of 147 AS patients support a disease model whereby ankylosis develops following repair of SIJ erosion with backfill as key intermediary step.
Pedersen SJ, Poddubnyy D, Sørensen IJ, Loft AG, Hindrup JS, Thamsborg G, et al. Course of magnetic resonance imaging-detected inflammation and structural lesions in the sacroiliac joints of patients in the randomized, double-blind, placebo-controlled Danish multicenter study of adalimumab in spondyloarthritis, as assessed by the Berlin and Spondyloarthritis Research Consortium of Canada methods. Arthritis Rheum. 2016;68:418–29. In this randomized controlled trial in axial SpA, treatment with a tumour necrosis factor inhibitor was associated with resolution of erosion and development of backfill.
Krohn M, Braum LS, Sieper J, Song IH, Weiss A, Callhoff J, et al. Erosions and fatty lesions of sacroiliac joints in patients with axial spondyloarthritis: evaluation of different MRI techniques and two scoring methods. J Rheumatol. 2014;41:473–80.
Weber U, Maksymowych WP, Chan SM, Rufibach K, Pedersen SJ, Zhao Z, et al. Does evaluation of the ligamentous compartment enhance diagnostic utility of sacroiliac joint MRI in axial spondyloarthritis? Arthritis Res Ther. 2015;17:246.
Jans L, van Praet L, Elewaut D, van den Bosch F, Carron P, Jaremko JL, et al. MRI of the SI joints commonly shows non-inflammatory disease in patients clinically suspected of sacroiliitis. Eur J Radiol. 2014;83:179–84.
Van Onna M, van Tubergen A, van der Heijde D, Jurik AG, Landewé R. Gadolinium contrast-enhanced MRI sequence does not have an incremental value in the assessment of sacroiliitis in patients with early inflammatory back pain by using MRI in combination with pelvic radiographs: a 2-year follow-up study. Clin Exp Rheumatol. 2014;32:225–30.
Weiss PF, Xiao R, Biko DM, Johnson AM, Chauvin NA. Detection of inflammatory sacroiliitis in children with magnetic resonance imaging. Is gadolinium contrast enhancement necessary? Arthritis Rheum. 2015;67:2250–6.
Herregods N, Jaremko JL, Baraliakos X, Dehoorne J, Leus A, Verstraete K, et al. Limited role of gadolinium to detect active sacroiliitis on MRI in juvenile spondyloarthritis. Skeletal Radiol. 2015;44:1637–46.
Jarrett SJ, Sivera F, Cawkwell LS, Marzo-Ortega H, McGonagle D, Hensor E, et al. MRI and clinical findings in patients with ankylosing spondylitis eligible for anti-tumour necrosis factor therapy after a short course of etoricoxib. Ann Rheum Dis. 2009;68:1466–9.
Varkas G, Jans L, Cypers H, van Praet L, Carron P, Elewaut D, et al. Six-week treatment of axial spondyloarthritis patients with an optimal dose of nonsteroidal antiinflammatory drugs: early response to treatment in signal intensity on magnetic resonance imaging of the sacroiliac joints. Arthritis Rheum. 2016;68:672–8.
Bedaiwi MK, Sari I, Wallis D, O'Shea FD, Salonen D, Haroon N, et al. Clinical efficacy of celecoxib compared to acetaminophen in chronic nonspecific low back pain: results of a randomized controlled trial. Arthritis Care Res. 2016;68:845–52.
Mandl P, Navarro-Compán V, Terslev L, Aegerter P, van der Heijde D, D’Agostino MA, et al. EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice. Ann Rheum Dis. 2015;74:1327–39. A set of 10 evidence-based recommendations on the use of imaging in the clinical management of axial and peripheral SpA was developed by systematic literature review and expert consensus.
Sudol-Szopińska I, Jurik AG, Eshed I, Lennart J, Grainger A, Østergaard M, et al. Recommendations of the ESSR arthritis subcommittee for the use of magnetic resonance imaging in musculoskeletal rheumatic diseases. Semin Musculoskelet Radiol. 2015;19:396–411.
Christiansen AA, Hendricks O, Kuettel D, Hørslev-Petersen K, Jurik AG, Nielsen S, et al. Evaluation of sacroiliac joint radiographs in patients with chronic low back pain: is erosion the main driver of interreader disagreement? Arthritis Rheum. 2015;67:S3852 [abstract 3210].
U.S. Food and Drug Administration, Department of Health & Human Services. Arthritis Advisory Committee Meeting: Adalimumab (Humira®) for active non-radiographic axial spondyloarthritis (nr-axSpA) in adults with objective signs of inflammation by elevated CRP or MRI, who have had inadequate response or are intolerant to NSAIDs; July 23, 2013; Available from: www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM361563.pdf.
U.S. Food and Drug Administration, Department of Health & Human Services. Arthritis Advisory Committee Meeting: Certolizumab (Cimzia®) for active axial spondyloarthritis, including ankylosing spondylitis; July 23, 2013; Available from: www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM361565.pdf.
Deodhar A, Reveille JD, van den Bosch F, Braun J, Burgos-Vargas R, Caplan L, et al. The concept of axial spondyloarthritis: joint statement of the spondyloarthritis research and treatment network and the Assessment of SpondyloArthritis international Society in response to the US Food and Drug Administration’s comments and concerns. Arthritis Rheum. 2014;66:2649–56.
Van den Berg R, Lenczner G, Feydy A, van der Heijde D, Reijnierse M, Saraux A, et al. Agreement between clinical practice and trained central reading in reading of sacroiliac joints on plain pelvic radiographs. Results from the DESIR cohort. Arthritis Rheum. 2014;66:2403–11. This report in a SpA inception cohort demonstrated only moderate agreement (kappa 0.54) of radiographic SIJ evaluation by central readers raising concerns about reliability of radiographic modified NYc in suspected early SpA.
Van den Berg R, Lenczner G, Thévenin F, Claudepierre P, Feydy A, Reijnierse M, et al. Classification of axial SpA based on positive imaging (radiographs and/or MRI of the sacroiliac joints) by local rheumatologists or radiologists versus central trained readers in the DESIR cohort. Ann Rheum Dis. 2015;74:2016–21. Assessment of SIJ MRI in the same SpA inception cohort as above showed substantial agreement among central readers (kappa 0.73) for the ASAS definition of a positive MRI based on active inflammatory lesions.
Spoorenberg A, de Vlam K, van der Linden S, Dougados M, Mielants H, van de Tempel H, et al. Radiological scoring methods in ankylosing spondylitis. Reliability and change over 1 and 2 years. J Rheumatol. 2004;31:125–32.
Dougados M, Demattei C, van den Berg R, Vo Hoang V, Thevenin F, Reijnierse M, et al. Rate and predisposing factors of sacroiliac radiographic progression after a 2 years follow-up period in recent onset spondyloarthritis. Arthritis Rheum. 2016. doi:10.1002/art.39666. Blinded evaluation of sacroiliac radiographic progression in early SpA over 2 years showed progression from modified NYc negative to positive in 4.9%, but vice versa also regression in 5.7% switching back from positive to negative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
UW, AGJ, RGWL, and WPM declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Spondyloarthritis
Rights and permissions
About this article
Cite this article
Weber, U., Jurik, A.G., Lambert, R.G.W. et al. Imaging in Spondyloarthritis: Controversies in Recognition of Early Disease. Curr Rheumatol Rep 18, 58 (2016). https://doi.org/10.1007/s11926-016-0607-7
Published:
DOI: https://doi.org/10.1007/s11926-016-0607-7